Evaluation and Management of Humeral Shaft Nonunions and Malunions
Charles L. Getz
Matthew L. Ramsey
INTRODUCTION
Fractures of the humeral shaft occur relatively frequently and are typically treated successfully by functional bracing with a reported nonunion rate of 1.8% to 3.9% for closed fractures and 6% for open fractures.22,23 and 24 Malunion is less commonly reported. When surgery is required, the results are also predictable for healing and functional results.7,13
HUMERAL SHAFT NONUNION
Therefore, an unusual complication is nonunion of humeral shaft fracture. These can be broadly divided into two types, those that were initially treated nonoperatively and those that had previously undergone surgery. Nonunion has occurred when there is evidence of hardware failure or if there is no bridging callus at 4 to 8 months from surgery.7
Evaluation of the Patient with Nonunion
Consideration of the patient’s previous treatment is helpful to determine why the fracture did not heal primarily. By elucidating the etiology of the nonunion, the surgeon can create a treatment strategy that addresses the underlying cause for the nonunion.
Patients with nonunion from nonoperative treatment are often the results of inadequate immobilization. The resulting hypertrophic nonunion will have evidence of callus formation but a lack of bridging callus. Plain films are often adequate to make the diagnosis. In more difficult cases, a computed tomography scan of the fracture site with 1 mm cuts are useful to determine if bridging callus is present.
Another circumstance is the nonoperatively treated humeral shaft fracture that shows a lack of callus formation or an atrophic nonunion; this is determined on plain radiographs. An atrophic nonunion occurs because of problems with the healing biology as opposed to fracture stability. The issues can be local such as an infection, or systemic, such as renal disease, diabetes, smoking, malnutrition, or metabolic disease. When evaluating the patient with an atrophic nonunion, an underlying etiology should be sought and addressed to improve healing of the repair.
The patient with previous surgery on the humerus presents a different set of considerations. The fracture may not heal because the fixation (either plate or rod fixation) was either too rigid or not secure enough. Altered local tissue biology, from infection or disrupted blood supply from soft tissue stripping from surgery or the original injury, such as seen following open fractures, may also play a factor. And finally, the systemic causes of atrophic nonunion previously described can also lead to failed surgical osteosynthesis and therefore should be considered.
Surgical Planning
Treatment of humeral shaft nonunions is surgical in those patients in adequate health to undergo surgery. Experts in the use of external fixation and Illizarov frames have reported successful outcomes.13,16,17 and 18,25 However, risk of neurovascular structure, pin tract infections, and unfamiliarity are downsides to this technique. The use of rods for treatment of nonunions has been also reported with a wide range of success. However, failure rates have been as high as 40%.6,15,26 McKee reported a 40% failure rate when using humeral rods compared to 100% union rate with plate repair and bone grafting.15
Foster has reported more predictable union rates with plate fixation compared to Rodding (80% versus 72%) with less complaints of shoulder pain.6
Compression plating, when possible, or bridge plating, is the treatment of choice for nonunion repair. The surgical approach takes in several considerations. The first is adequate exposure of the fracture site and plate application. The second is removal of the prior hardware. The third is safe control of the radial and ulna nerves. And lastly, scarring from previous surgical approaches.
Nonunion from Prior Nonoperative Treatment
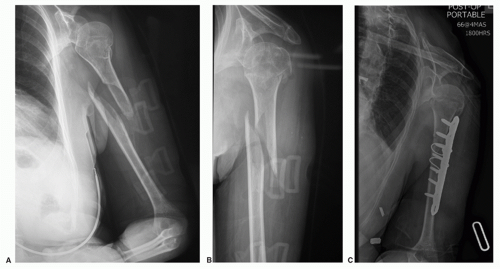
A common scenario is a patient who has been treated with a functional brace and the fracture has failed to unite resulting in a hypertrophic nonunion. For proximal third fractures an anterior approach is most commonly used (Fig. 30-1). For distal third fractures, a posterior approach is used. Midshaft fractures can be approached either from anterior or posterior (Fig. 30-2). Once the nonunion site is exposed, the intervening scar tissue is removed back to the bone. The intramedullary canal is recreated and some of the hypertrophic bone may be removed to allow plate placement and saved for graft. Freshening the bone ends with a rongeur will allow for maximal bone contact. Compression plating with a large (4.5 mm) dynamic compression (DC) plate with six to eight cortices of fixation on each side of the fracture secures the repair. Bone loss is exceptionally rare in patients with hypertrophic nonunions. The hypertrophic bone that was removed is then used as graft material at the fracture site to fill any areas that are not compressed.
As previously mentioned, with atrophic nonunion there can be an underlying medical condition that must be addressed for successful nonunion repair. Selection of the surgical approach is based on the location of the fracture site as previously described. Bone loss may be present and shortening of the humerus up to 2 cm is acceptable. More shortening will lead to triceps weakness.10 Bone grafting to improve fracture healing is frequently used in atrophic nonunion repair to improve the local healing biology. When direct compression plating cannot be achieved because of bone loss, wave plating with bone grafting has proven a successful option.
The bone graft source for nonunion repair in the atrophic setting has traditionally been from autologous iliac crest.19,20 Recently, the use of allograft bone matrix and bone morphogenic protein has been explored.5,9 Also, the use of internal or external bone stimulators can be further used to enhance fracture biology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree