Elbow Arthroplasty: History, Design Evolution, and Current Design Options for Treatment
Peter S. Johnston
Matthew L. Ramsey
HISTORICAL PERSPECTIVE
Normal elbow function requires a pain-free, mobile, and stable articulation.
Nonarthroplasty surgeries
Resection arthroplasty, interposition arthroplasty, and arthrodesis predominated prior to the advent of elbow arthroplasty.
ELBOW ARTHROPLASTY (HISTORY)
Development of total elbow arthroplasty (TEA) was borne out of the failures of nonreplacement surgeries to effectively treat articular and periarticular pathologies.
The elbow was felt to function as a rigid hinge.
Early efforts at elbow arthroplasty
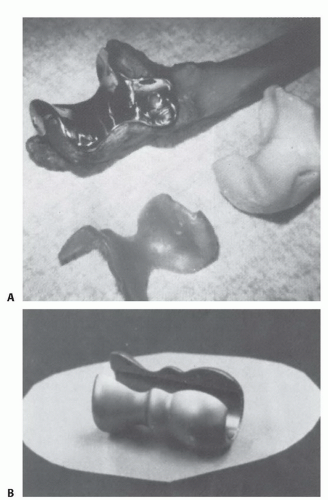
Characterized by metallic, nylon, rubber, or acrylic hemiarthroplasties of the distal humerus or proximal ulna (FIG 1).
TEAs were metallic rigid hinged devices.
Predated the introduction of polymethylmethacrylate (PMMA)
Fixation of these implants to bone was achieved through uncemented intramedullary stems or extramedullary supports screwed into cortical bone (FIG 2).
Instability, early loosening, and unpredictable range of motion limited the success of these implants.
Poor implant fixation to bone and inferior implant design contributed to high failure rates from early loosening.
EVOLUTION OF ARTHROPLASTY (EARLY EFFORTS)
The modern era of total elbow replacement was initiated with the introduction of PMMA for implant fixation.9
The period of time following this achievement was characterized by a rapid evolution in the understanding of elbow biomechanics and surgical techniques and improvements in implant materials and design.
The failure of early efforts at arthroplasty led to two approaches to implant design.
Unlinked “resurfacing” designs
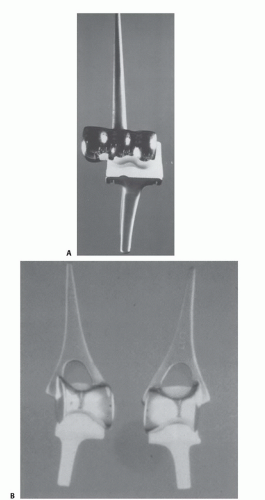
The joint is resurfaced with preservation of the collateral ligaments (FIG 3).
Success depends on the integrity of the soft tissue envelope, the presence of adequate bone stock to support the prosthesis, and the geometry of the articulation.
The contribution of the soft tissues to absorbing the forces across the elbow is believed to result in lower rates of implant loosening.
Linked “semiconstrained” designs
Stability is achieved through a coupled articulation between the humeral and ulnar components which allows a few degrees of varus-valgus and rotational laxity (FIG 4).
The ulnohumeral articulation tracks within the tolerance of the implant implying that the muscular envelope counters some of the forces across the elbow.29
EVOLUTION OF ARTHROPLASTY (MODERN EFFORTS)
TEA is in a period of refinement.
Clinical experience has demonstrated the design features that are acknowledged to contribute to success.
Anterior flange
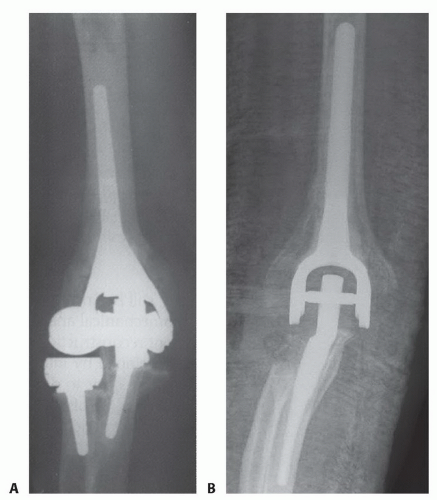
Incorporated into many linked humeral designs
Felt to counteract posterior and rotational forces across the elbow contributing to implant loosening
Incorporation and hypertrophy of the bone graft behind the anterior flange proves that the graft becomes load bearing through stress transfer (FIG 5).
Stemmed implants
The addition of intramedullary stems to the humeral and ulnar components reduced the rates of component loosening.
Cemented stems
Cement fixation of the implants is the current standard of care.
Cement technique is improved with brushing and lavage of the canals, use of PMMA in a more liquid state, and cement restrictors in the humerus and ulna to occlude the canal.12
EVOLVING ISSUES IN TOTAL ELBOW ARTHROPLASTY
Challenges remain with TEA that continue to fuel efforts to improve the outcome of surgery.
There have been numerous improvements in surgical techniques and implant design. These lessons can be broadly classified as implant fixation, instability, polyethylene wear and osteolysis (the articulation), and triceps dysfunction.
Implant fixation
The vast majority of implants are fixed to bone with PMMA.
Modern cement techniques have improved.12
Aseptic loosening has highlighted the need to continually explore alternative techniques of implant fixation.
Instability