Abstract
Introduction
The flexible derotator is one of the therapeutic resources used to combat primary and secondary abnormalities in walking cerebral palsy children. It was developed to reduce abnormal femoral and tibial torsions and lessen the latter’s negative functional impact.
Objective
To determine the effect of wearing a flexible derotator on anatomic and functional parameters in walking cerebral palsy children.
Methods
We performed a retrospective study of walking cerebral palsy children by gathering data on bone-related parameters (femoral and tibial torsion) and functional parameters (distance and speed gait, and the energy expenditure index (EEI)). Fifteen walking cerebral palsy children were treated with the flexible derotator for one year and 15 untreated walking cerebral palsy children were included as controls. The two groups were compared in terms of the various parameters’ change over time between the initial examination (the last examination prior to the start of the study or prior to use of the flexible derotator) and the final examination (after one year of follow-up).
Results
Right femoral anteversion and right and left external tibial torsion improved. There was a significant increase in distance and speed gait and a decrease in the EEI in walking cerebral palsy children.
Conclusion
Our retrospective study revealed a significant improvement in functional parameters in children with cerebral palsy, as a result of wearing the flexible derotator for at least 6 hours a day for a year. Bone parameters only improved slightly. Use of the flexible derotator could improve these children’s quality of life.
Résumé
Introduction
Parmi les moyens thérapeutiques disponibles pour lutter contre les anomalies primaires et secondaires chez les enfants paralysés cérébraux marchants (EPCM), le dérotateur souple a été développé pour réduire les phénomènes de torsions osseuses fémorales et tibiales anormales ainsi que leurs conséquences fonctionnelles.
Objectif
Déterminer l’efficacité sur le plan osseux et fonctionnel du dérotateur souple chez l’EPCM.
Méthodes
Un recueil rétrospectif de données concernant des EPCM a été réalisé sur les paramètres osseux (torsion fémorale et tibiale) et fonctionnels (périmètre et vitesse de marche sur 5 minutes, Indice de Dépense Energétique (IDE)). Quinze EPCM traités avec le dérotateur souple durant un an, et 15 EPCM non traités ont été inclus dans cette étude. Les paramètres du bilan initial (bilan le plus récent réalisé avant le début de l’étude, ou à la mise en place du dérotateur souple) et du bilan final (bilan réalisé un an après le début du suivi) ont été analysés comparativement dans les deux groupes.
Résultats
Il existait une amélioration de l’antéversion fémorale droite, de la torsion tibiale externe droite et gauche, une augmentation significative du périmètre et de la vitesse de marche, et une diminution de l’IDE chez les EPCM.
Conclusion
Cette étude rétrospective rapportait une amélioration significative des paramètres fonctionnels chez les enfants paralysés cérébraux ayant porté le dérotateur souple quotidiennement six heures par jour pendant un an, mais une faible amélioration des paramètres osseux. Cela pourrait ainsi améliorer la qualité de vie de l’enfant.
1
English version
1.1
Introduction
Children with cerebral palsy present many impairments due to brain damage suffered during pregnancy and/or the perinatal period . The initial neurological lesions do not worsen over time. However, the resulting neuromuscular imbalances (motor handicaps, muscle imbalance and spasticity) and motor control disorders (referred to as primary abnormalities) prompt the appearance of new impairments which do worsen over time (notably during growth). These new impairments are referred to as secondary abnormalities (musculoskeletal deformations) and tertiary abnormalities (very adverse gait disorders and compensations) . The therapeutic goal (particularly in ambulatory children with cerebral palsy) is to combat primary abnormalities and attempt to prevent and treat secondary and tertiary abnormalities .
The musculoskeletal deformations notably include excessive femoral anteversion and internal hip rotation. This femoral rotation disorder is triggered by spasticity and musculotendinous retraction of the hip rotators . Several treatment approaches are currently available for reducing or correcting the excess rotation, depending on the predominating abnormality : injection of botulinum toxin into the spastic muscles , tenotomy of the retracted muscles and derotation osteotomy . Indeed, these individual approaches can be combined into a complex programme of multisite surgery once the child has stopped growing . A physiotherapeutic treatment approach has been extensively developed by Le Métayer , which particularly insists on the muscle relaxation obtained by the use of inhibition techniques, posture in a relaxed position and work on restoring innate neuromotor behaviour.
An orthosis (the flexible femur derotator ) was recently designed by J. Reydelet with the intention of reducing axial femoral and tibial bone torsion and limiting the latter’s negative functional impact . The device is intended to replace the use of rigid derotators, which are no longer used in view of the constraints on the child, limiting joint amplitudes and leading to abnormal poorly functional gait . The flexible derotator was designed to reduce the occurrence of rotational disorders and bone torsion during growth and thus improve the quality of the child’s gait in general and decrease energy expenditure during effort in particular. This improvement is obtained by modifying the biomechanics of gait: the orthosis is designed to facilitate hip extension and knee joint locking, decrease the likelihood of scissor gait and limit excessive internal or external hip rotation . This new orthosis is better tolerated than older models by virtue of its fully elastic, flexible textile-like structure.
