Abstract
Objective
The aim of this study was to analyze the effect of running retraining on the recovery of the knee’s functional and muscular properties after anterior cruciate ligament (ACL) reconstruction.
Methods
Eighty-five athletes who had undergone ACL reconstruction surgery were selected randomly to receive, or not to receive, controlled running training based on interval training and speed exercises. The effect of retraining was measured by the evolution of the knee’s isokinetic strength deficit and progress (at angular speeds of 60 and 180°/s), the knee laxity parameters and the score on the Lysholm Knee Scale from the 4th to the 6th month after the surgery. Forty subjects were retrained and compared with 40 control-group subjects. The effect of the retraining program was studied in terms of the type of ACL reconstruction and the effect of time.
Results
After retraining, no difference was found for isokinetic knee strength deficit and progress, knee laxity and Lysholm Knee Score. The isokinetic strength deficit was influenced mainly by the type of ACL reconstruction.
Conclusion
It would seem that running retraining has an insufficient effect on the muscular and functional recovery after ACL reconstruction, despite the fact that this type of training is well-tolerated.
Résumé
Objectif
L’étude avait pour objectif d’analyser après ligamentoplastie de genou, l’impact d’un réentraînement à l’effort par la course à pied sur la récupération fonctionnelle et musculaire du genou.
Méthode
Quatre-vingt-cinq sportifs ayant bénéficié d’une reconstruction du ligament croisé antérieur ont été tirés au sort pour pratiquer ou non un réentraînement à l’effort basé sur la pratique de la course à pied à vitesse variée. L’effet du réentraînement a été mesuré à partir de l’évolution entre les quatrième et sixième mois postopératoires du déficit et des progrès de force isocinétique du genou (60 et 180°/s), des paramètres de laxité du genou et du score de Lysholm. Quarante patients ont été réentraînés et comparés à 40 patients témoins. L’effet du programme de réentraînement a été étudié en tenant compte du type de reconstruction du ligament croisé antérieur et de l’effet temps.
Résultats
Après le réentraînement, aucune différence n’a été retrouvée au niveau des valeurs isocinétiques pour les déficits et progrès, ainsi qu’au niveau de la laxité du genou et le score de Lysholm. Le déficit de force isocinétique a été particulièrement influencé par le type de reconstruction du ligament croisé antérieur.
Conclusion
Il semblerait que la course à pied ait peu d’effet sur la récupération musculaire et fonctionnelle après reconstruction du ligament croisé antérieur alors que celle-ci est bien tolérée.
1
English version
1.1
Introduction
Each year, many people undergo anterior cruciate ligament (ACL) reconstruction surgery. Ligament reconstruction using a patellar tendon graft or a hamstring graft is frequently recommended in order to improve the knee’s stability and make the knee less painful, as well as to allow people to resume their previous athletic activities, if at all possible . It is necessary to gradually resume athletic training because detraining occurs when athletic activity ceases . For example, given that there is no traumatism, 4 weeks of inactivity will lead to a 10% loss of strength and a 25% loss of aerobic capacity .
After ACL reconstruction, an isokinetic strength deficit in the operated knee is expected compared to the contralateral knee. However, this isokinetic deficit is dependent on the type of surgery. Four months after a ligament reconstruction using a patellar tendon graft, the deficit of the knee extensors and flexors evaluated at an angular speed of 60°/s can reach, respectively, 36 to 47% and 7 to 13% . For the same time period after surgery and the same angular speed, the isokinetic deficit of the knee extensors and flexors for a ligament reconstruction using a hamstring graft is, respectively, from 25 to 35% and 8 to 34% . Various retraining programs have been proposed to reduce this strength deficit, without however really knowing if this deficit can be reduced.
Retraining via certain aerobic activities, such as cycling or stair exercises, have already been studied, but none of these activities has proved effective for recuperating isokinetic knee strength . Previously, we studied the effect of continuous intensity running retraining and were not able to demonstrate a significant effect compared to a non-retrained group . Nonetheless, concentric isokinetic tests at angular speeds of 60 and 180°/s are known to be objective for monitoring the knee’s evolution after surgery . This observation led us to analyze the impact of running retraining on the muscular strength of the knee’s extensors and flexors at 4 and 6 months after surgery. We based our analysis on isokinetic evaluations of running at varied angular speeds. During the same period, we used the Lysholm Score to study the subject’s tolerance of this retraining program in terms of instrumental laxity and the occurrence of subjective pain.
