Abstract
Background
When the subject is not able to satisfy traditional testing procedures, alternative exercises or indices such as arm cranking or the oxygen uptake efficiency slope (OUES) have been proposed. However, the OUES has not yet been used on elderly subjects from an exercise performed with the arms.
Objective
The aim of our study was to evaluate the possibility of using the OUES as an index of the cardiorespiratory functional reserve in the elderly when the exercise evaluation test is performed with the arms and when this parameter is estimated from submaximal responses.
Methods
Seventeen adults (62–82 years) undergoing total joint arthroplasty of the hip took part in this study. Maximal incremental exercise tests were performed on an arm crank ergometer 1 month before (T 1 ) and 2 months after (T 2 ) surgery. Gas exchanges were measured continuously to determine oxygen consumption at peak exercise ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak) and were used to calculate the OUES.
The correlation coefficient was calculated between <SPAN role=presentation tabIndex=0 id=MathJax-Element-2-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak and OUES, and their relative changes between T 1 and T 2 .
Results
<SPAN role=presentation tabIndex=0 id=MathJax-Element-3-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak was not significantly different between T 1 and T 2 : 10.3 ± 0.7 and 9.8 ± 0.5 mL/min per kilogramme respectively. The OUES estimated from submaximal responses did not show a significant difference between T 1 and T 2 . Significant correlations were observed between individual <SPAN role=presentation tabIndex=0 id=MathJax-Element-4-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak and OUES, as well as at T 1 and T 2 .
Conclusion
The use of arm cranking exercises and the calculation of the OUES from the submaximal respiratory response can be used for the objective quantification of cardiorespiratory functional reserve in the elderly.
Résumé
Rationnel
Lorsqu’un sujet n’est pas capable d’effectuer correctement les procédures habituelles de test, des exercices alternatifs (pédalage avec les membres supérieurs) ou des indices tels que l’indice d’efficacité cardiorespiratore oxygen uptake efficiency slope (OUES) ont été proposés. Pourtant, l’OUES n’a pas encore été utilisé chez des sujets âgés lorsque l’exercice est effectué avec les bras.
Objectif
Le but de notre étude était d’évaluer la possibilité d’utiliser l’OUES comme un indice de la réserve fonctionnelle cardiorespiratoire chez des personnes âgées lorsque l’exercice utilisé pour l’évaluation est effectué avec les bras et lorsque ce paramètre est calculé à partir d’une réponse sous-maximale.
Méthode
Dix-sept adultes (62–82 ans) subissant une arthroplastie totale de la hanche ont participé à cette étude. Un exercice maximal incrémental a été effectuée avec un ergomètre à bras un mois avant (T 1 ) et deux mois après (T 2 ) la chirurgie. Les échanges gazeux ont été mesurées continuellement pour déterminer la consommation pic d’oxygène ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-5-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
pic) et ont été utilisés pour calculer OUES. Le coefficient de corrélation entre <SPAN role=presentation tabIndex=0 id=MathJax-Element-6-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
pic et OUES a été calculé.
Résultats
<SPAN role=presentation tabIndex=0 id=MathJax-Element-7-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak n’était pas significativement différent entre T 1 et T 2 : 10,3 ± 0,7 et 9,8 ± 0,5 mL/min par kilogramme, respectivement. OUES estimée à partir des réponses sous-maximales n’était pas significativement différent entre T 1 et T 2 . Des corrélations significatives ont été observées entre <SPAN role=presentation tabIndex=0 id=MathJax-Element-8-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak et OUES, aussi bien à T 1 qu’à T 2 .
Conclusion
Les exercices effectués avec les bras et le calcul d’OUES à partir des réponses respiratoires lors d’exercices sous-maximaux peuvent être utilisés avec un objectif de quantification de la réserve fonctionnelle cardiorespiratoire chez les personnes âgées.
1
English version
1.1
Introduction
Exercise stress testing is frequently used in the preoperative evaluation of patients with known or suspected ischemic heart disease to evaluate their physical capacities . This is usually done through a graded exercise test that provides an accurate and objective expression of exercise capacity. Out of all modes of exercise, the most popular are cycling and running and the most frequently used current indices of exercise capacity are peak or maximal oxygen uptake and ventilatory threshold (VT) (respectively <SPAN role=presentation tabIndex=0 id=MathJax-Element-9-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak, <SPAN role=presentation tabIndex=0 id=MathJax-Element-10-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
max, VT), or other indices calculated from the variables measures during the exercise test (e.g., extrapolated <SPAN role=presentation tabIndex=0 id=MathJax-Element-11-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
max or <SPAN role=presentation tabIndex=0 id=MathJax-Element-12-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E-V˙O2′>V˙E-V˙O2V˙E-V˙O2
V ˙ E- V ˙ O 2
slope) .
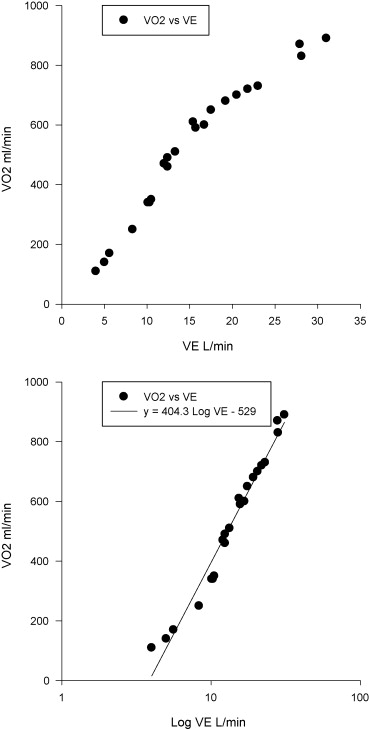
Baba and co-workers proposed another such single index: the oxygen uptake efficiency slope (OUES). This index is derived from the logarithmic relationship between oxygen consumption ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-13-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
) and minute ventilation ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-14-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E’>V˙EV˙E
V ˙ E
) during incremental exercise. In a wide panel of subjects (healthy people , male or female, children and adolescent cardiac patients ), this index appears to be an objective and reproducible measure of exercise capacity, and may also be easier than <SPAN role=presentation tabIndex=0 id=MathJax-Element-15-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
max or VT determination . Moreover, with the OUES, it is possible to consider only the submaximal response (75 or 90% and of the exercise duration) to estimate the cardiorespiratory functional reserve .
All these advantages should be particularly important when elderly are concerned. It is recognized that the evaluation of aerobic capacity through exercise stress testing is very important to evaluate their cardiovascular functional reserve, but additional information from which functional capacity can be derived and additional tools able to provide this data are needed . Indeed, treadmill or bicycle tests have been shown to screen elderly individuals adequately, but the choice of these exercise modes may be compromised by lower limb impairments, claudication, amputation or debilitating arthritis of the joint(s). In addition, maximal exercise performance is potentially dependent on patient motivation , and in order to preserve the patient’s health, the exercise may be stopped before maximal performance in the event of symptoms of breathlessness, ECG changes or an undue rise in blood pressure. Such limitations render difficult the realization of the standard procedures (exercise testing performed on treadmill or cycle-ergometer) and impossible the assessment of the standard parameters (i.e. <SPAN role=presentation tabIndex=0 id=MathJax-Element-16-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak, <SPAN role=presentation tabIndex=0 id=MathJax-Element-17-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
max) used to evaluate physical fitness.
With old subjects suffering from lower limb impairments, the use of alternative testing modes such as symptom-limited arm ergometer testing and OUES calculated from submaximal responses seem pertinent. However, to the best of our knowledge, the OUES has not yet been derived from a test performed with the arms.
Thus, the aim of our study was to evaluate the possibility of using the OUES as an index of the cardiorespiratory functional reserve in the elderly when the exercise evaluation test is performed with the arms and when this parameter is estimated from a submaximal response.
1.2
Methods
1.2.1
Participants
Seventeen older adults (15 males/two females mean age: 74.03 S.D. 1.18 years, 66–82, range; maximal theoretical heart rate (HR) (208–0.7 times age) equal to 156.9 ± 0.8 bpm undergoing total joint arthroplasty of the hip participated in this study. They were unable to perform a standard exercise test with the lower limbs, neither before surgery because of pain, nor after surgery because of the risk of hip luxation. Participants were recruited by their surgeon during a presurgery visit. All subjects were unmedicated and none presented with cardiovascular disease, cerebrovascular disease or upper limb musculoskeletal impairment and were otherwise medically able to complete a full exercise test safely. The Local Ethics Committee approved the investigation, and all volunteers signed an informed consent form.
1.2.2
Testing
During the presurgery visit with the surgeon (1 month before surgery: T 1 ) and 2 months after surgery (T 2 ), each patient performed a maximal graded test under the supervision of a cardiologist. The second visit was performed after 6 weeks of a traditional rehabilitation program, which consisted of exercises for muscular strength, range of motion, aquatics and walking for two hours per day. Two exercise stress testing were used not to verify the reproducibility of the OUES (the conditions were not the same before and after hip replacement) but to assess whether any change in their physical capacity would be observed with OUES, either decreasing (due to the surgery) or increasing (due to the rehabilitation).
The arm crank ergometer (Monark Rehab Trainer, Model 881E, Monark Exercise, Sweden) used was calibrated before and after each test. After an initial warm-up period of three minutes, exercise began at a power output of 10W for two minutes, followed by 10W increments every two minutes, until the subject was unable to continue . The subject was encouraged to maintain a pedaling rate of 60 rpm . The results were taken into account only if at least two of the following three criteria had been met:
- •
a drop in arm cranking cadence below 50 rpm despite encouragement;
- •
a respiratory exchange ratio value exceeding 1.0;
- •
attainment of 80% of age predicted maximal HR (208–0.7 times age) .
A pulmonary assessment was performed with a portable metabolic measurement system cart (Aerosport KB1-C, Aerosport Inc. Ann Arbor, Michigan, USA, validated by King et al.) . Ventilation volumes were calculated using a flat-plate orifice within an open pneumotachometer. The KB1-C was calibrated immediately prior to each test in the low-flow position according to the manufacturer’s specifications using a 3-L calibrated syringe (Hans-Rudolph Inc., Kansas city, MO, USA). Expiratory gases were sampled and analysed during each 20 s period. The outcome variables were the rate of oxygen consumption ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-18-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
, mL/min per kilogramme), rate of carbon dioxide production ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-19-Frame class=MathJax style="POSITION: relative" data-mathml='V˙CO2′>V˙CO2V˙CO2
V ˙ CO 2
, mL/min per kilogramme), respiratory exchange ratio and ventilation per minute ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-20-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E’>V˙EV˙E
V ˙ E
, L/min). HR (bpm) was continuously monitored (Multichannel ECGs, Nihon Kodhen, type 2R-701.VK) during all tests. The maximal tolerated power (W) (the highest load which could be maintained with a constant pedaling speed for one minute) was registered during maximal graded tests.
1.2.3
Data analysis and statistics
The OUES was calculated according to the methodology reported by Baba et al. . The <SPAN role=presentation tabIndex=0 id=MathJax-Element-21-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E-V˙O2′>V˙E-V˙O2V˙E-V˙O2
V ˙ E- V ˙ O 2
slope was described by a single exponential function, using the following equation:
V ˙ O 2 = a log 10 V ˙ E + b
V ˙ O 2
is plotted on the y -axis and <SPAN role=presentation tabIndex=0 id=MathJax-Element-24-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E’>V˙EV˙E
V ˙ E
is plotted on the semilog transformed x -axis, the slope of this linear relationship, “a”, represents the OUES. Typical curves obtained from one subject are presented ( Fig. 1 ). The OUES was calculated twice, first using the responses registered until HR reached 80% of the maximal predicted HR (208–0.7 times age) ) which in our population corresponds to 125 (± 0.6) bpm and second using the responses registered during the overall exercise duration; these two indexes were named OUES 80 and OUES 100 respectively. In order to see whether these methods of calculation may influence the OUES’s values, a t test for paired samples was used to compare OUES 100 and OUES 80 calculated before and after surgery.
The comparison of the <SPAN role=presentation tabIndex=0 id=MathJax-Element-25-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak, OUES 100 and OUES 80 between T 1 and T 2 was performed using a t test for paired samples. The Pearson product moment correlation coefficient was calculated between <SPAN role=presentation tabIndex=0 id=MathJax-Element-26-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2
V ˙ O 2
peak, OUES 100 and OUES 80 respectively. The normality of the data distribution was verified by the Kolmogorov-Smirnov test. Agreement between OUES 100 and OUES 80 was evaluated thanks to the Bland and Altman method. All data are presented as means ± standard deviations (S.D.) unless otherwise specified. Statistical significance was set at P < 0.05 (SigmaStat, SPSS, Illinois, USA).
1.3
Results
Compliance with the exercise protocols was excellent. There were no test-related injuries. There was no difference between mass and height measured before and after surgery: mass = 71.1 kg (45.2–97, range), height = 159.5 cm (145.5–179) and mass = 70.3 kg (44–95.4), height = 159.8 cm (147–178).
The results obtained from the maximal progressive test at T 1 and T 2 are summarized in Table 1 . There was no significant difference between the parameters considered before and after surgery. There was no significant difference between OUES 100 and OUES 80 calculated before or after surgery. The limits of agreement between OUES 80 and OUES 100 estimated by the Bland-Altman method correspond to −60.4 and 86.1 respectively for the lower and upper limit.
| T 1 | T 2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <SPAN role=presentation tabIndex=0 id=MathJax-Element-27-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2 V ˙ O 2 | <SPAN role=presentation tabIndex=0 id=MathJax-Element-28-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E’>V˙EV˙E V ˙ E | HR | OUES 80 | OUES 100 | <SPAN role=presentation tabIndex=0 id=MathJax-Element-29-Frame class=MathJax style="POSITION: relative" data-mathml='V˙O2′>V˙O2V˙O2 V ˙ O 2 | <SPAN role=presentation tabIndex=0 id=MathJax-Element-30-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E’>V˙EV˙E V ˙ E | HR | OUES 80 | OUES 100 | |
| n = 19 | 10.3 ± 0.7 | 24.0 ± 1.6 | 135.5 ± 2.3 | 377.4 ± 24.2 | 388.4 ± 22.2 | 9.8 ± 0.5 | 24.0 ± 1.0 | 132.3 ± 2.8 | 388.44 ± 22.29 | 404.2 ± 20.8 |
V ˙ O 2
, mL/min per kilogram), minute ventilation ( <SPAN role=presentation tabIndex=0 id=MathJax-Element-32-Frame class=MathJax style="POSITION: relative" data-mathml='V˙E’>V˙EV˙E
V ˙ E
, L/min), heart rate (HR, bpm) at the peak exercise and oxygen uptake efficiency slope values at 100% (OUES 100 ) of incremental exercise duration and when submaximal responses until 80% (OUES 80 ) of maximal heart rate (220-0.7 age) are considered before (T 1 ) and after (T 2 ) surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