To our knowledge, the use of the flexible derotator and its impact on femoral torsion have not yet been studied. The present study therefore sought to determine whether the flexible derotator reduces rotational disorders of the femur and tibia in walking cerebral palsy children and whether it has a functional impact on gait parameters and energy expenditure.
1.2
Material and methods
This retrospective study was performed by examining the medical records of patients treated in the paediatric unit of a specialist physical and rehabilitation medicine (PRM) clinic.
1.2.1
Material: description of the flexible hip derotator
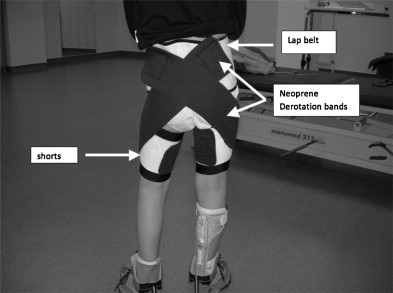
The flexible derotator is a custom-designed item of clothing constituted by an abdominal belt and two neoprene thigh bands (or shorts) ( Fig. 1 ). Neoprene is an elastic, compressive material which adheres to the skin and thus stops the orthosis from slipping during gait. The orthosis is custom-made, in order to avoid pressure points. Two straps are attached to the abdominal belt and the two thigh bands. The straps can be made of (i) neoprene if significant rotational correction is required or (ii) a more flexible and less restrictive elastic fabric if a lesser degree of correction is sufficient. The straps are placed in a spiral position, in order to prevent poor posture. If medial femur rotation is present, the orthosis is expected to induce a movement which counters poor posture, i.e. external hip rotation so that the leg segment remains in the sagittal plane. If lateral femoral torsion is present, the force exerted by the orthosis should induce internal hip rotation. These lines of force are shown in Fig. 2 .

 (white cross on the Figure) point of attachment with Velcro.
(white cross on the Figure) point of attachment with Velcro.  Force vector.
Force vector.  Position of the grand trochanter.
Position of the grand trochanter. The orthosis must be fitted symmetrically in all cases – even for a unilateral disorder. In fact, if the flexible derotator is used on one leg only, the torsion component induced by the orthosis would be compensated for by homolateral rotation of the pelvis. Moreover, it is very important to consider morphostatic aspects in all three spatial planes because the straps’ force vectors can induce poor posture.
If required, the flexible derotator can be adjusted from the femur to a tibial segment. To this end, a Velcro patch is placed on a lower leg brace (notably “lift” braces). This enables a strap to be attached between the brace (usually on the posterior aspect) and the thigh band. The orthosis is then fitted as described above, depending on whether the rotation is medial or lateral.
The participants wore the derotator for at least 6 hours a day .
1.2.2
Population
The patients included in this study were walking children (aged from 6 to 9) with cerebral palsy and clinically significant rotational disorders. The children had been monitored for at least one year in a paediatric PRM unit.
The study population comprised two groups:
- •
a flexible derotator group (the “FD group”) of 15 walking children (9 boys and 6 girls) with cerebral palsy and who wore the flexible derotator for 6 hours a day throughout the study. There were 11 spastic diplegic children, one right-side hemiplegic child and three tetraparetic children. The mean (± SD) age was 8 ± 1.4 (range: 6-9). One other child was immediately excluded from the FD group because skin irritation prompted the abandonment of the derotator on the first day of use;
- •
a control group of 15 walking children (8 boys and 7 girls) with cerebral palsy and who did not wear a flexible derotator: 11 spastic diplegic children, two right-side hemiplegic children, one tetraparetic child and one triplegic child. The mean (± SD) age was 8 ± 1 (range: 6–9).
The two groups were constituted retrospectively. The indication for use of the flexible derotator was the presence of rotational disorders with a functional impact on gait quality and efficiency in a prepubertal child in whom spasticity was graded below 4 on the modified Ashworth scale.
There were no significant differences between the two groups in terms of mean age, gender distribution, systematic clinical follow-up (between 1 and 3 visits a year), mean Gross Motor Function Measure score, mean Gillette score and spasticity on the modified Ashworth scale.
1.2.3
Evaluation tools
The various bone-related and functional parameters studied here are specified in Table 1 . These data were collected retrospectively from the patients’ medical records and physiotherapy reports. Bone parameters were measured according to Viehweger et al.’s guidelines . Gait distance and speed were measured during a 5-minute gait test during which the child had to walk up and down a 20-metre test track as many times as possible. The gait distance was thus recorded and the average gait speed was calculated. The child’s heart rate was measured immediately after the end of the 5-minute test so that the energy expenditure index (EEI) could be calculated according to following equation: EEI = heart rate/average speed.
| Descriptions and measurements | Reference values | |
|---|---|---|
| Bone parameter | ||
| Femoral anteversion | Measured in the prone position, with the knee flexed at 90°. One palpates the greater trochanter and then applies internal hip rotation while holding the malleoli. When the greater trochanter moves under the fingers, the movement is stopped and one measures the angle between the axis of the limb segment and the vertical axe | The usual mean femoral anteversion for children of this age (6 to 9) ranges from 20° to 25° |
| Thigh/foot angle | The child lies in the prone position, with the hip extended and the knee flexed at 30°. One measures the angle between the axis of the foot and that of the thigh | |
| External tibial torsion | The child sits on the edge of a table, with his/her legs hanging down. The internal tibial torsion corresponds to the angle between the bimalleolar axis and the horizontal axis | This parameter normally varies from 0° to 20° during growth |
| Internal tibial torsion | The measurement is performed in the same way as for external tibial torsion | |
| Functional parameters | ||
| Number of metres covered during the 5-min gait test | Enables definition of the number of metres that the child can cover during five minutes | |
| Energy expenditure index | This is the ratio between the heart rate and the average speed. It enables evaluation of a potential improvement in energy efficiency during gait with the orthosis | 2.09 (< 0.32) between 6 and 7 years of age, 2.01 (< 0.27) between 7 and 8 years of age, 1.91 (± 0.26) between 8 and 9 years of age |
Tolerance issues related to use of the orthosis during the treatment period (irritation, skin damage, overheating, psychological problems, etc.) were identified in the participants’ medical records.
1.2.4
Statistical analyses
For each patient, we took account of the parameters recorded during the initial examination (corresponding to the last examination prior to the start of the study for the control group or prior to initiation of flexible derotator use for the FD group) and the final examination (performed at the end of the study, i.e. after one year of orthosis use in the FD group and after one year of follow-up in the control group).
Mean values and standard deviations were calculated for all measured and calculated variables. A test of normality was performed for each parameter, with calculation of a skewness coefficient for the distribution’s asymmetry and a kurtosis coefficient for its flatness. For each parameter, the effects of the “treatment” (use of a flexible derotator orthosis vs. no orthosis) and “time” factors (initial examination vs. final examination) were examined in a two-way repeated measures analysis of variance (ANOVA) and then (if the result reached the significance threshold) a Student’s t-test. All analyses were performed with Statview® software (Version 5.0, SAS Institute Inc., Cary, NC, USA). The significance threshold was set to P < 0.05.
1.3
Results
The mean values of the study’s descriptive parameters are reported in Table 2 . The interaction between the “treatment” and “time” factors was significant for right femoral anteversion, the left-side thigh/foot angle, left external tibial torsion and the gait distance and speed. The “treatment” effect was not significant for any of the parameters. The “time” effect was significant for left external tibial torsion and the gait distance and speed.
| Initial examination | Final examination | |
|---|---|---|
| Bone parameters (in degrees) | ||
| Left femoral anteversion | ||
| FD group | 36.3 ± 11.1 | 33.3 ± 7.5 |
| Control group | 36.0 ± 11.7 | 36.7 ± 12.1 |
| Right femoral anteversion | ||
| FD group | 42.7 ± 7.3 a,b | 37.7 ± 8.2 a |
| Control group | 35.3 ± 9.5 b | 35.7 ± 9.0 |
| Left-side thigh/foot angle | ||
| FD group | 2.7 ± 8.2 | 3.7 ± 6.9 |
| Control group | 7.3 ± 8.2 | 1.3 ± 11.1 |
| Right-side thigh/foot angle | ||
| FD group | 6.7 ± 5.6 | 6.3 ± 5.5 |
| Control group | 6.3 ± 8.1 | 4.3 ± 6.8 |
| Left external tibial torsion | ||
| FD group | 18.2 ± 9.9 a | 14.7 ± 9.5 a |
| Control group | 11.3 ± 9.9 | 13.1 ± 9.7 |
| Right external tibial torsion | ||
| FD group | 23.3 ± 8.8 a,b | 17.7 ± 9.8 a |
| Control group | 16.3 ± 9.7 b | 14.6 ± 8.7 |
| Functional parameters | ||
| Gait distance (m) | ||
| FD group | 238.1 ± 55.0 a | 265.5 ± 58.6 a |
| Control group | 247.2 ± 97.4 | 242.6 ± 106.3 |
| Mean gait speed (m/min) | ||
| FD group | 47.6 ± 11.0 a | 53.1 ± 11.7 a |
| Control group | 49.7 ± 19.2 | 50.1 ± 21.7 |
| EEI (beats/m) | ||
| FD group | 2.8 ± 1.0 a | 2.7 ± 0.8 a |
| Control group | 3.5 ± 2.7 | 4.8 ± 7.4 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







