Epidural steroid injection (ESI) has been used to treat cervical radiculopathy for several decades. Generally, available studies demonstrate favorable results, although definitive evidence of efficacy is lacking. ESIs are not considered a first line treatment and are undertaken after non-interventional treatments have been adequately provided. In the cervical spine, where evidence of potential benefit is moderate and there is risk of major complication, non-interventional care is even more germane. This article reviews the available literature regarding risks and efficacy of ESIs for cervical radiculopathy, and aims to guide practitioners in treatment decisions for individual patients.
The injection of glucocorticoid (steroid) medication into the epidural space to treat back pain was first performed in the 1950s. The first publication of cervical epidural steroid injection (ESI) for radicular pain was in 1961. In the 1960s, initial reports in the United States described treatment of sciatica using the caudal and interlaminar (IL) approaches. By the mid 1970s, injections via the transforaminal (TF) approach alongside the nerve root were described in combination with fluoroscopic radiograph guidance.
The founding principle of injecting steroid and anesthetic medication into the epidural space is that it decreases pain and inflammation at the site of injection. A herniated disc is the most commonly proposed mechanism of increased inflammation and pain. Herniated disc material has been shown to cause an inflammatory response in the dura, nerve roots, dorsal root ganglion, and the spinal cord, with a notable increase of phospholipase A 2 activity. Human lumbar disc herniation extracts have shown 20 to 10,000 times greater phospholipase A 2 activity than any other human source. Other immunohistochemical substances implicated in increasing inflammation and pain from discs include matrix nitric oxide, metalloproteinases, prostaglandin E 2 , and interleukin 6. The hypothesis is that steroid medication in the epidural space interrupts the inflammatory cascade in addition to inhibiting neural transmission by nociceptive C fibers. Disc herniation is only one possible cause, and cervical spondylotic foraminal and central stenosis can also cause radiculopathy. The various etiologies of radiculopathy may respond differently to ESIs.
General indications
ESIs have been used to treat a variety of spinal disorders. They are primarily and most widely accepted as a treatment of radicular symptoms. Patients with radicular pain that has been unresponsive to noninterventional care for 1 to 2 months including physical therapy, medications, and education are candidates for ESIs. In patients without progressive neurologic deficit or cervical myelopathy, ESIs are considered as a rational part of treatment before surgical intervention. However, the potential benefits must be weighed against the possible risks for each patient.
Complications of ESIs
In general, risks of spine interventions are related to needle placement, the medications used, and patient factors. These include, but are not limited to, tissue trauma, bleeding, infection, nerve/cord injury, spinal block, medication side effects/toxicity, and allergic reaction. Minor procedural complications vasovagal reactions, nausea, transient neurologic symptoms, and increased neck or arm pain. Transient complications with ESIs can occur as a result of side effects of steroids, anesthetics, and contrast dye. Another risk to consider is radiation exposure. More specific risks for cervical ESIs depend on the route of administration. Both the IL and the TF routes have risk, but the TF route has a higher rate of major complications.
A recent review of cervical IL ESI complications included studies from 1996 to 2005. The investigators cited 2 studies specific to IL ESI, one documenting the rate of complication as just less than 1%, whereas conversely the other reported a 16.8% rate. Minor complications included increased axial neck pain, nonpositional headache, facial flushing, vasovagal episode, superficial skin infection at the site of injection, insomnia, and nausea/vomiting. Major complications included epidural hematoma, subdural hematoma, subdural block, intrathecal block, dural puncture, persistent/permanent neuropathic symptoms, intracranial hypotension and granuloma, permanent spinal cord injury, pneumocephalus, venous air embolism, cervical epidural abscess, and Cushing syndrome for 12 months after a single ESI with 60 mg of methylprednisolone. One reported case of death was caused by complications after epidural hematoma. Of the permanent spinal cord injuries, 2 were caused by direct trauma, 3 were caused by epidural hematoma, and in one case there was no apparent trauma. The investigators noted that many of the severe complications could be avoided by precise needle placement and careful technique. Bleeding diathesis and thus potential for hematoma could theoretically be avoided with a careful patient history. Only one of the 3 epidural hematomas cited, however, was clearly associated with anticoagulation or antiplatelet medication.
For TF ESI, the minor complications are similar to the IL route, although major complications are more frequent. Initially, case reports related to the risk of cervical spinal cord and brain injury with cervical TF ESIs raised awareness of potential serious complications. In 2007, a large retrospective anonymous survey of the American Pain Society asked physicians to report known complications of cervical TF ESIs. A total of 21.4% (287/1340) responded, reporting 74 major complications (lasting >24 hours). Many of these were purportedly due to inadvertent intrarterial injection of particulate steroid causing embolism in the brain and/or spinal cord. In 2010, a review of the literature on complications of cervical TF ESIs cited 105 published major complications, 68 of these with details available. Complications included brain infarction and edema, spinal cord infarction, cortical blindness, high spinal anesthesia, seizure, and bleeding. Fifteen of these led to death. Another 35 cases of major complication are referred to in the literature, but have not been published. The exact number of major complications is unknown. Some practitioners argue that anonymous surveys may overestimate the number of these cases, because more than one physician could report the same case. On the other hand, because of medical-legal issues, the number of major complications may be underestimated. The proposed mechanisms of severe spinal cord and brain injuries include injection of particulate steroid into vertebral or cervical radicular arteries, needle-induced dissection/thrombosis/vasospasm, and intraarterial injection of anesthetic or pharmaceutical preservatives/vehicles. Needle misplacement is the primary mechanism by which these occur.
Complications of ESIs
In general, risks of spine interventions are related to needle placement, the medications used, and patient factors. These include, but are not limited to, tissue trauma, bleeding, infection, nerve/cord injury, spinal block, medication side effects/toxicity, and allergic reaction. Minor procedural complications vasovagal reactions, nausea, transient neurologic symptoms, and increased neck or arm pain. Transient complications with ESIs can occur as a result of side effects of steroids, anesthetics, and contrast dye. Another risk to consider is radiation exposure. More specific risks for cervical ESIs depend on the route of administration. Both the IL and the TF routes have risk, but the TF route has a higher rate of major complications.
A recent review of cervical IL ESI complications included studies from 1996 to 2005. The investigators cited 2 studies specific to IL ESI, one documenting the rate of complication as just less than 1%, whereas conversely the other reported a 16.8% rate. Minor complications included increased axial neck pain, nonpositional headache, facial flushing, vasovagal episode, superficial skin infection at the site of injection, insomnia, and nausea/vomiting. Major complications included epidural hematoma, subdural hematoma, subdural block, intrathecal block, dural puncture, persistent/permanent neuropathic symptoms, intracranial hypotension and granuloma, permanent spinal cord injury, pneumocephalus, venous air embolism, cervical epidural abscess, and Cushing syndrome for 12 months after a single ESI with 60 mg of methylprednisolone. One reported case of death was caused by complications after epidural hematoma. Of the permanent spinal cord injuries, 2 were caused by direct trauma, 3 were caused by epidural hematoma, and in one case there was no apparent trauma. The investigators noted that many of the severe complications could be avoided by precise needle placement and careful technique. Bleeding diathesis and thus potential for hematoma could theoretically be avoided with a careful patient history. Only one of the 3 epidural hematomas cited, however, was clearly associated with anticoagulation or antiplatelet medication.
For TF ESI, the minor complications are similar to the IL route, although major complications are more frequent. Initially, case reports related to the risk of cervical spinal cord and brain injury with cervical TF ESIs raised awareness of potential serious complications. In 2007, a large retrospective anonymous survey of the American Pain Society asked physicians to report known complications of cervical TF ESIs. A total of 21.4% (287/1340) responded, reporting 74 major complications (lasting >24 hours). Many of these were purportedly due to inadvertent intrarterial injection of particulate steroid causing embolism in the brain and/or spinal cord. In 2010, a review of the literature on complications of cervical TF ESIs cited 105 published major complications, 68 of these with details available. Complications included brain infarction and edema, spinal cord infarction, cortical blindness, high spinal anesthesia, seizure, and bleeding. Fifteen of these led to death. Another 35 cases of major complication are referred to in the literature, but have not been published. The exact number of major complications is unknown. Some practitioners argue that anonymous surveys may overestimate the number of these cases, because more than one physician could report the same case. On the other hand, because of medical-legal issues, the number of major complications may be underestimated. The proposed mechanisms of severe spinal cord and brain injuries include injection of particulate steroid into vertebral or cervical radicular arteries, needle-induced dissection/thrombosis/vasospasm, and intraarterial injection of anesthetic or pharmaceutical preservatives/vehicles. Needle misplacement is the primary mechanism by which these occur.
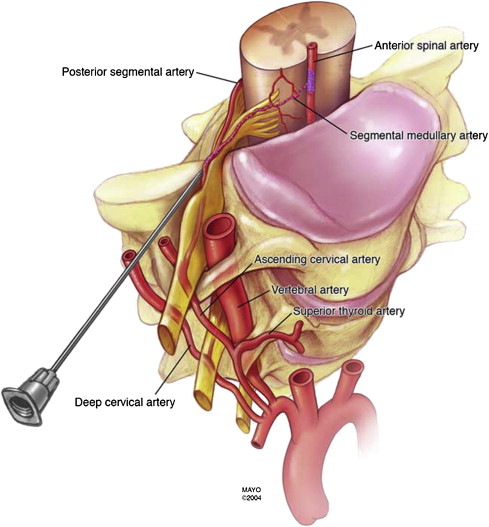
Anatomy relevant to cervical ESI
Performing technically sound injections to maximize efficacy and minimize risk requires exact knowledge of the anatomy. The epidural space contains the spinal nerve roots and their dural sleeves, the internal vertebral venous plexus, loose areolar tissue, segmental blood supply, adipose tissue, and lymphatics. The location of the dura is an obvious consideration, and the vascular structures are even more important. The epidural veins form an arcuate pattern, positioned laterally at the level of each vertebral body. This consideration is important for IL ESIs because venous puncture is more likely to occur laterally than with midline approaches. Venous injection may not typically cause serious injury, but it decreases or voids the efficacy of the injection because the medications are dispersed into the circulation.
Key anatomic features of the cervical spine include a thin ligamentum flavum (unfused in the midline in approximately half of individuals), absence of the interspinous ligament, and a small posterior epidural space (distance between the ligamentum flavum and dura mater). At C6 to 7 and C7 to T1, where the epidural space is the widest and most IL ESIs are placed, the mean width is 3 mm (1–4 mm).
The cervical arterial anatomy within and near the intervertebral foramina is pertinent to TF ESIs. The vertebral artery is an obvious hazard. Although it typically lies anterior in the foramen, some individuals may have a tortuous vertebral artery with a more posterior location near the target for injection in the posterior foramen. Also vulnerable are spinal branches of the ascending and deep cervical arteries contributing to radicular or segmental medullary branches to the anterior spinal artery supplying the anterior spinal cord. Injury or injection of embolizing matter to these spinal branches can cause anterior spinal cord injury ( Fig. 1 ). In addition, these branches anastomose with branches from the vertebral artery and could jeopardize brainstem and cerebellar tissues supplied by the vertebral circulation. These spinal arterial branches can enter the foramen posteriorly, at the usual location for TF ESI needle placement. Therefore, appropriate technique with consideration and knowledge of the anatomy and its appearance on fluoroscopic images is critical to avoid serious complications.
ESI approaches, evidence, and efficacy
Techniques available to access the cervical epidural space include the IL and TF approach. The TF route has become more common because it may place the medication more directly at the site of the proposed cause of pain. Prospective studies by Derby and others in the 1990s described improved outcomes using the TF route for radicular pain in the lumbar spine. Similar studies comparing the IL and TF routes are not available for the cervical spine, although there is some evidence to suggest the TF route has advantages for certain diagnoses. The varied ESI techniques and diversity of etiologies of radicular pain make the comparison of studies difficult, and it is likely that all types of ESIs are not equally efficacious for all causes of radiculopathy. The next sections provide an overview of the literature and are not intended to serve as a reference for conducting the procedures.
Fluoroscopy
The use of fluoroscopic guidance for epidural needle placement in the cervical spine is considered standard of care. Fluoroscopy is used in conjunction with radiopaque contrast to establish correct epidural placement without intravascular injection. In the past, IL placement was sometimes made without fluoroscopic guidance. However, inaccurate needle placement occurs in 17% to 53% of IL injections performed without fluoroscopic guidance.
For TF ESI, fluoroscopy is mandatory along with the use of real-time fluoroscopy or digital subtraction angiography to assess for vascular injection. Negative aspiration is not a reliable means of detecting intravascular placement. Greater than 50% of cases in which intravascular placement was documented by digital subtraction angiography had negative aspiration. The documentation of epidural flow also does not rule out vascular injection, because a combination of epidural and vascular flow is often encountered. Real-time or live fluoroscopy is performed by continuous fluoroscopy while contrast media is injected. Digital subtraction angiography is performed in the same manner by the physician, but requires additional software that “subtracts” stationary objects on the fluoroscopic image and shows only moving or new objects. With this software, vascular structures are not obscured by radiopaque structures and are more readily visualized. Digital subtraction angiography has been shown to be superior to live fluoroscopy in the cervical spine in which the rate of detection of intravascular injection nearly doubled to 32.8% compared with 17.9% with real-time fluoroscopy.
Injectate
There are no standardized practices for the type and volume of medication administered via an epidural injection, and there is significant variation across disciplines and institutions. A steroid/local anesthetic mixture is the most commonly used for ESI in both academic institutions and private practices. The volume of the injectate varies based on the approach used. Generally, volumes do not exceed 2 to 3 mL for TF and 3 to 4 mL for cervical IL ESIs. Some argue that larger volumes may dilute the injectate and lessen effects at a specific target.
More recently, the question of risks and efficacy of particulate versus nonparticulate steroids for TF ESIs has been raised. Given the risk of intraarterial injection and neurologic sequelae described earlier, most physicians now use nonparticulate steroid for cervical TF ESIs. Intraarterial injection of nonparticulate steroid did not cause embolic injury in one animal study. In this study, direct injection of steroid into the vertebral artery of pigs showed none that received particulate steroid (methylprednisolone) regained consciousness, whereas all of those that were administered nonparticulate steroid showed no evidence of neurologic injury and no changes were noted on magnetic resonance imaging. Therefore, if inadvertent intraarterial injection were to occur during TF ESI, nonparticulate steroid should not result in neurologic injury.
However, there is some debate that particulate steroids may not be as efficacious as nonparticulate steroids. In 2006, a small study comparing effectiveness in cervical TF ESI noted that there was no statistically significant difference, but there was a trend favoring particulate steroids. In 2009, a larger retrospective study comparing triamcinolone (particulate) versus dexamethasone (nonparticulate) in cervical TF ESI for cervical radiculopathy found no significant difference in effectiveness or in the rate of those who went on to have surgery. However, there is a lumbar TF study that suggests pain scores are significantly more improved with triamcinolone versus dexamethasone at 1 month. Limitations of this study include that the baseline pain scores were significantly different between groups, confounding the results. In addition, there was not a significant difference in Oswestry disability scores between groups. Overall, nonparticulate steroid is nearly or equally effective as particulate steroids in cervical TF ESI for the treatment of radiculopathy and carries less risk of causing major neurologic injury.
IL Approach
Technique
The IL technique achieves access to the epidural space using a midline approach preferably one spinal segment below the suspected disease site because most epidural spread is cephlad. The route of the needle from superficial to deep includes the skin, subcutaneous tissue, nuchal ligament, ligamentum flavum (although it is thin and often absent in the midline), then entry into the epidural space. Physicians avoid the IL approach if there has been surgery at the site of intended injection, especially laminectomy, given derangement of the anatomy and a higher risk of dural puncture. The most common technique includes a loss of resistance technique used to identify entry into the epidural space, which can be lost with epidural scarring. Fluoroscopy with radiopaque contrast confirms epidural placement and excludes vascular flow. Medication is then injected and postinjection washout images are taken to confirm flow of the medication to the target.
Evidence
Several retrospective and one prospective controlled study have been conducted on cervical IL ESIs for neck pain and radiculopathy performed without fluoroscopy. Success for the treatment of radiculopathy was cited at 40% to 60%. However, the rate of misplacement of a cervical IL ESI without fluoroscopic guidance has been cited as high as 53%, and these results, therefore, are difficult to interpret.
Studies on cervical IL ESIs with fluoroscopic guidance have also provided favorable evidence, although none of these are randomized controlled studies. In a prospective study of 13 patients with cervical disc herniation with neck pain and radiculopathy who had up to 3 cervical ESIs (proceeding from blind IL to fluoroscopically guided IL to fluoroscopically guided TF) all patients had resolution of symptoms at 12-month follow-up, except for one with neck pain. A retrospective study of 91 patients with neck pain and radiculopathy showed 72% achieved success, but follow-up was only 2 weeks. A study of physical therapy (and other noninterventional care) combined with cervical IL ESI with fluoroscopic guidance (only for persistent symptoms after noninterventional care) showed that 20 of 26 patients with cervical radiculopathy and disc herniation had good to excellent results. Most of these patients had neurologic deficits, yet were able to avoid surgery.
