Evaluation and Prosthetic Management of Proximal Humeral Malunions
Christopher Chuinard
Pascal Boileau
Gilles Walch
INTRODUCTION
With our aging population, proximal humerus fractures are increasing in incidence; so too are their sequelae. Distorted osseous anatomy and/or soft-tissue contractures lead to stiffness and pain; treatment of this pathology is difficult at best. The treating physician needs to have a careful understanding of the pathology and treatment options. The sequelae—nonunions, malunions, and failed osteosynthesis or arthroplasty—can be the result of improper nonoperative management, inadequate reduction or fixation, improper surgical planning, soft-tissue interposition, or overly aggressive rehab or mobilization.
EVALUATION
A careful assessment of the patient’s needs and goals is important to determine the necessity of treatment and expectations. Ideally, the history should include a review of the injury films and subsequent treatment. The disability may be multi-factorial; many patients may have axillary nerve or brachial plexus injuries, and an EMG is warranted. Arterial injury should be suspected if there was a dislocation or displacement of the fracture fragments medial to the conjoined tendon. Suprascapular nerve entrapment can occur with a malunion, leading to chronic pain. Previous surgery can contribute to neurovascular compromise or persistent propionibacterium acnes infection. Patient factors, i.e., alcoholism or diabetes, may have contributed to failure of the previous treatment.
While Neer31,32 was the first author to describe the difficulties of treatment of “Old Trauma,” multiple authors have considered shoulder arthroplasty to be an unpredictable treatment for sequelae of proximal humerus fractures.1,3,4,20,33,34,47 The unpredictable results for unconstrained shoulder arthroplasty for the treatment of sequelae of proximal humerus fractures results from the complexity of the bone loss and associated deformities.1,2,3 and 4,11,14,15,17,19,20,21,22,23 and 24,27,28,29,30,31 and 32,34,35,40,44,47
Without a classification scheme for proximal humerus fracture sequela it is difficult to build consensus for appropriate surgical treatment, to compare results among differing treatment algorithms, or provide patients with possible outcomes. Furthermore, the number of cases in each series is limited and the pathology is ill-defined and heterogeneous with respect to the anatomic lesions.1,3,4,12,14,17,19,20,21,22,23 and 24,27,32,34,37 Because these patients are often younger and more active than patients treated for osteoarthritis (OA), the prognosis is crucial when deciding on potential treatment.8,5,6
Simply describing the pathology as a nonunion or malunion was not adequate to assign a treatment algorithm. A fracture sequelae classification has been developed with prognostic implications in mind5,6,8; its application can help the treating surgeon make recommendations based upon radiographic data. The classification scheme was borne out of a diligent review of 221 sequelae of proximal humeral fractures treated with a shoulder prosthesis; the patients were followed for a minimum of 2 years to be included in the series (mean follow-up 42 months). There were 145 women and 75 men (1 woman was operated on both shoulders). The average age of the patients at the time of shoulder arthroplasty was 61 years. The Neer classification of proximal humeral fractures was applied to the initial injury30: 26 two-part fractures, 38 three-part fractures, and 74 four-part fractures were identified (63% of the series). A total of 118 (53%) underwent nonoperative treatment of the initial fracture, and 60 (27%) underwent an operative procedure to reduce and fix the initial fracture. The classification was then retrospectively applied and the outcomes were evaluated (including constant score and range of motion)13; we found statistical correlation between the final functional results and the following parameters6,8,9:
A greater tuberosity osteotomy jeopardized the final functional results (P value <0.0005);
Initial nonoperative treatment led to better final results than initial open reduction and internal fixation (P value <0.008) for the patients requiring treatment of the sequela;
The functional results of nonconstrained shoulder replacement in cases of cephalic collapse or necrosis and locked
dislocation or fracture-dislocation were significantly better than in cases of surgical neck nonunion and major tuberosity malunion (P value < 0.0005);
Any complication (P < 0.03) or revision surgery (P < 0.003) greatly affected the final result.
While no substitute for the clinical examination, the X-rays, CT scan, or MRI can provide the surgeon with an understanding of the distorted anatomy, posterior tuberosity displacement can block external rotation; superior tuberosity displacement can limit abduction either mechanically or by limiting the mechanical advantage of the rotator cuff.21 Ideally, the sequelae classification can help the surgeon choose an appropriate surgical option based upon radiographic data and provide both the surgeon and the patient with some expectation of outcome when an arthroplasty option is selected. Furthermore, the classification should provide some general treatment guidelines.
What follows is a simple algorithm for classification. The status of the greater tuberosity has dramatic prognostic import. The body seems to have the capacity to heal one insult to the greater tuberosity but not two or more. Therefore, we feel that if a tuberosity osteotomy is necessary, a standard prosthesis may be contraindicated. Based upon anteroposterior X-ray and axillary or outlet lateral X-ray, the surgeon needs to answer the following questions:
Is this the result of a missed dislocation?
Is there a surgical neck nonunion?
If yes, is the greater tuberosity healed to the proximal fragment?
Is there a gross malunion or nonunion of the head/tuberosity anatomy, or would stem implantation be impossible without a greater tuberosity osteotomy?
Is the greater tuberosity healed to the humerus?
If yes, using a modular, adaptable prosthesis, can a humeral stem be implanted without an osteotomy?
The above questions serve as the basis of our classification scheme:
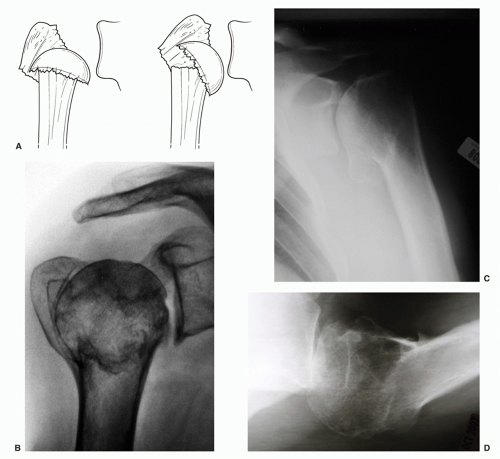
Type 1: impacted valgus or varus fracture with cephalic collapse or necrosis (Fig. 29-1)
Type 2: locked dislocation and fracture-dislocation (Fig. 29-2)
Type 3: nonunion of the surgical neck (Fig. 29-3)
Type 4: displaced fractures with severe tuberosity malunion or nonunion (Fig. 29-4)
MANAGEMENT
If the X-ray shows a healed greater tuberosity but cephalic necrosis (type 1), then a standard shoulder arthroplasty has an excellent chance for success—if the stem can be implanted without osteotomizing the greater tuberosity (Fig. 29-5A-D). It is important to remember that the prosthesis must adapt to the patient’s anatomy and not vice versa. Modern prostheses with adaptable geometry can help recreate native anatomy; older generation systems often do not allow the freedom to conform to distorted anatomy and should, therefore, be used with caution. Newer “micro” stems or custom stems with short lengths or metaphyseal fitting stems can provide an additional option (Fig. 29-5E). Resurfacing implants are not likely to have a sufficient cancellous bed for secure fixation. Modern, low-profile fracture stems that allow copious bone grafting may improve results in cases when an osteotomy must be performed. Furthermore, rotator cuff integrity has been demonstrated to influence outcome (minimal fatty infiltration and an acromial humeral distance of >7 mm), so the prosthesis must respect the soft tissue surrounding it.5,27,29 Pay attention to the position of the tuberosity relative to the acromion, if it is in a normal relationship, then place the prosthesis in a normal or anatomic position (Fig. 29-1B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree