Elbow Replacement for Acute Trauma
Srinath Kamineni
Harikrishna Ankem
DEFINITION
Most comminuted elbow fractures have associated soft tissue injuries, which are often of equal or greater importance to the bony injury.
The goal when treating acute elbow fractures is that of anatomic open reduction and internal fixation (ORIF) with management of any soft tissue injuries.
An acute elbow arthroplasty should be considered only if ORIF is unlikely to achieve a predictably good functional outcome in the older age groups.
In the majority of cases, elbow replacements for the treatment of acute fractures should be limited to the physiologically elderly patient with low functional demands.
ANATOMY
The bony anatomy of the elbow consists of the distal humerus, proximal ulna, and proximal radius.
Important soft tissue stabilizers include the medial and lateral ligamentous complexes and surrounding musculature, especially the brachialis, common flexor and common extensor masses, and triceps.
The ulnar nerve is tethered to the medial condylar-epicondylar fragment by the cubital tunnel retinaculum distally and the arcade of Struthers proximally.
PATHOGENESIS
Elbow injuries are often the result of direct impact—for example, a direct blow on the elbow during a fall.
Knowing the energy of the fracture is important to gauge the likelihood of associated injuries.
Less energy is required to create a comminuted fracture in elderly and osteoporotic individuals, but muscular injuries of the triceps and brachialis are common, with a subsequent influence on the functional outcome.
The ulnar nerve displaces with the medial fragment. As a consequence, the nerve may kink, leading to a local nerve injury. Nerve lacerations are an uncommon consequence of comminuted distal humeral fractures.
NATURAL HISTORY
Most distal humeral fractures are treatable with either nonoperative management or ORIF. Challenging fracture subgroups include fractures that involve articular surfaces and are highly comminuted, although younger patients (younger than 65 years old) are generally not considered candidates for total joint replacements, partial joint replacements are an emerging solution.22
Many direct and indirect soft tissue complications may ensue, including neurovascular entrapment,8,12 muscle tears leading to myositis ossificans,12,18,23 and soft tissue contracture with joint stiffness.
There is some evidence to suggest that congruently reducing and fixing a comminuted intra-articular distal humeral fracture does not eliminate the risk of posttraumatic arthritis,13 although, where possible, ORIF with anatomic congruity should remain the primary goal.
PATIENT HISTORY AND PHYSICAL FINDINGS
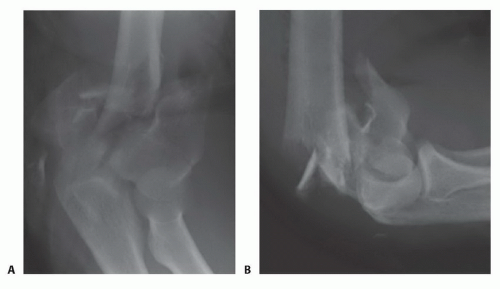
The physical examination (FIG 1) should be performed gently in the presence of fractures, especially when comminution suggests the possibility of neurovascular injury.
A complete examination of the elbow should also include evaluation of associated injuries. It should begin away from the elbow, progressing toward it, for example, shoulder/wrist with progression toward the elbow.
The following associated injuries should be ruled out:
Distal radial and scaphoid fractures: Because the most common mechanism of injury is a fall onto an outstretched hand, the energy transfer of the fall begins in the extended wrist, through the distal radius and scaphoid. Direct palpation of the distal radius should be done, and anatomic snuffbox tenderness should be elicited. Palpation of the
scaphoid tubercle and ulnar and radial deviation of the wrist may also identify a scaphoid injury.
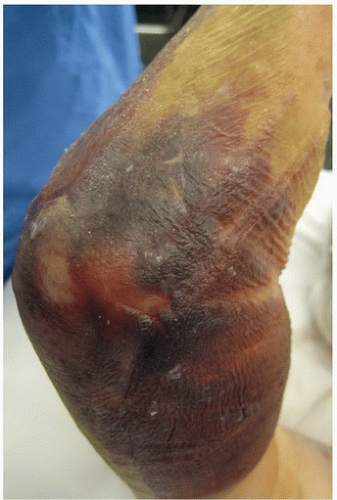
FIG 1 • Typical appearance of an elbow with an underlying fracture with extensive swelling and bruising.
Distal radioulnar joint disruption: Ballottement of the ulnar head should be done in the volar and dorsal directions, in pronation and supination. A disrupted joint is often painful with such ballottement, and the ulnar head may be prominent with the forearm in pronation.
Fracture extension beyond the elbow: The examiner should palpate the ulnar shaft, along its subcutaneous border, from the wrist to the olecranon.
Interosseous membrane injury: Palpating the interval between the bones of the forearm is not a sensitive examination but can raise suspicion for an Essex-Lopresti injury, leading to further imaging. If an interosseous membrane disruption is present, this will influence the type of implant used for elbow replacement (one with a radial head replacement), but the pathology is not commonly described.
IMAGING AND DIAGNOSTIC STUDIES
Plain radiographs, including anteroposterior (AP) and lateral views (FIG 2) of the elbow and both wrists, should be obtained. The elbow view may have to be taken in a protective splint or plaster backslab for patient comfort.
Elbow radiographs will allow initial assessment of the degree of comminution and may indicate the presence of decreased bone mineral density.
Bilateral wrist views will indicate the presence of an axial (interosseous membrane) injury if the ulnar head is in positive variance compared to the contralateral uninjured wrist.
Plain tomograms are of use in improving the understanding of the fracture configuration, but an alternative would be a computed tomography (CT) scan. With the latter, the surgeon can view a three-dimensional reconstruction, which is a useful surgical planning tool for ORIF.
If there is evidence on physical examination of a neurologic injury, it is prudent to document its extent with a carefully performed neurologic examination.
DIFFERENTIAL DIAGNOSIS
Nonunion
Ligamentous disruption
Fracture-dislocation
NONOPERATIVE MANAGEMENT
The “bag-of-bones” technique is a nonoperative method of treatment described by Eastwood7 that encourages the compressive molding of the comminuted distal humeral fracture fragments.
Subsequent rehabilitation with collar and cuff support achieves substandard but acceptable results only in the elderly and debilitated group of patients who have almost no demand on elbow function.
This type of treatment does not achieve acceptable results with respect to stability and strength in younger patients.
SURGICAL MANAGEMENT
Open Reduction and Internal Fixation
ORIF has been widely documented for comminuted fractures of the distal humerus.
Some reported series demonstrate good results with fixation of such challenging fractures, with better results predominantly in the younger age groups.19,24 Rarely are good results achieved in the elderly, osteoporotic group.13
Many series report less than satisfactory outcomes in the elderly treated by operative fixation.19
A direct comparison of internal fixation to primary total elbow replacement in the elderly osteoporotic group revealed that replacement produced no poor results and no need for revision surgery at 2 years of follow-up. The internal fixation group produced three poor results requiring revision to a total elbow replacement.10
Elbow Arthroplasty
When a distal humerus fracture is not reliably reconstructable, arthroplasty becomes a valid treatment option.
Elbow replacement following a failed attempt at fixation has proven to have a significantly worse outcome than if the arthroplasty was performed initially.9
There are a number of studies that support the concept of an acute total elbow arthroplasty in select patients with comminuted fractures of the distal humerus.6,9,16
The more traditional form of replacement for the elderly and low-demand population with an unreconstructable distal humerus fracture is the total elbow arthroplasty.
A more recent innovation has been the replacement of the distal humerus (hemiarthroplasty) to preserve an intact ulna and radial head.20 This procedure is not U.S. Food and Drug Administration (FDA) approved and so should be considered experimental and not for general consideration, especially because the elbow joint is variable and highly congruent in its topography, which differs from many of the standard implants used for acute fractures. However, there is a definite place within the algorithm of acute fracture management for such a surgical technique and implant and is still available outside the United States for this indication.
Indications and Contraindications (Total Elbow Arthroplasty)
Indications for acute total elbow arthroplasty
Comminuted, unreconstructable distal humerus fracture
Physiologically elderly patient
Low-demand patient
Poor quality/injured cartilage of ulna
Absolute contraindications for acute joint replacement (total or hemi)
Infection (overt)
Lack of soft tissue coverage (skin, muscle)
Relative contraindications for acute joint replacement
Infection in distant body part
Contaminated wound
Neurologic injury involving the elbow flexors
Indications and Contraindications (Distal Humeral Hemiarthroplasty)
Indications for acute elbow hemiarthroplasty
Unreconstructable distal humeral fracture (C3)
Unreconstructable combined fractures of capitellum and trochlea
Well-preserved cartilage of ulna
Very low bicondylar T fracture of distal humerus
Young patient
Active patient
Repairable or intact collateral ligaments (may require reconstruction of the medial and lateral supracondylar columns)
Repairable or intact radial head
Contraindications for acute elbow hemiarthroplasty
Unreconstructable medial/lateral columns
Articular damage to greater sigmoid notch (ulna)
Osteoporotic/osteopenic ulna (relative)
Preoperative Planning
Standard radiographs should be obtained (AP and lateral).
If doubt exists regarding the ability to anatomically repair the fracture, then a CT scan should be requested to assess the degree of comminution and the fracture line orientation.
An assessment of humeral shaft bone loss is important in planning the implant design that might be considered. If the degree of loss is greater than the articular condylar fragments, an implant that has the ability to restore humeral length will be more appropriate. If an unreconstructable fracture of the humeral articular surfaces without humeral shaft bone loss is encountered, an implant with the ability to resurface the articular surfaces as a hemiarthroplasty or a resurfacing ulnotrochlear replacement can be considered, but the former implantation technique should be regarded as an off-label and experimental procedure.
Humeral shaft length loss of 2 cm can be tolerated and standard implants used.
Humeral shaft length loss of greater than 2 cm can be restored with implant designs with anterior flanges, especially those with extended flanges that allow restoration of humeral length.
The surgeon should assess the intramedullary canal dimensions of the humerus and ulna. This will help to plan the requirement of extra small diameter.
Neurovascular status of the limb should be fully assessed and documented in the clinical notes.
Patient Positioning
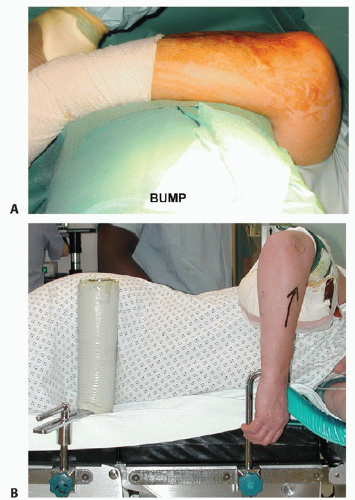
Two methods of patient positioning can be used, depending on surgeon comfort and the access required.
Supine: The arm is draped for maximum maneuverability. During the procedure, the arm is supported on a large rolled towel placed on the patient’s upper thorax, carefully avoiding the endotracheal tube, stabilized by an assistant. In this position the surgeon stands on the side of the patient’s injured limb (FIG 3A).
Lateral decubitus: The arm is positioned on an arm support, thereby minimizing the need for an assistant, but this setup is less maneuverable. In this position, the surgeon stands on the opposite side of the patient’s injured limb (FIG 3B).
Surgical Approach
Two main surgical approaches are useful for acute total elbow arthroplasty:
“Triceps on” (eg, Alonso-Llames, paratricipetal)
“Triceps off” (eg, Bryan-Morrey)
The triceps should be carefully managed in either approach, and it often has a thin tendon, especially in older patients and those with rheumatoid arthritis. The triceps tendon should be dissected from the olecranon with a small curved scalpel blade, maintained perpendicular to the interface between the tendon and bone.
TECHNIQUES
▪ Incision and Dissection
Make a midline longitudinal skin incision (TECH FIG 1A), with a gentle curve to avoid the olecranon weight-bearing prominence. Extend the incision 5 cm distal to and proximal to the prominence of the olecranon tip.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree