Fractures of the humeral shaft are common in low-energy and high-energy trauma, and optimal clinical management remains controversial. Nonsurgical management has been supported as the preferred treatment based on high union rates and minimal functional deficit due to a rich vascular supply from overlying muscle and the wide motion available at the glenohumeral joint. Recent studies of nonoperative management have challenged surgeons’ understanding of these fractures and the perception of favorable outcomes. Current considerations support expanded operative indications with traditional open-plate fixation and with the use of minimally invasive techniques, implants, and a reconsideration of intramedullary nailing.
Key Points
- •
Surgical indications for humeral shaft fractures are expanding.
- •
Elderly, osteoporotic humeral shaft fractures are becoming more common.
- •
Use of a plate or nail for fixation depends on fracture and patient characteristics as well as surgeon preference.
- •
Minimally invasive anterior plating has favorable outcomes.
- •
Most radial nerve palsies can be observed.
- •
Nonunion and bone defect management must consider the severity of initial injury, time since injury, patient comorbidities, and healing response to date.
Introduction
Fractures of the humeral shaft are common fractures in low-energy and high-energy trauma, and optimal clinical management remains controversial. Nonsurgical management has been supported as the preferred treatment based on high union rates and minimal functional deficit due to a rich vascular supply from overlying muscle and the wide motion available at the glenohumeral joint. Historically, surgical treatment, usually via plate fixation, has been less common outside of some very specific clinical situations, such as open fractures, ipsilateral forearm fractures, and fractures with concomitant vascular injuries. Recent studies of nonoperative management have challenged surgeons’ understanding of these fractures and the perception of their favorable outcomes. Current considerations support expanded operative indications with traditional open-plate fixation as well as with the use of new minimally invasive techniques, new implants, and a reconsideration of intramedullary nailing.
Introduction
Fractures of the humeral shaft are common fractures in low-energy and high-energy trauma, and optimal clinical management remains controversial. Nonsurgical management has been supported as the preferred treatment based on high union rates and minimal functional deficit due to a rich vascular supply from overlying muscle and the wide motion available at the glenohumeral joint. Historically, surgical treatment, usually via plate fixation, has been less common outside of some very specific clinical situations, such as open fractures, ipsilateral forearm fractures, and fractures with concomitant vascular injuries. Recent studies of nonoperative management have challenged surgeons’ understanding of these fractures and the perception of their favorable outcomes. Current considerations support expanded operative indications with traditional open-plate fixation as well as with the use of new minimally invasive techniques, new implants, and a reconsideration of intramedullary nailing.
Characteristics and diagnosis
Anatomically, the humeral shaft is the area between the proximal pectoralis major insertion and the distal metaphyseal flare. Fracture in this area presents with displacement and angulation that is representative of the energy involved and the pull of the muscular attachments above and below the fracture. On presentation, a history is initiated with emphasis on hand dominance, type of work or hobby, and mechanism of injury. Low-energy mechanisms should heighten suspicion of pathologic fracture through tumor or metabolic disease. High-energy injuries should warrant higher suspicion for open fractures and compartment syndrome and further investigation for associated injuries to the lung, ribs, clavicle, scapula, brachial plexus, and axillary artery. A focused history should identify modifiable factors that influence healing, such as smoking and other medical comorbidities. Physical examination of the shoulder and upper extremity is paramount to assess the soft tissue injury and possible neurovascular sequelae. A detailed motor examination documenting active wrist extension must be verified as radial nerve palsy following fracture has an incidence of 6% to17%. Radial nerve injury is most common with transverse middiaphyseal fractures. It is important not to accept digital extension as evidence of radial nerve function because hand intrinsics from the ulnar nerve can perform this function as well. In proximal shaft fractures, lateral shoulder skin sensation and the ability to push the elbow into the torso can be used to assess the axillary nerve. Standard orthogonal radiographs of the shoulder, humerus, and elbow should be obtained. With proximal or distal fractures, any suspicion of articular extension should be further evaluated with CT imaging. Initial management is aimed at pain control and immobilizing the fracture and can usually be achieved with a coaptation splint, sling and swath, or shoulder immobilizer. Acute functional bracing is becoming more common because it offers patients the immediate advantage of hygiene control and potential elbow motion once pain subsides.
Management
Most isolated humeral shaft fractures have been historically treated without surgery. In most patients, this fracture will heal predictably without surgical intervention because it is a well-vascularized bone encapsulated by muscle. Using a functional brace, Sarmiento and colleagues reported a union rate of 97% in 620 subjects, including 94% union in low-grade open fractures. The high union rates coupled with the shoulder’s ability to compensate for moderate degrees of deformity has traditionally made nonoperative treatment a reasonable first option in many patients. The limits of acceptable reduction are considered to be 20° of sagittal plane angulation, 30° of coronal angulation, 15° of malrotation, and 3 cm of shortening. These standards are historical, however, and the degree of disability was based on a sample of 32 subjects, only two of which had a malrotation deformity, and no objective measures were used. Functional bracing maintains fracture alignment through gravity and soft tissue compression.
Enthusiasm for functional bracing has been challenged with recent observations of permanent loss of motion and a higher than expected nonunion rate of 10%. Specific fracture patterns, most notably transverse and proximal-third oblique fractures, may have unacceptably higher rates of nonunion. Further, certain injury and patient factors make functional bracing less likely to succeed. These include plexus injury, in which muscle contractility around the fracture is lost and cannot provide the essential compression to maintain fracture alignment and prevent distraction, and morbid obesity, in which effective bracing technique is difficult and excess tissue often creates frontal plane malalignment.
Absolute indications continue to be open and pathologic fractures, associated vascular injuries requiring repair, brachial plexopathy, severe soft tissue injury precluding closed treatment, associated articular injury of the shoulder or elbow, and ipsilateral operative forearm fracture. Relative indications are guided by patient and fracture factors, in addition to associated injuries. By discussing this with patients and understanding the demands of their lives, surgeons are able to make individual recommendations for conservative versus surgical management. Frequently, multiply injured patients with humeral shaft fractures and, occasionally, isolated shaft fractures in patients who need rapid return to function are treated surgically. Surgical management can allow immediate full range of motion, pain control, early rehabilitation, and return to work. However, risks of radial nerve palsy, reoperation, infection, anesthetic risk, bleeding, and nonunion must be discussed and accepted by the patient before proceeding.
External fixation
Use of external fixation is generally limited to damage control situations in which patients are unable to physiologically tolerate extensive surgical intervention. Additional indications include associated soft tissue injury requiring multiple debridements or frequent dressing changes, vascular injuries requiring bony stabilization before repair, and joint instability. Risks with external fixation include pin loosening, infection, lost motion, refracture, malunion, and nonunion. The radial nerve is also at risk during distal percutaneous pin insertion. A recent study of 40 cadaver upper extremities, demonstrated four radial nerve injuries and nine pins with direct contact with the nerve during percutaneous pin insertion. The investigators recommended larger incisions with blunt dissection to the lateral humeral cortex, finger palpation for the nerve, and retraction of tissues during pin insertion to avoid injury.
In damage control situations, once the patient is hemodynamically stable, consideration must be given to definitive management. This often requires conversion to an internal fixation construct and associated debridement and wound coverage in injuries with soft tissue compromise. A retrospective study was done of 17 humeral shaft fractures initially treated with damage-control external fixators that were converted to plates at an average of 6.2 days; 14 days was the longest duration. Eighty-eight percent healed. Two subjects developed infections requiring debridement and conversion back to external fixation. Their failure was attributed to poor compliance and severity of initial injury. Conversion to plate was thought to be safe within 2 weeks. There are no data to suggest a safe time point for conversion to an intramedullary nail.
Intramedullary nailing
Intramedullary nailing of long-bone fractures has been very effective in the lower extremities but historically limited in the upper extremity owing to concerns of shoulder and elbow dysfunction, nonunion, and reoperation. Further, there is long-standing concern regarding stiffness from capsular adhesion, pain, and fracture at joints adjacent to start sites on antegrade and retrograde nails. The theoretical benefits are significant and include smaller incisions, maintenance of fracture hematoma, and an implant that is load-sharing and can be used to ad lib immediately. Indications for intramedullary fixation have been narrower than plate fixation and include fractures with associated soft tissue injury precluding an open approach, pathologic fractures, extreme osteopenia, and true diaphyseal segmental patterns.
Recent advances in technique, implants, surgeon experience, and improved study design have renewed interest in intramedullary nailing. The anterolateral acromial approach using the interval between the anterior and middle deltoid raphe leads to better visualization of the rotator cuff, making it easier to identify the rotator interval itself and pinpoint the start site. Moreover, the start site with this approach is more collinear with the intramedullary canal, making it technically easier to avoid varus malalignment and to achieve medial calcar contact ( Fig. 1 ). It also allows for protection of the anterior branch of the axillary nerve during placement of proximal interlocking bolts. With respect to the start site on the humerus, translation of the entry site medially onto the articular surface will avoid the common deformity of medial shaft displacement with nail passage.
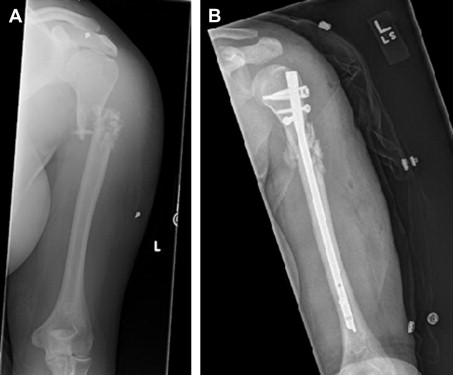
Nails today are larger, more rigid, anatomically-contoured, and statically locked with multiple proximal and distal interlocks. They share load with the bone and avoid stress shielding. Use of newer nails with minimal reaming has been shown to reduce nonunion and implant failure. Patients with native isthmus diameters of 9 mm or greater are good candidates for nails because they can accommodate a larger nail with minimal reaming. New designs with more points of fixation have expanded the level of proximal and distal fractures that can be nailed. There is increasing interest in straight proximal nails with a more articular, on-axis start site. These are optimal for proximal fractures and assist in avoidance of frontal plane malalignment. Many of these nails have multiple proximal locking options and the ability to achieve angular stability with the interlocking screws ( Fig. 2 ). As a result, use of intramedullary nails have increased and, as surgeons have become more comfortable with the technique and radiographic interpretations during the surgery, common complications, such as subacromial impingement due to prominent nails, rotator cuff tears due to poor technique during canal access, and serial reaming, have become less common.
Many technical tricks during intramedullary nailing can be used to avoid complications. One such priority is protection of the radial nerve. Pushing the reamer across the fracture site protects the radial nerve from the reamer itself and from thermal injury. Isolating the nerve through a small, separate incision and directly visualizing it during canal reaming is also possible and reassuring ( Fig. 3 ). To avoid a prominent proximal nail tip and achieve fracture site compression, countersinking the nail by 3 to 4 mm and backslapping to cortical contact or using new nail designs that allow for interfragmentary compression after distal interlocking has decreased the number of nonunions. For proximal humeral shaft fractures undergoing antegrade nailing, restoration of the medial column prevents loss of reduction, screw penetration into the glenohumeral joint, and lost humeral head height. This reduction can be attained by tagging the rotator cuff tendons and placing two 2 mm Kirschner wires into the humeral head and using these as joysticks to control sagittal and coronal alignment. A Kirschner wire, outside of the expected path of the nail, can then be placed across the fracture for provisional stabilization. A recent review of 48 subjects treated with a contemporary antegrade humeral nail demonstrated 96% union in a mean time of 10 weeks, five required reoperation for nonunion, loose hardware, and infection. Ninety-one percent had excellent or good shoulder function. In another study, 94% of subjects went onto uncomplicated union with good functional outcomes. This study highlighted that most complications are the result of surgeon technical error and not limitations of the nailing technique. In addition, the investigators noted that younger subjects had better shoulder outcomes than elderly subjects did. Despite the worse outcomes, elderly subjects tolerated their deficits well because of their lower functional requirements. Healing and acceptable functional results seem possible with precise technique. Improved recognition of technical issues, such as placement of the entry site, fracture site compression, and understanding newer implant options, is imperative for treatment success.
Antegrade nailing is favored in North America, but there is persistent regional interest in locked retrograde nailing technique. Retrograde nails can be used for fractures in the distal-third and middle-third of the humerus in patients with shoulder abduction greater than 60°. A new technique with the patient supine, using a radiolucent arm table and the elbow fully flexed, splits the triceps tendon and establishes the nail entry point between the supracondylar ridges through the superior aspect of the olecranon fossa ( Fig. 4 ). This entry site provides straighter access to the canal and remains clear of the olecranon tip of the ulna during full elbow extension. The proximal insertion of the nail is generally to about 1.5 cm below the humeral head articular surface. A large enough entry site is crucial in retrograde nailing because unforceful introduction of the nail avoids iatrogenic supracondylar fractures. Reaming is not necessary as long as a rigid nail can be passed. However, it is recommended to ream 2 mm larger than the nail at the insertion and 1.5 mm larger in the isthmus and proximal humerus to avoid supracondylar fracture. A study of 16 subjects using this technique reported no iatrogenic fractures. Although useful in preventing bending moments and nail incarceration, canal reaming weakens the humerus and does not prevent deformity from off axis entry sites. The bony anatomy of the distal humerus makes it necessary to remove more bone to accommodate current nail designs. Avoidance of the creation of a scenario of bone loss and supracondylar humerus fracture in a poorly performed retrograde nail is critical.







