Abstract
Objectives
To evaluate the effectiveness of a multidisciplinary consultation of diabetic foot in terms of ulcer healing rate and podiatric complications prevention.
Methods
A longitudinal observational study was conducted on 78 patients consulting multidisciplinary clinic of diabetic foot between the 1st January 2005 and the 31th December 2006. There were two evaluations: the first one in June 2008, the second one in January 2010, at a medium follow-up of 48 months.
Results
30.8% of diabetic patients were addressed in primary prevention, 53.8% for treatment of foot ulcer, and 15.4% in secondary prevention. The global healing rate was 76.19% after a medium follow-up of 29 months, and the recurrence rate at a medium follow-up of 48 months was 9.52%. Healing was achieved in 63.6% of patients with off-loading shoes versus 81.8% of whom with fiberglass cast boot.
Conclusion
Care and follow-up of diabetic patients with foot at risk in multidisciplinary consultation seem to be effective not only in curative treatment, but also in primary and secondary prevention. The economic benefits need to be evaluated.
Résumé
Introduction
L’ulcération du pied chez un sujet diabétique est la première cause d’amputation en France.
Objectifs
Évaluer les résultats d’une consultation multidisciplinaire du pied diabétique en termes de cicatrisation des lésions pour le traitement curatif, et d’absence de complication podologique pour le traitement préventif.
Patients et méthodes
Suivi longitudinal de cohorte mené sur l’ensemble des patients vus en consultation entre le 1 er janvier 2005 et le 31 décembre 2006, soit 78 patients. L’étude a comporté deux évaluations, l’une rétrospective réalisée en juin 2008 et l’autre prospective en janvier 2010, soit au bout d’une durée moyenne de 48 mois.
Résultats
Sur cette population de 78 diabétiques, 30,8 % ont été adressés en prévention primaire, 53,8 % pour une ulcération du pied, et 15,4 %, en prévention secondaire. Au final, le taux de cicatrisation global a été de 76,19 % après une durée moyenne de suivi de 29 mois, avec un bon maintien dans le temps puisque le taux de récidive était de 9,52 % au bout d’un suivi moyen de 48 mois. Le taux de guérison a été de 63,6 % avec une chaussure de décharge contre 81,8 % avec botte plâtrée ou en résine.
Conclusion
La prise en charge au sein d’une consultation multidisciplinaire des patients présentant un pied à risque diabétique semble efficace en termes de traitement curatif ainsi qu’en termes de prévention primaire et secondaire. Les bénéfices économiques restent à évaluer.
1
English version
1.1
Introduction
In the diabetic population, podiatric complications are numerous, serious and remain too frequent in France. At least 15% of diabetic patients will present a foot ulcer during their life . Foot ulcer in diabetic patients is the first cause of amputation in France. The annual amputations incidence in diabetic population is 200 to 800 for 100,000, the prevalence is estimated at 1,3%. Amputations are precessed by ulcer in 50 to 70% of cases. The amputation risk is 10 to 30 times higher than general population. Ulcer can multiply by 2 to10 the amputation risk and by 2.4 the risk of death compared to diabetic population without podiatric lesion. The 3-years survey rate is 72% for patients with ulcer versus 87% in control diabetic population. Ulcer recurs in 70% of cases within 5 years . After amputation, survey at 5 years is 58%, and another one amputation is necessary in 50% at years. Ulcer incidence may vary according to age, male sex, economic conditions and care access.
Thus, it is fundamental to develop the primary prevention, an optimal curative treatment, and an attentive follow-up of diabetic patients . Since 1989, the Saint Vincent Declaration sets up a 5-year target of decreasing by 40% the leg amputation rate in diabetic patients. In France, the Haute Autorité de santé published in May 2006 recommendations for management of diabetic patients, and defined a guideline for screening and prevention of the podiatric risk.
In a medico-economic point of view, podiatric lesions cause 10 to 20% of hospitalisation days for diabetes . The hospitalisation cost varies between 9000 and 35,000 euros. Diabetes is responsible of five to 10,000 amputations per year, which represents a direct cost of 76 to 150 millions euros. In 2003 was performed the first evaluation of the treatment cost of podiatric ulcer in diabetic patients. Medium monthly costs per patient were 697 euros for the ambulatory treatment, 15,556,20 euros for hospitalisations and 34,76 euros for stoppage of work. In cases of hospitalisation, hospitalisation represented about 70% of the medium podiatric ulcer cost. The ambulatory cost mainly consisted in expenses in medical and paramedical cares and for a lower proportion (10%) in medicinal treatments. The clinic predictive factors of higher cost of treatment were the recentness and the initial severity of the lesion. In logic association with clinical factors, amputation and specialized medical follow-up generated higher treatment costs. For the authorities, these economic results confirmed the interest of a precocious care for diabetic podiatric complications.
In Limoges, a multidisciplinary consultation of diabetic foot is functioning since April 2004. The consultation’s objectives are a not also diagnosis and multidisciplinary treatment of foot lesions in diabetic patients, but also primary and secondary prevention, information, and education. Moreover, it responds at an epidemiologic role.
The aim of our study was to evaluate the consultation’s results, in terms of healing of foot ulcer, and absence of complication in case of prevention.
1.2
Patients and methods
1.2.1
Research design
We conducted a longitudinal observational study by including all diabetic patients referred, one time at least, to the multidisciplinary consultation, between the first January 2005 and the 31th December 2006: there were 78 patients. We performed two evaluations: the first one, retrospectively, in June 2008 (medium follow-up of 29 months), and the second one, prospectively, in January 2010 (medium follow-up of 48 months).
1.2.2
Diagnostic criteria
Ulcers were considered as healed when completely cured. Recurrences were defined as apparition of a new lesion after a complete cicatrization. Primary as well as secondary prevention were considered as efficacy when no podiatric complication occurs.
1.2.3
Clinical features
Sex, age, address, referring doctor’s speciality, consultation’s motive, presence of ulceration, diabetes type were reported. Association with neuropathy, arteriopathy or nephropathy was also noticed.
We considered that patients were in primary prevention when they had no amputation or ulcer history. In case of ulcer, we pointed out the presence or not of osteitis. During the consultation, osteitis diagnosis was based essentially on clinical arguments (local inflammation and bone contact), and bone X-rays. About fitting, we enquired if patients had ever worn anyone beforehand, and its type. Then we distinguished the different type of protection from weight bearing, which have been prescribed: off-loading shoes, plantar orthesis, fiberglass cast boot, total off-loading by hospitalisation. Moreover, we reported all cases of surgical treatment, their number and nature. Toe and transmetatarsal amputations were considered as minor amputation, amputations realized above were considered as major. Lastly, we censored all patients who required a hospitalisation and got the mean length of stay.
In term of clinical of clinical evolution, we set apart cicatrization cases, in progress cases, recurrence cases, deaths, and loss of view. We considered patients as lost of follow-up when they did not come to their convocation. Recurrence was defined as apparition of a new lesion after a total cicatrization.
When healing was obtained, we were looking for prescription or not of secondary prevention casting-off.
When patients were addressed in a preventive motive, we required occurrence or not of podiatric complication.
Finally, the mean number of consultations by patient was noticed.
1.2.4
Consultation setting in CHU de Limoges
Diabetic foot consultation is established in Limoges since April 2004.
Medical participants are physical and rehabilitation medicine (PRM) doctor (permanent member), dermatologist (permanent member), diabetologist, infectiologist, and angiologist.
Paramedical participants are nurse, orthoprothesist, and podiatrist.
Consultation takes place twice a month in the PRM unit, in a vast room near to the orthoprothesist’s workshop, with complete podiatric equipment.
The type of treatment depends on multidisciplinary decision. When hospitalisation is required, it is easily organized by the representant of the unit needed. In case of ulcers in final step of cicatrization, or when problematics of fitting or diabetes treatment remain isolated, patients are directed toward the adapted specialized consultation.
1.2.5
Type of fitting
Location, severity, presence of arteriopathy, patient’s autonomy are criteria to the prescription of the type of casting-off. In this study, we distinguished off-loading shoes (anterior or posterior), fiberglass cast boot, and total off-loading in hospitalisation.
Because we had observed a bad compliance to removable fitting, we decided to realize only non-removable fitting. To limit decubitus complications and examine daily the lesion, we realize rigid fiberglass boot, made-to-measure, windowed, with important upholstery, wadding internal sole, and two rubber lifts. Boots are baked-off, in the orthoprothesist’s workshop, by the same experimented staff, and made weekly. As soon as evolution permits it, we shift the boot by an off-loading shoe.
Total off-loading in hospitalisation is proposed in last resort, when fitting is impossible because of the severity of the arteriopathy, or the size of the lesion.
1.3
Results
Our study included two evaluations: the first one, retrospective, in June 2008, and the second one, prospective, in January 2010. We chose to present our results at these two periods since they provide complementary data. Indeed, in June 2008, after a mean of 29 months of the first consultation, preventive and therapeutic actions decided initially were quite achieved, so it is a treatment phase. Whereas, in January 2010, the results correspond to the follow-up of our population.
1.3.1
Global description
Overall, 78 diabetic patients have been referred to the multidisciplinary consultation between the first January 2005 and the31st December 2006. There were 51 men (65.4%) and 27 women (34.6%). The mean of age at the first consultation was 64.7 years. Most of them came from Limousin, and 11.5% from extraregional.
Percents of the different specialists who referred patients are reported in Table 1 .
| Instigator doctors | Number of patients in % |
|---|---|
| General practitioners | 25.6 |
| Specialists | 70.5 |
| Independent diabetologists | 14.5 |
| Hospital specialists | 85.5 |
| Diabetology | 48.9 |
| Dermatology | 25.5 |
| PRM | 6.4 |
| Haemodialysis | 4.2 |
| Vascular surgery | 8.5 |
| Infectious diseases | 4.2 |
| Orthopaedics | 2.1 |
Regarding the type of diabetes, there were 14.1% of type 1, 37.2% non insulin-dependant type 2, and 48.7% insulin-dependant type 2.
More often, patients suffered of a complicated diabetes: 17.9% of isolated neuropathy, 12.8% of isolated arteriopathy, 50% of association neuropathy-arteriopathy. Seven patients (9%) presented major or minor amputation. One quarter (25.6%) had nephropathy.
On 78 diabetic patients, 24 were referred for primary prevention, 42 for foot ulcer (53.8%), and 12 for secondary prevention (15.4%).
The mean number of consultations was 4 per patient, whatever the motivation of consultation.
1.3.2
Results of primary prevention (24 patients)
In case of primary prevention, all patients presented a podiatric risk defined as grade 2. These patients were widely addressed (41.7%) by diabetologist. Only two patients already had plantar orthesis or orthopaedic shoes. Fitting was proposed in 90.3% cases: plantar orthesis everytime, orthoplasty in 21.4%, orthopaedic shoes in 7.1%. During a consultation for primary prevention, the mean number of interventions (PRM, diabetologist, dermatologist, podiatrist or nurse) was 2.89 per patient.
In June 2008, after a medium follow-up of 29 months, the mean number of consultations was 3.46 per patient, and primary prevention had been effective in all cases. It means that no podiatric complication occurred in this period.
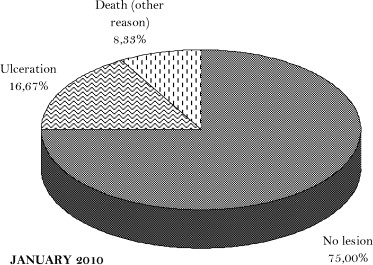
However, in January 2010, after a medium follow-up of 48 months, foot ulcer had appeared in 16.67% of our patients ( Fig. 1 ). But only two had been followed within the multidisciplinary consultation. Indeed, mean number of consultations between June 2008 and January 2010 was 0.23 per patient.
1.3.3
Results of curative treatment
On 42 patients referred from ulceration, 24 had no osteitis, and 18 presented osteitis at time of first consultation (42.8). Our study shows an evolution very different according to the presence or not of osteitis. That’s why we chose to present first the results on the whole population with ulceration, and then the results functions of presence or not of osteitis.
1.3.3.1
Results of all patients with foot ulcer (42 patients)
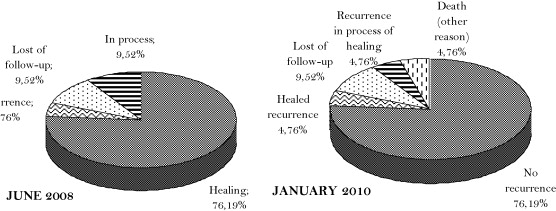
Evolution in June 2008 is reported in Fig. 2 . Healing had been obtained in 63.6% of cases with off-loading shoes, versus 81.8% of cases with fiberglass cast boot. Toe amputation had been realized in five patients (11.9%), cicatrization was in process for one patient, and had been achieved for the four other ones. No major amputation was performed.
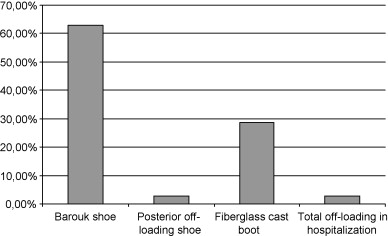
Protection from weight bearing had been indicated in most of time (83.3%). Modalities are described in Fig. 3 . Fiberglass cast boot had been prescribed in 28.6% of cases, 28.6% of which were relieved by Barouk shoe.
Mean number of consultations in case of ulceration was 5.53 per patient.
More than a third of patients (35.7%) need an hospitalisation: osteitis above all ambulatory treatment, high vascular risk, Charcot’s foot in acute period, difficulties to follow-up the casting-off by consultations. The mean length of stay in hospitalisation was 26.9 days.
Once healing was complete, secondary prevention was managed by fitting for 37 patients (88.1%). Modalities are reported in Table 2 .
| Type of fitting | Number of patients in % |
|---|---|
| Plantar orthesis | 88.1 |
| Orthopaedic shoes | 42.8 |
| Orthoplasty | 14.3 |
Evolution in January 2010 (i.e. medium follow-up of 48 months) of these 42 patients suffering from ulceration shows the stability of the results in time ( Fig. 2 ). Between June 2008 and January 2010, the mean number of consultations per patient was 0.4.
1.3.3.2
Results of patients with ulceration without osteitis (24 patients)
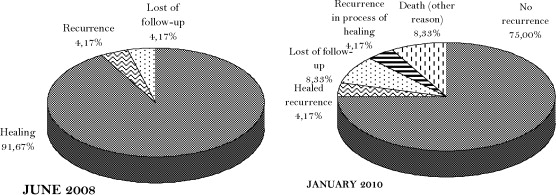
These results are presented Fig. 4 . In June 2008, healing was obtained in 91.7% of cases. In January 2010, recurrence rate was 8.33% that concerned two patients; one of them had recovered by healing and the other one need a toe amputation whose cicatrisation is still in process.
1.3.3.3
Results of patients with ulceration complicated by osteitis (18 patients)
Fig. 5 shows the main results. In June 2008, after a medium follow-up of 29 months, healing rate was 55.6%, and 22.2% of patients remained in process of treatment. 28% had required a toe amputation (the five patients described above); 16.6% were lost of follow-up (it was three patients, two of them had refused amputation and one had refused total off-loading in hospitalisation).
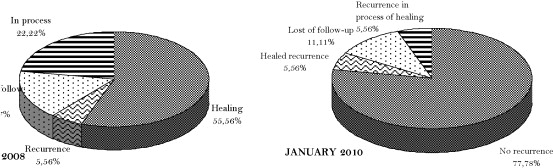
After a medium follow-up of 48 months, all patients whose cicatrisation was in process in June 2008 (22.22%) and those who had presented a recurrence (5.56%) got healed without recurrence in January 2010. One patient who had been lost of view (for refusal of total off-loading in hospitalisation) came back to consultation, with favourable evolution. Finally, between June 2008 and January 2010, there were only two recurrences on 18 patients, one of which had favourable evolution and the other one remains in process of cicatrisation.
1.3.4
Results of secondary prevention
Results of our management in secondary prevention are reported Fig. 6 . Recurrence rate in January 2010 was 25%. For these three patients who presented recurrence of ulceration, one required a femoral amputation. This is the one and only case of major amputation in our population.
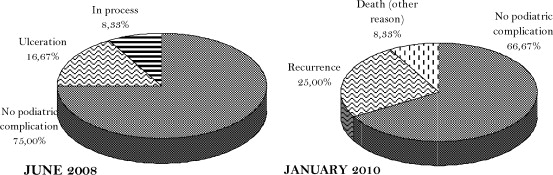
Between June 2008 and January 2010, the mean number of consultations for patients initially referred for secondary prevention was 0.08.
1.4
Discussion
1.4.1
Discussion about curative treatment
In our study, the evolution was initially favourable (healing rate of 76.19% after a medium follow-up of 29 months), and persisted in time since results of January 2010 are similar, with a low recurrence rate (9.52%).
Evaluation on June 2008 highlights a large difference of results according to the presence or not of osteitis. The presence of osteitis affects cicatrisation, since healing rate falls from 91.7% without osteitis to 55.6% with osteitis, and highly increases the delay of cicatrisation since 22.2% of patients were in process of treatment in June 2008 in case of osteitis, versus 4.17% without osteitis. Moreover, there was no amputation on patients without osteitis whereas five toe amputations had been performed on patients with osteitis.
