Elbow Instability: Arthroscopic Management Options and Medial Collateral Ligament Reconstruction
Christopher C. Dodson
David W. Altchek
Excessive valgus and extension forces are generated during the throwing motion in several sports, most notably baseball, tennis, football, and certain track and field events (1). The repetition required to excel in these sports can ultimately lead to fatigue and even failure of key stabilizing structures in the elbow. The medial ulnar collateral ligament (MUCL) is the primary restraint to valgus load during the throwing motion and is most susceptible to injury after repetitive throwing. MUCL insufficiency leads to valgus instability, a condition that is only significant in overhead athletes. Overtime, chronic valgus instability can result in a unique constellation of elbow pathologies that are indicative of repetitive overhead throwing.
The most common injuries seen in the elbow of the throwing athlete are MUCL injuries, ulnar neuritis, posteromedial impingement/osteophyte formation, flexor-pronator strain, ulnar stress fractures, osteochondritis dissecans of the capitellum, and capsular contracture (2, 3, 4 and 5). Although not all pathology in the thrower’s elbow is amenable to arthroscopic management, it is essential that any clinician who cares for throwing athletes be familiar with all pathologic conditions and comfortable with both open and arthroscopic treatments.
Over the past decade, clinicians have gained a better understanding of the complex interplay between the dynamic and static stabilizers of the elbow. Furthermore, the desire for minimally invasive treatment of these conditions has led to the development of advanced techniques and instrumentation for elbow arthroscopy. This discussion will be limited to the arthroscopic treatment of common elbow injuries in throwing athletes, including those that can be managed entirely arthroscopically as well as in conjunction with a common open procedure for valgus instability (i.e., MUCL reconstruction).
ANATOMY/PATHOANATOMY
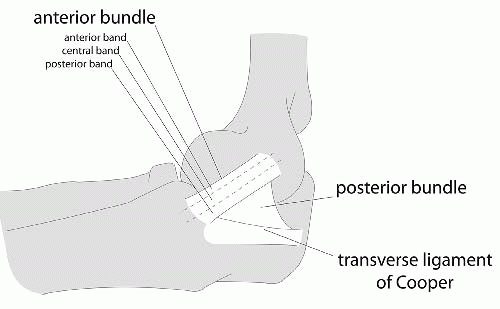
The elbow is a hinge joint with the bony ulnohumeral articulation providing stability at the extremes of motion, from 0° to 20° of flexion and beyond 120° of flexion (2). The intervening 100°, which is the primary arc of motion used in overhead throwing, relies progressively on the static and dynamic soft tissue restraints to provide stability. The anatomy of MUCL has been well described; it is actually not a single ligament but rather a complex consisting of an anterior bundle, a posterior bundle, and a transverse component (Fig. 37.1). The anterior bundle is the most well-defined structure and originates on the medial epicondyle and inserts on the sublime tubercle. The anterior bundle is subdivided into three components: an anterior band, a central band, and a posterior band. The anterior and posterior bands tighten in a reciprocal manner during flexion and extension, respectively. The posterior bundle is a less distinct fan-shaped structure, and the transverse ligament is the least distinct anatomic structure and provides very little stability to the elbow, because it does not cross the joint. Biomechanical studies have demonstrated that the anterior bundle is the primary constraint to valgus stress about the elbow; the anterior band of the anterior bundle provides most of the stability from 30° to 90° of flexion, whereas the posterior bundle becomes functionally significant between 60° and maximum flexion (6, 7).
The mechanics of overhead throwing, particularly pitching, accounts for the various pathologies seen in overhead athletes. Valgus forces have been estimated to reach 64 N during the late cocking and early acceleration phases of throwing (3, 4 and 5). After the early and late cocking phases, the elbow goes from rapid flexion to extension, and the tangentially directed forces produce a valgus and extension moment, with resulting tensile forces across the medial side of the elbow, compressive forces across the lateral aspect of the joint, and shear forces in the posterior compartment (3, 4 and 5). The repetitive stress on the MUCL eventually leads to attenuation and ultimately rupture, resulting in an insufficient ligament complex, abnormal valgus rotation of the elbow, and
instability. The term valgus extension overload describes this phenomenon (8). As the athlete continues to throw with instability, the valgus overload is accentuated and excessive valgus moments lead to stretch of other medial structures, resulting in ulnar neuritis, flexor-pronator tendonopathy, or medial epicondyle apophysitis in the skeletally immature patient. Corresponding overload on the lateral side of the elbow may lead to radiocapitellar chondromalacia, osteophyte formation, and loose bodies. Finally, during extension, posterior shear forces can produce olecranon osteophytes at the posteromedial tip with a corresponding “kissing lesion” on the posteromedial trochlea (3). It is imperative that the clinician who treats throwing athletes be familiar with these various pathologies and possess a high index of suspicion for underlying MUCL insufficiency as the etiology for many of these disorders because treating the pathology alone, without ligament reconstruction, will often fail to relieve the athletes’ symptoms and to allow them to return to sport.
instability. The term valgus extension overload describes this phenomenon (8). As the athlete continues to throw with instability, the valgus overload is accentuated and excessive valgus moments lead to stretch of other medial structures, resulting in ulnar neuritis, flexor-pronator tendonopathy, or medial epicondyle apophysitis in the skeletally immature patient. Corresponding overload on the lateral side of the elbow may lead to radiocapitellar chondromalacia, osteophyte formation, and loose bodies. Finally, during extension, posterior shear forces can produce olecranon osteophytes at the posteromedial tip with a corresponding “kissing lesion” on the posteromedial trochlea (3). It is imperative that the clinician who treats throwing athletes be familiar with these various pathologies and possess a high index of suspicion for underlying MUCL insufficiency as the etiology for many of these disorders because treating the pathology alone, without ligament reconstruction, will often fail to relieve the athletes’ symptoms and to allow them to return to sport.
CLINICAL EVALUATION
History
A comprehensive patient history is crucial to developing a differential diagnosis for recalcitrant elbow pain and disability in the throwing athlete. The nature, mechanism, acuity of onset, and symptoms associated with the pain or injury are important factors to elucidate, as with any chief complaint. In addition, the phase of throwing and any change in accuracy, velocity, stamina, or strength can help provide information about the specific diagnosis. Pain during the late cocking phase on the medial side of the elbow can indicate MUCL insufficiency. Young throwing athletes with OCD lesions often report progressive lateral elbow pain during the late acceleration and follow-through phases, with the loss of extension and episodes of locking. A history of mechanical symptoms, such as locking or catching, and posterior pain exacerbated by forced extension are also important as these symptoms may be caused by loose bodies, chondral flaps, or posteromedial impingement.
It is of utmost importance to inquire about ulnar nerve symptoms not only because this can be a source of elbow pain in the throwing athlete, but also because it is vulnerable to arthroscopic injury. Sharp pain radiating down the medial portion of the forearm with paresthesias in the fifth digit and in the ulnar-innervated half of the fourth digit can indicate ulnar neuritis. When these symptoms are associated with a snapping or popping sensation, ulnar nerve subluxation may be the cause. It is critical to make the diagnosis of a subluxating ulnar nerve because it is a risk factor for injury when making and utilizing medial portals during elbow arthroscopy.
Physical Examination
The physical examination of the elbow begins with cervical spine and includes the ipsilateral shoulder and the contralateral elbow, followed by examination of the involved elbow. Neurovascular assessment of the involved extremity, including motor and sensory testing and reflexes, is equally important.
Inspection of the elbow begins with an assessment of the resting position of the elbow and its carrying angle. A normal carrying angle is approximately 11° of valgus for men and 13° of valgus for women (2). An increase in the carrying angle of further valgus may indicate an adaptation to the repetitive stress of valgus instability. Angles of greater than 15° in professional pitchers have been documented in the literature (9). Next the lateral, posterior, medial, and anterior regions of the involved elbow should be examined for any swelling, obvious deformity, scars, or signs of previous trauma.
Following careful inspection, the four regions of the elbow should be palpated in an orderly fashion. The patients’ history generally guides the examiner toward a specific location, but palpating all four anatomic regions ensures that concomitant pathology is not missed. The medial region of the elbow is often a focus when examining throwing athletes. Tenderness on the medial epicondyle and flexor-pronator mass can suggest an avulsion fracture (adolescents) or flexor-pronator tendonosis (adults). The patient with tendonosis will exhibit local tenderness and pain with resisted flexion and forearm pronation. The MUCL can be palpated under the mass of the flexor-pronator origin when the elbow is flexed greater than 90° at its insertion at the sublime tubercle; tenderness to palpation at this location can be indicative of MUCL insufficiency. In the posteromedial region of the elbow, the ulnar nerve is easily palpable in the groove, which is located between the medial epicondyle and the olecranon. The examiner should test not only for a Tinel’s sign but also for hypermobility. This is done by palpating the nerve as the elbow is brought from extension to terminal flexion to determine whether the nerve subluxates or completely dislocates over the medial epicondyle. Palpation of
the posteromedial region of the elbow should also focus on the olecranon, which can reveal osteophytes or swelling, which are present in the throwing athlete with valgus extension overload syndrome. The medial subcutaneous border of the olecranon should also be palpated for tenderness, which in the throwing athlete, can be caused by a stress fracture (10). Lastly, examination of the lateral region of the elbow begins with palpation of the lateral epicondyle. Tenderness directly over the epicondyle is consistent with lateral epicondylitis; tenderness directlyover the anconeus soft spot can indicate a symptomatic lateral plica, a condition that is commonly found in throwing athletes. In a recent study, this was the most reproducible finding in a group of patients who were treated for this condition (11).
the posteromedial region of the elbow should also focus on the olecranon, which can reveal osteophytes or swelling, which are present in the throwing athlete with valgus extension overload syndrome. The medial subcutaneous border of the olecranon should also be palpated for tenderness, which in the throwing athlete, can be caused by a stress fracture (10). Lastly, examination of the lateral region of the elbow begins with palpation of the lateral epicondyle. Tenderness directly over the epicondyle is consistent with lateral epicondylitis; tenderness directlyover the anconeus soft spot can indicate a symptomatic lateral plica, a condition that is commonly found in throwing athletes. In a recent study, this was the most reproducible finding in a group of patients who were treated for this condition (11).