Studies have also aimed to identify which causes of cervical radiculopathy respond best to IL ESI. Kwon and colleagues showed that patients with osseous central and foraminal stenosis had less improvement than those with a disc herniation. In 2009, a retrospective study of 32 patients with cervical radiculopathy treated with fluoroscopically guided IL ESI with a catheter guided to the level of symptoms found that the presence of central canal stenosis correlated with significantly better outcome as measured by change in Neck Disability Index. Overall, it is unclear if a specific cause of cervical radiculopathy is more responsive to IL ESI.
TF Approach
Technique
The TF approach is considered to be more specific, delivering the injectate directly to the site of disease at the ventral epidural space next to the disc, the dorsal root ganglion, and the nerve root. The technique involves using fluoroscopy to identify a subpedicular target within the intervertebral foramen.
The correct oblique view of the target foramen is obtained with fluoroscopy. An entry point overlying the posterior half of the target foramen is used to pass a needle into the neck. Care is taken to ensure that the tip of the needle is positioned over the anterior half of the superior articular process to ensure that it is not inserted too far into the foramen. The needle is advanced to the superior articular process and then readjusted to enter the foramen tangential to its posterior wall, opposite the equator of the foramen. Accurate placement is confirmed in multiple planes with radiopaque contrast and fluoroscopy.
Real-time or live fluoroscopy or digital subtraction angiography is used to rule out vascular flow. The anesthetic is injected first, and a pause of 60 to 90 seconds is conducted to monitor for side effects in the central nervous system, which may be reversible (seizures, transient paresis, and respiratory depression), as an additional indicator of anesthetic intravascular injection. The medication is then injected and postinjection washout images are taken to confirm flow of the medication to the target.
Selective nerve root block
In practice and in the literature, the terms selective nerve root block (SNRB) and TF ESI are sometimes used interchangeably. The term SNRB describes a highly selective TF injection in which the interventionalist anesthetizes a single specific nerve root to confirm or refute it as the source of pain. The selective nature of the nerve root block applies if the injectate/anesthetic travels only to the target nerve root. However, it has recently been shown that with as little as 0.5 mL of contrast directed via SNRB at L4 or L5, flow to an adjacent level can be seen. With standard doses of 1 to 2 mL of anesthetic used, these injections are likely often nonselective or at least only partially selective.
Evidence
For lumbar radicular pain, 2 recent randomized controlled trials support the efficacy of TF ESI, with decreased surgical rates and decreased pain scores at 12-month follow-up. There are no randomized controlled studies to show efficacy of TF ESIs in the cervical spine. However, several case series show favorable results. Results tended to be better in those more than 50 years old and in patients with nontraumatic radiculopathy. To determine effect on surgery sparing, a small series of 21 patients with cervical radiculopathy awaiting surgery underwent 2 TF ESIs 2 weeks apart. Five of the 21 patients had excellent results at 4 months and elected not to have surgery. However, there was no control group to show if this was a better outcome than natural history alone. A recent prospective randomized trial of 40 patients with cervical radiculopathy resulting from degenerative changes, all with positive response to SNRB, did not show an increased benefit of methylprednisolone over bupivicaine alone at 3-week follow-up. Limitations of this study include that the questionnaire used was not a validated outcome measure and inclusion criteria required only 50% relief of extremity pain with the SNRB. In addition, these findings may be limited to TF ESIs for cervical radiculopathy due to degenerative causes, and better results with corticosteroids would be expected for soft disc herniations in which inflammation may play a larger role.
IL Versus TF
Injectate flow
The rationale for using a TF approach in preference to the IL approach is that it delivers the medication directly to the ventral epidural space, closer to the target disc and/or nerve root. Studies evaluating contrast patterns generally support this concept in the lumbar spine. Though, a recent analysis of contrast patterns for midline cervical IL ESIs found the rate of ventral epidural spread was 56.7% with 1 mL and 90% with 2 mL of injectate.
Evidence
Studies of lumbar TF ESIs demonstrate benefit over IL approach in the lumbar spine. Comparison studies have not been conducted in the cervical spine, although some extrapolation may be reasonable. In a study of 48 patients with cervical radiculopathy who did not improve with IL ESI, 79.2% were reported to have an effective TF ESI. In these patients who had failed IL ESI, patients with foraminal stenosis were more likely to improve than those with disc herniation. TF ESIs have a theoretic benefit over IL ESIs, and may be superior for certain causes of radiculopathy, but this has not been clearly substantiated in the cervical spine. Given the increased risk of major complications with TF ESI discussed earlier, the potential benefit must be carefully weighed for each individual patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