However, in January 2010, both groups (with or without osteitis) got similar results.
Finally, in our study, the initial presence of osteitis influences healing time and functional prognosis (in relationship with toe amputation), but not the medium-term evolution (mean of 48 months).
Besides, our results were comparable to the study of PMR department of Strasbourg . We got a higher healing rate than Erlher et al. (76.19%versus 64.39%) and a lower amputation rate: 11.9% of our patients had to have minor amputation (in all cases, toe amputation) and no major amputation had been performed, whereas Erlher et al. report a minor These differences can be explained by a shorter follow-up (4 years in our study versus 5 years) and by the fact that our population seems to be less severely affected, with fewer mixed complications (50% versus 69.20%). Moreover, our multidisciplinary consultation seems to intervene earlier in the management of diabetic foot ulcer, since in our population referring for ulceration, only 9% presented amputation, versus 61.54% (48 patients) in Erlher et al. population.
Furthermore, our results on patients suffering from osteitis can be compared to the study performed in the podiatry unit of the diabetology department at the Pitié Teaching Hospital in Paris . We got a global cicatrisation rate of 55.5% after a mean of 29 months of treatment, and 77.8% after a medium follow-up of 4 years, whereas Ha Van et al. reported a cicatrisation rate of 70% at 16 months. Compared to this study, our results are lower at the first evaluation, but identical at the second one, that suggests a longer healing time. We obtained a similar limb salvage (100% in our study, 97,5% for Ha Van et al.), and a lower minor amputation rate (five patients on 42 versus 37 on 118 patients for Ha Van et al.). These results probably follow from different strategy of management: in Limoges, management is essentially based on a medical and ambulatory treatment , whereas Ha Van et al. describe a standardised treatment strategy, including a second-line surgical treatment.
1.4.2
Discussion about modalities of protection from weight bearing
To compare the discharge efficacy between half-shoes and fiberglass cast boot, we censored the healing rate obtained from each one, on the whole population suffering from ulcer (with and without osteitis).
In our study, healing was obtained in 63.6% cases with off-loading shoe, versus 81.8% of cases with fiberglass cast boot. There are few comparative studies on protection from weight bearing by half-shoe versus cast boot. However, we can compare our results to a randomized study realised in Saint-Louis by Mueller et al. on the efficacy of “total contact casting” (TCC). On the group treated by TCC, 90% of ulcerations healed in 42 ± 29 days, whereas in the group treated by half-shoe, only 32% of ulcerations healed in 65 ± 29 days ( p < 0.05).
Likewise, our healing rate with fiberglass cast boot is close to the Armstrong et al. study , who reported a healing rate of 82.6% and confirmed the fundamental importance of therapeutic observance.
1.4.3
Discussion about preventive treatment
Primary prevention represents in our study an important consultation motive (30.8%) that can seem surprising for a multidisciplinary consultation. Indeed, considering the French recommendations about the management of diabetic foot, only patients presenting risk grade 3 need multidisciplinary consultation, whereas patients with risk grade 2 are supposed to be followed by ambulatory network.
Our study concerns the beginning of the consultation functioning (2005–2006), and at that time there was not yet such recommendation. In Limoges, ambulatory network was still sparse, and devoid of PMR doctor. Within the external consultations in the PMR department, few diabetic patients were referred for prevention. The fact that 41.7% of patients coming for primary prevention had been referred by diabetologists suggests that needs were clearly identified but means not properly known. The creation of the multidisciplinary consultation contributed to diffuse these information and prevention means. Today, primary prevention seems to be a lesser consultation motive.
About efficacy of this preventive management, results were excellent after a medium follow-up of 29 months since no ulceration had occurred. However, evolution got worse since 16.7% of patients had developed ulceration in January 2010. The international working group on diabetic foot established the spontaneous evolution according to grade of podiatric risk: for grade 2 (such as our population in primary prevention), ulcer occurs in 18.8% of cases at 3 years. Thus, multidisciplinary consultation had initially improved this spontaneous evolution. Secondary aggravation might be due to a lack of follow-up, particularly the fitting-follow-up. Indeed, the main intervention realized during the first consultation consisted in a fitting prescription. Fitting delivery would have been performed in multidisciplinary consultation, in order to verify its tolerance and observance. But afterward, there was no more specialized follow-up of these fitting, which yet is supposed to get worn and lose efficacy with time.
In case of secondary prevention, evolution is known to be definitively unfavourable: Apelqvist et al. reported a recurrence rate of ulceration of 70% at 5 years, and the international working group on diabetic foot estimates at 55.8% of cases of grade risk 3 to develop an ulceration at 3 years. Our multidisciplinary management significantly reduces this recurrence rate. Moreover, it is interesting to compare evolution between our patients initially referred for ulceration ( Fig. 2 , January 2010) and our patients initially referred for secondary prevention ( Fig. 6 ). In both cases, it is secondary prevention. However, the recurrence rate is far lower for patients who initially consulted for ulceration (9.52% versus 25%). The more probable hypothesis is that this group got a better follow-up within the multidisciplinary consultation, as shown by the mean number of follow-up consultations.
1.4.4
Limits
Since it is a retrospective study, we could not record systematically some variables, which however could be pertinent, such as Wagner classification and exact healing time. Besides, we report a rate of lost of follow-up of 9.5% on all patients suffering from ulcerations, it is said that four patients, three of which presented osteitis. In the reasons of loss of view, there were two refusals of amputation, one refusal of total off-loading in hospitalisation, and one without explicit reason. Lost of follow-up because refusal of amputation highlights the difficulty to tackle this therapeutic option during ambulatory cares. Perhaps it could be easier to strike up this discussion between doctors and patients once patient is hospitalized, that could permit to doctor to give more complete and progressive explanations, and let patient have more time for reflection.
In order to reduce the number of lost of follow-up and to improve the quality of the follow-up, we are organizing a systematic convocation according to the patient’s podiatric risk.
1.5
Conclusion
In conclusion, our study confirms the efficacy of multidisciplinary management in curative and preventive treatment of diabetic foot, even if our results should be confirmed by a longer-term evaluation. Medium-term results (mean of 48 months) suggest the importance of the follow-up. Outlooks of this work are to extend the multidisciplinary management to podiatric risk of non-diabetic patients, to develop new discharge modalities, to enlarge their indications and improve their tolerance, and at last to compare clinical results to economic ones. This economic evaluation gets all the more importance as recent progress in repayment of podiatric cares for diabetics in France would lead ambulatory networks to reconfiguration.
Conflicts of interest
The authors have no conflict of interest.
2
Version française
2.1
Introduction
Les complications touchant le pied chez les sujets diabétiques sont multiples, graves et encore beaucoup trop fréquentes en France. Au moins 15 % des patients diabétiques souffriront d’une ulcération du pied au cours de leur vie . L’ulcération du pied dans le cadre du diabète est la première cause d’amputation en France. L’incidence annuelle des amputations chez le diabétique est de 200 à 800 pour 100 000, leur prévalence de 1,3 %. Elles sont précédées d’un ulcère dans 50 à 70 % des cas. Le risque d’amputation est dix à 30 fois supérieur par rapport à population générale. La présence d’une ulcération multiplie par deux à dix le risque d’amputation et par 2,4 le risque de décès par rapport à une population diabétique indemne de lésion du pied. Le taux de survie cumulée sur trois ans est de 72 % chez un diabétique porteur d’ulcère contre 87 % dans la population diabétique contrôle. Un ulcère récidive dans 70 % des cas à cinq ans . Après amputation, la survie à cinq ans est à 58 %, et une nouvelle amputation est nécessaire dans 50 % des cas à cinq ans. L’incidence des ulcérations varie avec l’âge, le sexe masculin, le niveau économique et l’accessibilité aux soins.
D’où l’importance capitale de développer la prévention primaire, d’assurer une prise en charge thérapeutique optimale et un suivi régulier des patients diabétiques . Rappelons que dès 1989, l’OMS, par la convention de Saint-Vincent, s’était fixé pour objectif de réduire de 40 % le taux d’amputation liée au diabète. En France, la Haute Autorité de santé a édité en mai 2006 des recommandations pour la prise en charge des patients diabétiques, et a défini en particulier la conduite à tenir pour le dépistage et la prévention des pieds à risque.
Sur le plan médicoéconomique, les plaies du pied sont à l’origine de 10 à 20 % des journées d’hospitalisation pour le diabète . Le coût varie de 9000 à 35 000 euros par hospitalisation. Le diabète est responsable de cinq à 10 000 amputations par an, ce qui représente un coût direct de 76 à 150 millions d’euros. En 2003, a eu lieu la première évaluation du coût de la prise en charge des ulcères du pied chez les patients diabétiques (évaluation des coûts directs et indirects pour l’Assurance Maladie). Les coûts mensuels moyens par patient étaient de 697 euros pour le suivi ambulatoire, 15 556,20 euros pour les hospitalisations (de jour et de court séjour) et 34,76 euros pour les arrêts de travail. Pour les patients ayant été hospitalisés, les hospitalisations représentaient environ 70 % du coût moyen d’un ulcère du pied. La part des coûts ambulatoires était surtout générée par les dépenses en soins médicaux et paramédicaux, les interventions du personnel soignant. En revanche, les traitements médicamenteux ne représentaient que 10 % des coûts. Les facteurs cliniques identifiés comme prédictifs du coût de prise en charge élevé étaient le caractère récent de la lésion et sa gravité initiale. L’amputation et le suivi par un spécialiste étaient corrélés à des coûts plus importants, en lien logique avec les facteurs cliniques. Ces résultats économiques confirment donc, pour les pouvoirs publics, l’intérêt d’une prise en charge précoce des complications liées au diabète.
C’est dans ce contexte qu’a été instaurée, en avril 2004 au CHU de Limoges, la consultation « du pied à risque ». Cette consultation a pour objectif le traitement multidisciplinaire des lésions du pied diabétique, mais également des objectifs de diagnostic, de prévention primaire et secondaire, d’éducation et d’information, et de recueil des données nécessaires en santé publique.
Le but de l’étude était d’évaluer les résultats de cette consultation, en termes de cicatrisation des lésions pour le traitement curatif, et d’absence survenue de complication podologique pour le traitement préventif.
2.2
Patients et méthodes
2.2.1
Type d’étude
Il s’agit d’un suivi longitudinal de cohorte. Nous avons repris les dossiers des patients diabétiques adressés à la consultation entre le 1 er janvier 2005 et le 31 décembre 2006, soit 78 patients. Nous avons inclus tous les patients vus au moins une fois à la consultation. Nous avons suivi leur évolution au moyen de deux évaluations : la première, rétrospective, en juin 2008, soit à une durée moyenne de suivi de 29 mois, et la seconde, prospective, en janvier 2010, soit à une durée moyenne de suivi de 48 mois.
2.2.2
Critères de jugement
Les ulcérations ont été considérées comme guéries lorsqu’elles étaient complètement cicatrisées ; et récidivantes dès qu’il apparaissait une nouvelle plaie après obtention d’une fermeture complète. Le traitement préventif (primaire ou secondaire) a été considéré comme efficace en l’absence de survenue complication podologique lésionnelle.
2.2.3
Données recueillies
Pour chaque patient, nous avons recueilli les données suivantes : sexe, âge, lieu de vie, spécialité et lieu d’exercice du médecin l’ayant adressé, motif de consultation (en portant une attention spéciale aux motifs de prévention), présence ou non d’une ulcération, le type de diabète. Nous avons également noté l’association ou non à une neuropathie, une artériopathie ou une néphropathie.
Nous avons considéré que les patients étaient adressés en prévention primaire quand ils n’avaient pas d’antécédent d’amputation ou d’ulcération, et ne consultaient pas pour une ulcération. En cas d’ulcération, nous avons relevé l’existence ou non d’une ostéite sous-jacente. Le diagnostic d’ostéite porté en consultation était basé sur des arguments essentiellement cliniques (signes d’inflammation locale et contact osseux) et radiologiques (radiographie standard).
Sur les aspects de l’appareillage, nous avons recherché la présence ou non d’un appareillage préalable et sa forme ; puis nous avons distingué les différents moyens de décharge que nous avions utilisés (décharge par résine, par chaussure, par orthèse plantaire, ou décharge totale en hospitalisation). De plus, nous avons identifié tous les patients ayant bénéficié d’un traitement chirurgical, en précisant, dans le cas d’une amputation, son niveau. Nous avons considéré comme mineures les amputations de l’avant-pied (amputations d’orteils et transmétatarsiennes), et comme majeures les amputations réalisées au-dessus de ce niveau.
Enfin, nous avons totalisé le nombre de patients ayant nécessité une hospitalisation, et comptabilisé le nombre de jours d’hospitalisation conventionnelle. Pour l’évolution, nous avons répertorié les cas de guérison, les cas de traitement toujours en cours, les cas de récidive, les décès, et les perdus de vue. Nous avons considéré que les patients avaient été perdus de vue lorsqu’ils ne s’étaient pas présenté aux consultations de suivi qui avaient été programmées. La guérison a été retenue lorsque, cliniquement, la cicatrisation était complète ; et la récidive lorsqu’une nouvelle lésion s’est constituée après une guérison complète.
Dans les cas où la guérison a été obtenue, nous avons relevé si un appareillage en prévention secondaire avait été prescrit ou non, et sous quelle forme.
Pour les patients ayant consulté pour un motif de prévention, primaire ou secondaire, nous avons noté la survenue ou non de complication podologique.
Enfin, nous avons totalisé pour chaque patient le nombre total de consultation.
2.2.4
Description de la consultation
La consultation du pied à risque est instaurée depuis avril 2004.
Les membres médicaux sont : médecin de MPR (permanent), dermatologue (permanent), diabétologue (hospitaliers et de ville), infectiologue, angiologue.
Les membres paramédicaux sont : IDE, technicien d’appareillage, et pédicure/podologue.
La consultation a lieu tous les 15 jours (deuxième mardi du mois, et quatrième vendredi du mois). Elle se déroule dans le service de médecine physique et de réadaptation (MPR) du CHU de Limoges, dans une vaste salle jouxtant l’atelier d’appareillage, et équipée d’appareillages pédicuraux.
Les décisions thérapeutiques sont prises conjointement. Quand une hospitalisation est indiquée, celle-ci est organisée dans le service le plus adéquat par un de ses représentants présents. Pour les plaies en phase finale de cicatrisation ou pour les patients ne se présentant plus que pour des problèmes d’appareillage ou d’équilibre du diabète, les patients sont réorientés vers la consultation spécialisée concernée, afin de ne réserver la consultation qu’à des problématiques multidisciplinaires. Enfin, les dossiers difficiles sont discutés en staff multidisciplinaire ou en fin de consultation.
2.2.5
Moyens de décharge utilisés
La localisation, la gravité, l’éventuelle artériopathie sous jacente, l’autonomie du patient font partie des multiples critères de choix qui guident la prescription du mode de décharge. Dans notre étude, nous avons distingué décharge par chaussure (de décharge antérieure ou postérieure), décharge par botte ou décharge totale en hospitalisation.
Pour les indications à une décharge par botte, nous avons pris le parti de ne proposer que des appareillages non amovibles, notre courte expérience nous révélant une mauvaise compliance à l’appareillage amovible. Pour limiter le risque de complications liées à l’immobilisation et permettre la surveillance quotidienne de l’état cutané, nous réalisons des bottes de marche en résine rigide, sur mesure, fenêtrées en regard de la plaie, munies d’un capitonnage important et d’une semelle interne faits à l’aide d’ouate en rouleaux et équipées de deux talonnettes en caoutchouc. Les bottes sont confectionnées sur place, dans l’atelier d’appareillage, par la même équipe d’orthoprothésistes expérimentés, revues et refaites toutes les semaines. Dès que l’évolution le permet, on effectue un relais par chaussure de décharge.
La décharge totale en hospitalisation reste proposée en dernier recours, lorsque les lésions cutanées sont si étendues ou que l’artériopathie est si évoluée qu’on ne peut proposer ni une chaussure de décharge, ni une botte en résine.
2.3
Résultats
Notre étude a comporté deux évaluations, l’une rétrospective en juin 2008, l’autre prospective en janvier 2010. Nous avons choisi de présenter nos résultats à ces deux périodes, car ils fournissent des informations complémentaires. En effet, en juin 2008, soit 29 mois après la première consultation, l’essentiel des actions préventives et thérapeutiques qu’elle avait induit étaient achevées, il s’agit donc d’une phase de traitement. En janvier 2010, les résultats sont le reflet du suivi de ces patients.
2.3.1
Descriptif global
Au total, 78 patients diabétiques ont été adressés à la consultation du pied à risque entre le 1 er janvier 2005 et le 31 décembre 2006. Il s’agissait de 51 hommes (65,4 %) et 27 femmes (34,6 %). Leur âge moyen à la première consultation était de 64,7 ans. La plupart provenaient du Limousin, et 11,5 % avaient une origine extrarégionale.
La proportion des différentes spécialités ayant adressé des patients est reprise dans le Tableau 1 .