Range of motion should be assessed for elbow flexion/extension and forearm supination/pronation, as well as the nature of the extension and flexion end points. Normal extension terminates in the firm sensation of the posterior bony articulation making contact in the olecranon fossa, and normal flexion terminates in the abutment of the soft tissues of the distal humerus and the proximal forearm. Variations in the normal end points particularly a bony end-feel in extension can be indicative of pathology such as posterior osteophytes. The examiner should focus on the end-feel at extension and not necessarily on motion itself; elbow flexion contractures can be a normal physical examination finding in high-level throwers and is not necessarily indicative of injury.
Evaluation of medial stability is the cornerstone of the assessment of the overhead athlete with valgus extension overload. Multiple techniques have been described in the literature for the optimal assessment of medial elbow stability. We typically find the valgus stress test and the moving valgus stress test to be the most specific and do both provocative maneuvers when examining throwing athletes. To perform the valgus stress test, the examiner places the patient’s distal forearm under the axilla and applies a valgus load to the elbow in 30° of flexion (Fig. 37.2). The absence of a distinct endpoint combined with pain and/or tenderness indicates a positive test and insufficiency of the anterior band of the anterior bundle of the MCL. The moving valgus stress test, as described by O’Driscoll et al. (12), is performed with the patient in an upright position and the shoulder abducted 90° (Fig. 37.3). Starting with the elbow in full flexion and the shoulder in maximal external rotation, the elbow is quickly extended while a constant valgus torque is maintained. For an examination to be positive, the pain generated by the maneuver must reproduce the medial elbow pain that the patient has with activities, and the pain should be maximal between the position of late cocking (120°) and early acceleration (70°) as the elbow is extended. Other relevant tests in the throwing athlete include the radiocapitellar compression test for osteochondritis dissecans of the radiocapitellar joint, the clunk test for posterior olecranon impingement, and the flexion-pronation test to detect a symptomatic snapping lateral plica. The radiocapitellar compression test is performed by placing the elbow in full extension and loading the joint with supination and pronation to produce mechanical symptoms. The clunk test for posterior olecranon impingement is simply stabilizing the upper arm and bringing the elbow into extension to produce posterior elbow pain (Fig. 37.4). The flexion pronation test is performed by placing the arm in maximum pronation and then passively flexing the elbow to approximately 90°, which will cause snapping in a positive test (11). Lastly, we reemphasize the importance of examining the ulnar nerve for subluxation, as many patients will be unaware of this “normal” variant.
Diagnostic Imaging
The routine preoperative radiographic evaluation of the elbow include AP, lateral, and oblique views. Stress views may be helpful in assessing ligamentous laxity and olecranon axial views at 110° of flexion may reveal posteromedial osteophytes in valgus extension overload syndrome. However, it has been our experience that a true lateral of the elbow in hyperflexion is adequate to diagnose posteromedial osteophytes. Contralateral comparison imaging studies of the elbow are helpful when evaluating elbow joint laxity and when trying to distinguish true growth disturbances from variant ossification centers in the pediatric
population. CT scans can be helpful when trying to assess suspected bony pathology including stress fractures and avulsion fractures.
population. CT scans can be helpful when trying to assess suspected bony pathology including stress fractures and avulsion fractures.
MRI remains the gold standard for the evaluation of the soft tissues about the elbow, including ligamentous injury, tendinopathy, and lesions of the articular cartilage. The accuracy of MRI in the evaluation of subtle MCL injuries and the role of arthrography and contrast remain controversial. At our institution, we use a noncontrast MRI with specially designed sequences (Fig. 37.5). Potter et al. (13) have demonstrated a high sensitivity and specificity in detecting ligamentous, soft-tissue, and cartilaginous injuries using this technique. This technique maintains the minimally invasive nature of the test and limits cost. A major additional advantage is excellent visualization of the articular cartilage in a highly specific and sensitive manner.
 FIGURE 37.4. The clunk test for posterior olecranon impingement is simply performed by stabilizing the upper arm and bringing the elbow into extension to produce posterior elbow pain. |
 FIGURE 37.5. Coronal fat-suppression MRI demonstrating a “T-sign,” which is indicative of a complete tear of the MCL complex at its humeral origin. |
TREATMENT
Nonoperative Treatment
Initially, a nonoperative treatment regimen is initiated consisting of a period of rest and anti-inflammatory medication to reduce pain and inflammation. Throwing athletes with partial MCL tears or those with overlapping symptoms secondary to medial epicondylitis or ulnar nerve symptoms are treated with activity modification and a shoulder-and-elbow-strengthening program. It is important that cortisone injections be avoided to prevent further tendon or ligament injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree