Assessing phrenic nerve function in the setting of diaphragmatic paralysis in diaphragm pacing candidates can be challenging. Traditional imaging modalities and electrodiagnostic evaluations are technically difficult. Either modality alone is not a direct measure of the function of the phrenic nerve and diaphragm unit. In this article, the authors present their method for evaluating phrenic nerve function and the resulting diaphragm function. Stimulating the phrenic nerve with transcutaneous stimulation and directly observing the resulting movement of the hemidiaphragm with M-mode ultrasonography provides quantitative data for predicting the success of advancing technologies such as phrenic nerve pacing and diaphragm pacing.
Key points
- •
Combining phrenic nerve stimulation with observation of the movement of the hemidiaphragm with M-mode ultrasonography provides quantitative functional data in the setting of diaphragm paralysis.
- •
Traditional phrenic motor nerve conduction studies such as electromyography of the diaphragm have limitations in predicting the success of phrenic nerve or diaphragm pacing.
- •
Phrenic nerve pacing is an effective form of respiratory management in pediatric high cervical spinal cord injury.
- •
Successful phrenic nerve pacing in pediatric high cervical spinal cord injury can be accomplished with only one intact phrenic nerve and hemidiaphragm.
- •
Successful phrenic nerve pacing in pediatric high cervical spinal cord injury can be accomplished several years after the initial injury.
Introduction: nature of the problem
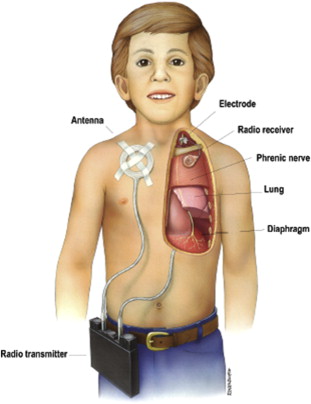
A phrenic nerve pacing system consists of implanted receivers and electrodes, external antennas worn directly over the implanted receivers, and an external transmitter. The external transmitter and antennas send energy to the implanted receivers. The electrical stimulation is accomplished by transcutaneous radiofrequency stimulation of the implanted receivers by the external antennas. The implanted receivers receive the radiofrequency energy and convert it to electrical impulses, which directly stimulate the phrenic nerves. The phrenic nerve stimulation leads to contraction of the diaphragms ( Fig. 1 ).
Electric stimulation of the phrenic nerve was first applied by Sarnoff and colleagues in 1948 in the setting of ventilatory insufficiency. Glenn and colleagues electrically stimulated the phrenic nerve through radiofrequency induction and successfully applied the technique clinically. Onders and colleagues described a method of directly stimulating the diaphragm to achieve successful ventilation. Diaphragm pacing via phrenic nerve stimulation requires an intact phrenic nerve and a functioning diaphragm. Patients with primary neuropathies and myopathies are generally not good candidates for this therapy. In pediatric centers, diaphragm pacing has been most commonly used for patients with high cervical spinal cord injury and for those with central hypoventilation syndromes such as congenital central hypoventilation syndrome. Successful application of these techniques for patients with spinal cord injury requires careful evaluation of phrenic nerve and diaphragmatic function.
Fluoroscopy is used in many institutions to evaluate diaphragmatic motion in the setting of presumed diaphragmatic paralysis. Fluoroscopy is limited by the use of ionizing radiation and the requirement for patient transport to a specialized examination or surgical suite. In addition, fluoroscopy provides qualitative images but cannot provide quantitative data regarding diaphragmatic motion.
Electrodiagnostic motor nerve conduction studies (mNCS) and electromyography (EMG) are conventionally used to evaluate the function and integrity of the phrenic nerve in the setting of diaphragmatic paralysis, but these methods possess several disadvantages. Phrenic nerve mNCS can be technically difficult to perform because of patients’ body habitus and confounding electrical interference. These factors can be especially limiting for a ventilated patient in an intensive care unit. In addition, mNCS only provide data regarding the phrenic nerve and corresponding diaphragmatic muscle action potentials, which serve as surrogate markers of phrenic nerve and diaphragmatic function. Phrenic nerve mNCS can be useful for detecting and quantifying the injury to the phrenic nerve, but the reliability and reproducibility are suboptimal. Although mNCS have been used to determine eligibility for phrenic nerve and diaphragm pacing systems, they offer no direct measurement of diaphragmatic response to phrenic nerve stimulation.
Performing EMG on the diaphragm can be daunting for an inexperienced electromyographer, owing to the small risk for pneumothorax. Similarly to fluoroscopy, EMG of the diaphragm provides only qualitative data regarding spontaneous activity and motor unit recruitment. In the setting of partial axonotmesis, EMG is not able to assess for the presence of adequate axonal function to achieve sufficient stimulation of the diaphragm and attain adequate ventilation with phrenic nerve stimulation.
This report details one center’s protocol for the assessment of diaphragmatic response to phrenic nerve stimulation. The technique provides information regarding the integrity of the phrenic nerve, anatomic etiology of diaphragmatic paralysis, and the potential for phrenic nerve pacing through transcutaneous stimulation of the phrenic nerve and direct visualization of the resulting diaphragmatic movement with ultrasonography. In addition to the initial evaluation for candidacy for phrenic nerve or diaphragmatic pacing systems, the utility of the technique for long-term follow-up and settings adjustments of the pacing systems are reviewed.
Introduction: nature of the problem
A phrenic nerve pacing system consists of implanted receivers and electrodes, external antennas worn directly over the implanted receivers, and an external transmitter. The external transmitter and antennas send energy to the implanted receivers. The electrical stimulation is accomplished by transcutaneous radiofrequency stimulation of the implanted receivers by the external antennas. The implanted receivers receive the radiofrequency energy and convert it to electrical impulses, which directly stimulate the phrenic nerves. The phrenic nerve stimulation leads to contraction of the diaphragms ( Fig. 1 ).
Electric stimulation of the phrenic nerve was first applied by Sarnoff and colleagues in 1948 in the setting of ventilatory insufficiency. Glenn and colleagues electrically stimulated the phrenic nerve through radiofrequency induction and successfully applied the technique clinically. Onders and colleagues described a method of directly stimulating the diaphragm to achieve successful ventilation. Diaphragm pacing via phrenic nerve stimulation requires an intact phrenic nerve and a functioning diaphragm. Patients with primary neuropathies and myopathies are generally not good candidates for this therapy. In pediatric centers, diaphragm pacing has been most commonly used for patients with high cervical spinal cord injury and for those with central hypoventilation syndromes such as congenital central hypoventilation syndrome. Successful application of these techniques for patients with spinal cord injury requires careful evaluation of phrenic nerve and diaphragmatic function.
Fluoroscopy is used in many institutions to evaluate diaphragmatic motion in the setting of presumed diaphragmatic paralysis. Fluoroscopy is limited by the use of ionizing radiation and the requirement for patient transport to a specialized examination or surgical suite. In addition, fluoroscopy provides qualitative images but cannot provide quantitative data regarding diaphragmatic motion.
Electrodiagnostic motor nerve conduction studies (mNCS) and electromyography (EMG) are conventionally used to evaluate the function and integrity of the phrenic nerve in the setting of diaphragmatic paralysis, but these methods possess several disadvantages. Phrenic nerve mNCS can be technically difficult to perform because of patients’ body habitus and confounding electrical interference. These factors can be especially limiting for a ventilated patient in an intensive care unit. In addition, mNCS only provide data regarding the phrenic nerve and corresponding diaphragmatic muscle action potentials, which serve as surrogate markers of phrenic nerve and diaphragmatic function. Phrenic nerve mNCS can be useful for detecting and quantifying the injury to the phrenic nerve, but the reliability and reproducibility are suboptimal. Although mNCS have been used to determine eligibility for phrenic nerve and diaphragm pacing systems, they offer no direct measurement of diaphragmatic response to phrenic nerve stimulation.
Performing EMG on the diaphragm can be daunting for an inexperienced electromyographer, owing to the small risk for pneumothorax. Similarly to fluoroscopy, EMG of the diaphragm provides only qualitative data regarding spontaneous activity and motor unit recruitment. In the setting of partial axonotmesis, EMG is not able to assess for the presence of adequate axonal function to achieve sufficient stimulation of the diaphragm and attain adequate ventilation with phrenic nerve stimulation.
This report details one center’s protocol for the assessment of diaphragmatic response to phrenic nerve stimulation. The technique provides information regarding the integrity of the phrenic nerve, anatomic etiology of diaphragmatic paralysis, and the potential for phrenic nerve pacing through transcutaneous stimulation of the phrenic nerve and direct visualization of the resulting diaphragmatic movement with ultrasonography. In addition to the initial evaluation for candidacy for phrenic nerve or diaphragmatic pacing systems, the utility of the technique for long-term follow-up and settings adjustments of the pacing systems are reviewed.
Description of technique
Diaphragmatic Ultrasonography
Diaphragmatic ultrasonography is performed with the patient in the supine position. For the older pediatric and adult patient, a multifrequency 4-MHz vector transducer is used in the longitudinal semicoronal plane using a subcostal or low intercostal approach extending from the midaxillary to the midclavicular lines. In young pediatric patients, a multifrequency 7-MHz vector transducer is used from the same approach. The right diaphragm is visualized through the window of the liver, and the left diaphragm is visualized though the window of the spleen.
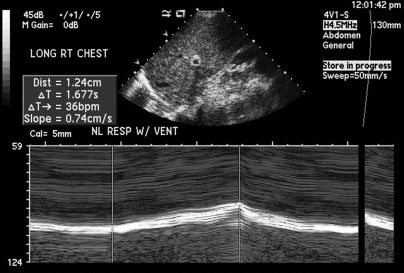
Diaphragmatic ultrasonography provides direct visualization of the diaphragm, qualitative evaluation of diaphragmatic excursion, and quantitative evaluation of diaphragmatic motion with M-mode ultrasonography. M-mode sonography allows for quantification of diaphragmatic motion by recording the successive positions of the diaphragm in relation to time. Patients are initially examined with and without mechanically assisted ventilation ( Figs. 2 and 3 ). The ventilator is temporarily disconnected when the patient undergoes phrenic nerve stimulation.