In 2005, 1.6 million people were estimated to be living with limb loss; by 2050, the rate is expected to double to 3.6 million in the United States. Past data have shown that the rates of dysvascular amputations were increasing. However, recent studies looking at single diseases of peripheral arterial disease and diabetes mellitus show amputations related to these conditions are now decreasing. The authors think that it may not be a single disease process but rather the cumulative illness burden that is leading to amputations. In addition to cause, age, gender, and race continue to play a role in limb loss.
Key points
- •
In 1996, the incidence of amputations most commonly occurred because of vascular conditions and trauma.
- •
Dysvascular amputation rates were 8 times greater than trauma-related amputation rates in 1996.
- •
The number of amputations among patients with diabetes is declining, but the number of patients with diabetes is increasing because of early diagnosis.
- •
The number of amputations among elderly patients with peripheral arterial disease is declining.
- •
The combined illness burden of multiple comorbidities increases the risk of amputations.
- •
Males are at a higher risk for dysvascular and trauma-related amputations than females.
- •
Racial disparities continue to play a role in dysvascular amputation rates with certain groups; African Americans, Hispanic Americans, and Native Americans having the highest rates.
- •
Trauma- and cancer-related amputations are declining.
Despite advancements in medicine and the emphasis on disease prevention, limb loss continues to be prevalent in our society. In 2005, 1.6 million people were estimated to be living with limb loss; by 2050, the rate is expected to double to 3.6 million in the United States. Limb loss can be subdivided into 2 types, major and minor limb loss . Major limb loss is a transhumeral, transradial, transfemoral, or transtibial amputation. Minor limb loss is defined as an amputation of the hand, digits, toes, or at the midfoot level. The incidence of amputations most commonly relates to vascular conditions, trauma, malignancy, and congenital deficiency. Between the 1980s and 1990s, the amputation rates increased among dysvascular patients and declined in trauma and cancer ( Table 1 ). Contemporary studies have shown a reduction of rates in subsets of those with diabetes and peripheral arterial disease (PAD). The purpose of this review is to highlight the epidemiology of limb loss and current trends.
| Year | Dysvascular a | Trauma a | Cancer a |
|---|---|---|---|
| 1988 | 38.3 | 11.37 | 0.62 |
| 1996 | 46.19 | 5.86 | 0.35 |
| Yearly Change | +3.0% | −5.6% | −4.7% |
| Overall Change | +27.0% | −50.0% | −43.0% |
Dysvascular
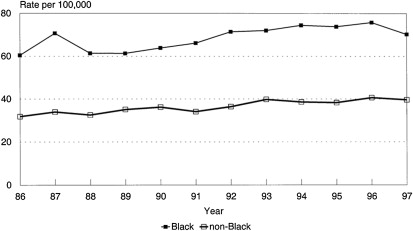
Nationally representative hospital discharge data from 1988 to 1996 from the Healthcare Cost and Utilization Project (HCUP) showed that overall, dysvascular-related amputations were increasing as reported by Dillingham, Pezzin, and MacKenzie in 2002. Increased rates were evident in levels associated with considerable functional impairments, such as the foot, transtibial, and transfemoral levels. Incidence rates of dysvascular amputations increased with age in both sexes and racial groups when comparing African Americans with non-African Americans. Men and African Americans underwent amputations at higher rates compared with Women and non-African Americans ( Fig. 1 ). The pattern was noted to be markedly higher among African Americans and women older than 85 years. African Americans older than 85 years were 11.7 times more likely than their middle-aged counterparts to undergo a dysvascular amputation. African Americans were also more likely to have amputations at higher levels than whites. A similar effect was noted among women undergoing dysvascular amputations who were older than 85 years, with a relative risk ratio of 12 compared with middle-aged women.
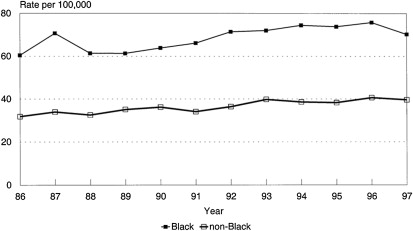
Dysvascular
Nationally representative hospital discharge data from 1988 to 1996 from the Healthcare Cost and Utilization Project (HCUP) showed that overall, dysvascular-related amputations were increasing as reported by Dillingham, Pezzin, and MacKenzie in 2002. Increased rates were evident in levels associated with considerable functional impairments, such as the foot, transtibial, and transfemoral levels. Incidence rates of dysvascular amputations increased with age in both sexes and racial groups when comparing African Americans with non-African Americans. Men and African Americans underwent amputations at higher rates compared with Women and non-African Americans ( Fig. 1 ). The pattern was noted to be markedly higher among African Americans and women older than 85 years. African Americans older than 85 years were 11.7 times more likely than their middle-aged counterparts to undergo a dysvascular amputation. African Americans were also more likely to have amputations at higher levels than whites. A similar effect was noted among women undergoing dysvascular amputations who were older than 85 years, with a relative risk ratio of 12 compared with middle-aged women.
Diabetes
Diabetes, a common comorbidity associated with dysvascular disease, affects 25.8 million people. Those patients with diabetes mellitus have an approximately 10-times higher risk of amputation compared with individuals without diabetes. Racial disparities continue to play a role in the course of diabetes. In general, the risk of diagnosed diabetes was 18% higher among Asian Americans, 66% higher among Hispanics, and 77% higher among non-Hispanic blacks compared with non-Hispanic whites. A review by Dillingham, Pezzin, and MacKenzie revealed that research has shown that among those individuals with diabetes, African Americans, Hispanics, and Native Americans are at a considerably higher risk for lower-limb loss than white people.
One objective of Healthy People 2010 was to decrease the rate of lower-extremity amputations among those individuals with diabetes. In 2000, Healthy People 2010’s goal was to decrease the incidence of amputation among patients with diabetes from 4.1 per 1000 (2000) to 1.8 per 1000 (2010). A summary of Healthy People 2010 revealed that the rate of lower-extremity amputations in patients with diabetes did in fact decline by 47% from 1997–1999 to 2005–2007. This finding was reflected in an incidence rate reduction from 6.6 per 1000 in 1997 to 3.5 per 1000 population in 2005 (age adjusted). Additionally, females had a lower rate (2.2 per 1000 population [age adjusted]) of lower-extremity amputations than males (4.8 per 1000) in 2005 to 2007. Because of the decline in the rate of amputations among patients with diabetes and its positive implications on health policy, this objective is maintained as a goal for Healthy People 2020.
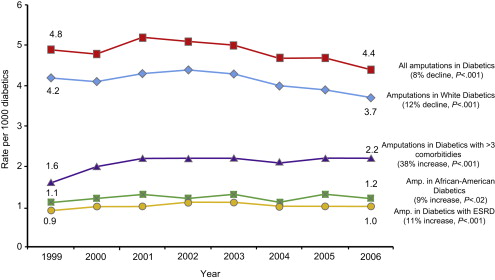
Goldberg and colleagues (2012) evaluated the effect of the Healthy People 2010 initiative in an enhanced sample of all patients with diabetes from the Medicare 5% sample during 1999 to 2006. They found that the amputation rate declined among patients with diabetes. However, the incidence of amputations among patients with diabetes with greater than 3 comorbidities and end-stage renal disease (ESRD) increased from 1999 to 2006 ( Fig. 2 ). This finding offers the perspective that perhaps it is not just a single comorbid condition but rather the combined illness burden from multiple conditions that leads to amputation. Eggers and colleagues (1999) reported from Medicare data that patients with diabetes and ESRD had a 10-fold greater risk of amputation than those with diabetes mellitus without ESRD. This finding suggests that a greater illness burden has serious implications to health care policy beyond the prevention of single diseases.