1.2
Materials and methods
1.2.1
Population
Between January 2005 and January 2006, isokinetic tests were proposed to 117 athletes. Table 1 provides the anthropometric data for these athletes. The subjects in this population, which originally had the same number of patellar tendon grafts and hamstring (i.e., semi-tendinosus and gracilis [STG]) grafts, were included prospectively according to the following criteria: aged between 18 and 50, lack of knee surgery antecedents, first ACL reconstruction, healthy contralateral knee, and practice of a pivot-contact sport three times a week before the ACL rupture. The exclusion criteria included: bilateral knee reconstruction, anterior or posterior knee pain, a Complex Regional Pain Syndrome (CRPS), a meniscal complication during the follow-up period, cardiovascular intolerance and/or knee disease. All subjects were informed about the study protocol and gave their consent without financial incentives. The study was approved by the Ethics Committee of the Regional Institute of Sports Medicine.
| PT retrained ( n = 21) | STG retrained ( n = 19) | PT control ( n = 20) | STG control ( n = 20) | p | |
|---|---|---|---|---|---|
| Age (years) | 22.7 ± 1.3 | 23.8 ± 1.2 | 25.2 ± 1.7 | 23.5 ± 2 | 0.64 |
| Weight (kg) | 73 ± 2.6 | 75 ± 2.9 | 72 ± 2.9 | 74 ± 3.7 | 0.72 |
| Height (cm) | 177 ± 1 | 176 ± 2 | 177 ± 1 | 175 ± 2 | 0.56 |
| Duration (month) | 5.9 ± 3 | 6.3 ± 4 | 5.7 ± 3 | 5.2 ± 4 | 0.54 |
| Tegner Score | 7.1 [6–9] | 7.9 [6–10] | 6.9 [6–9] | 7.3 [6–9] | 0.61 |
| Meniscus | Medial 3 | Medial 3 | Medial 4 | Medial 4 | |
| Lateral 1 | Lateral 3 | Lateral 2 | Lateral 3 | ||
| Medial + lateral 2 | Medial + lateral 1 |
After inclusion, the subjects were randomly chosen to participate, or not participate, in a running retraining program. They executed up to 30 minutes of running at various speeds three times a week for 2 months according to the program provided in Table 2 . Four groups were formed based on the type of ligament reconstruction and inclusion or non-inclusion in a retraining group (PT retrained , PT control , STG retrained and STG control ) ( Fig. 1 ). The subjects that did not complete the entire program were excluded from the study population. No postoperatory differences were observed between the four groups in terms of age, weight, height, the time between the ACL rupture and its reconstruction, and the Tegner Athletic Activity Score before the rupture occurred ( Table 1 and Appendix A ). During the surgery, the four groups showed no differences in terms of association to a meniscal pathology. Of the total 117 ACL reconstruction subjects, 85 male subjects were accepted into the study.
| Weeks | Duration (min) | Intensity |
|---|---|---|
| 1 | 5 × 3 | Walking and running at 70% CF max |
| 5 × 3 | Walking and running at 70% CF max | |
| 5 × 3 | Walking and running at 70% CF max | |
| 2 | 15 | Running at 70% CF max |
| 15 | Running at 70% CF max | |
| 15 | Running at 70% CF max | |
| 3 | 20 | Running at 70% CF max with 1 min × 5 IT (85% CF max ; 1 min rest period) |
| 20 | Running at 70% CF max | |
| 20 | Running at 70% CF max with 2 min × 3 IT (85% CF max ; 1 min rest period) | |
| 4 | 15 | Running at 70% CF max |
| 15 | Running at 70% CF max with 100 m × 5 accelerations (maximum speed) | |
| 15 | Running at 70% CF max | |
| 5 | 20 | Running at 70% CF max with 1 min × 5 IT (85% CF max ; 1 min rest period) |
| 20 | Running at 70% CF max with 80 m × 5 accelerations (maximum speed) | |
| 20 | Running at 70% CF max with 2 min × 3 IT (85% CF max ; 1 min rest period) | |
| 6 | 25 | Running at 70% CF max with 1 min × 5 × 2 IT (85% CF max ; 1 min rest period) |
| 25 | Running at 70% CF max with 100 m × 8 accelerations (maximum speed) | |
| 25 | Running at 70% CF max with 2 min × 5 IT (85% CF max ; 1 min rest period) | |
| 7 | 30 | Running at 70% CF max with 1 min × 10 IT (85% CF max ; 1 min rest period) |
| 30 | Running at 70% CF max with 80 m × 5 × 2 accelerations (maximum speed) | |
| 30 | Running at 70% CF max with 2 min × 5 IT (85% CF max ; 1 min rest period) | |
| 8 | 20 | Running at 70% CF max |
| 20 | Running at 70% CF max with 80 m × 10 accelerations (maximum speed) | |
| 20 | Running at 70% CF max | |

1.2.2
Surgical procedures
All surgical procedures were performed by arthroscopy by two experienced surgeons in order to evaluate the residual ACL and the menisci, which were treated if necessary. The central third of the patellar tendon or the four-strand hamstring technique using the STG muscles of the operated knee were used to reconstruct the ACL. An interference screw (BIO RCI, Smith Nephew endoscopy) was used to fix the graft in proximal and distal directions in both types of reconstructions. For the patellar tendon graft, the size of the tunnel was set 1 mm larger than the size of the bone block (from 7 mm to 11 mm), and for the hamstring technique, the size of tunnel was the same as the diameter of the STG graft (from 7 to 10 mm). In addition, for the hamstring technique, the distal fixation was reinforced by a staple (Smith Nephew Richards Memphis, USA).
1.2.3
Accelerated rehabilitation program
All the subjects benefited from a rehabilitation protocol that was similar either to the Shelbourne and Nitz’s accelerated rehabilitation protocol for the patellar tendon graft or to the Mac Donald et al.’s accelerated rehabilitation protocol for the hamstring graft . The goal was to restore as rapidly as possible the complete range of motion, quadriceps function and load-bearing capacity. A splint was used at first if quadriceps activity was not sufficient to control the knee during the unilateral stance-phase of the gait cycle. Cane support when walking was stopped when the load-bearing leg could be controlled for 10 seconds. The progression was guided based on the presence of pain and/or swelling, measured each week using the knee’s perimetric measurements for swelling and a Visual Analogue Scale for Pain (VAPS) .
The exercises intended to reinforce the quadriceps were closed kinetic chain exercises. No reinforcement and/or stretching of the hamstrings was done in the first 4 weeks after the hamstring graft because of the risk of posterior knee pain due to the absence of hamstring tendons . All subjects were supervised by a physical therapist during their postoperatory rehabilitation. Swimming and cycling were permitted 2 months after the surgery, but running was not allowed before the isokinetic tests had been performed 4 months after surgery.
1.2.4
Isokinetic evaluation
All the isokinetic tests were performed by the same doctor, a specialist in physical medicine and rehabilitation, who used a Cybex Norm isokinetic dynamometer (Rankoma, NY, USA). This doctor did not know whether the subject had, or had not, participated in the running retraining program. All subjects were tested at 4 and 6 months after their surgery. Each test session was preceded by a warm-up (10 minutes of pedaling on an ergocycle at 70 rpm and 50 w) and stretching exercises. Each subject was seated so that his hip would be flexed at 85°. The mechanical axis of the dynamometer was aligned with the external condyle of the knee. The trunk and the thigh were stabilized with belts. The knee’s range of motion was 100° (from 0 to 100°). The lever arm of the dynamometer was positioned at the leg’s distal level. The gravity correction was calculated at 45° of knee flexion.
The calibration of the dynamometer was controlled before each session according to the manufacturer’s recommendations. During a session, the evaluation always began with the knee extensors and flexors of the healthy limb. Three and five repetitions based on concentric contractions were used at speeds of 60 and 180°/s, chosen because of the frequency of their use . Rest periods of 1 minute were given between each series of tests. All the subjects were given visual feedback and verbal encouragement. The maximum peak torque was taken into consideration for the chosen angular speed.
1.2.5
Retraining by running
The retrained group participated in a running training program derived from the continuous running program that we evaluated in 2006 ( Table 2 ). The running exercises were scheduled three times a week (Tuesday, Thursday and Sunday) and were monitored with the aid of a written training notebook. The running intensity was chosen based on the percentage of the maximal heart frequency, estimated using the formula, 220 – subject age, in order to increase the subject’s aerobic capacities and resume the speed exercises needed to play team ball sports. The intensity of the retraining program and program compliance was controlled by computer.
1.2.6
Clinical evaluation
All subjects were evaluated at 4 and 6 months after their surgery by the same clinical practitioner, who was totally independent of the surgeons. Knee pain was assessed on a VAPS and knee function was assessed through the Lysholm Score in order to determine how well the subjects tolerated the retraining program. The knee’s clinical stability was evaluated using the Lachman test and the jerk, or pivot shift, test. These tests were graduated according to the symmetry of the two knees: exactly symmetric – 0, a slight difference – 1+, a moderate difference – 2+, and a great difference or a subluxation – 3+ . The instrumental laxity was determined by the same clinical practitioner using the arthometer KT 1000 (Medmetric Corp, San Diego, CA, USA). The displacement difference was measured using a manual force of 134 N.
1.2.7
Statistical analysis
The statistical analysis was performed using the software SPSS (SPSS 14.0, SPSS Inc, Chicago, USA). The isokinetic deficits and progress were expressed in percentages. The average and the standard deviation for instrumental laxity and the Lysholm Score were calculated for 4 and 6 months after surgery. The anthropometric parameters of all groups (PT retrained , PT control , STG retrained and STG control ) were compared through variance analysis. The effect of the running retraining program on the isokinetic strength deficit and the Lysholm Score was established in terms of the type of ACL reconstruction using a mixed linear model (time + ACL reconstruction + retraining + subjects). All factor interactions were tested, and the significance level was set at p < 0.05.
1.3
Results
1.3.1
Knee pain and knee function
In general, the retraining program was well-tolerated. Three subjects judged the 1st week of the program difficult due to their detraining and two subjects judged the program too easy. Three subjects, who had undergone patellar tendon ACL reconstruction (PT-ACLR), reported some knee pain (VAPS: 1.9, 2.1 and 2.5). Two subjects, who had undergone hamstring ACL reconstruction (STG-ACLR), suffered from pain in the hamstrings when running sprints (VAPS: 2.6 and 3.8). In the control group, two PT-ACLR subjects and one STG-ACLR subject reported anterior knee pain; two STG-ACLR subjects experienced hamstring discomfort during daily activities (VAPS < 2). No other subjects reported pain.
According to the Lysholm Score, knee function increased following the retraining program, though no difference was found between the types of ACL reconstruction ( p = 0.78). Depending on the group, the average Lysholm scores, which were between 90.5 and 92.3 points at 4 months after surgery, reached 95.8 to 97.7 points (out of a possible 100) at 6 months after surgery.
1.3.2
Knee laxity
Both the knee laxity evaluated by the Lachman test and the difference in anterior tibial displacement between the two knees measured by the arthometer KT 1000 at 134 N were identical following retraining, independent of the type of ACL reconstruction. The majority of the subjects had differences of under 2 mm (i.e., 0.6–2) at 4 and 6 months after surgery.
1.3.3
The knee’s isokinetic strength
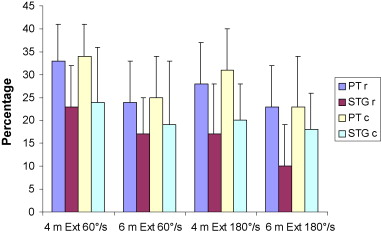
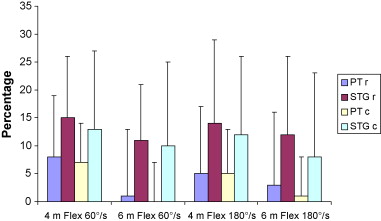
The running retraining program did not reduce the knee’s isokinetic strength deficit and did not have any impact the knee’s isokinetic progress. No interaction was found between the retraining program and the type of ACL reconstruction. Our results showed a less significant muscular deficit in the 6th month after surgery compared to the 4th month after surgery, without indicating any influence of the running retraining program or the type of ACL reconstruction ( Figs. 2 and 3 ). However, the strength deficits in the knee extensors and flexors depended significantly on the technique used during the ACL reconstruction. The deficit in the extensors was greater after PT-ACLR surgery and the deficit in the flexors was greater after STG-ACLR surgery ( Figs. 2 and 3 ).
1.4
Discussion
In order for athletes to recover their previous level in their sport following ACL reconstruction surgery, they need to resume running, especially if said athletes play a pivot-contact sport like soccer, basketball or handball. All of our subjects were particularly motivated to regain their previous levels in their sports.
Usually, retraining programs are empirical . Jogging is often recommended after the 3rd month following surgery because of the forces exerted on the knee. Running at a speed of 9 km/h exerts a force measured at eight times the runner’s body weight. This force increases with the running speed, attaining 14 times the runner’s body weight at 16 km/h . We intentionally authorized resuming running at 4 months after surgery for subjects who, despite having been operated on recently, had a flexible and painless knee without swelling. Knee pain can be the cause of a muscular strength deficit in the knee extensors in cases of anterior pain (PT), in the knee flexors in cases of posterior pain (STG), or both muscles groups in cases of complex regional pain syndrome . From an ethical perspective, it would have thus been inconceivable to propose a running retraining program to subjects who were in pain.
At 4 months after surgery, a deficit in the extensors and flexors of, respectively, 36 and 9% is to be expected for surgery using a patellar tendon graft . For surgery using a hamstring graft, the expected deficit in the knee extensors is between 25 and 35% while the expected deficit in the knee flexors is between 8 and 34% . Compared to these results, the results for our population at the moment of inclusion were slighter better, probably because we excluded the subjects who were in pain. However, as the standard deviations in Fig. 2 show, the intersubject variation remains relatively large, which reinforces the relevance of isokinetic evaluations after surgery in order to optimize the rehabilitation protocol.
At 6 months after surgery, our running retraining program, which included interval training and speed exercises, was not able to significantly improve the knee’s isokinetic strength deficit and progress. Using the customary concentric isokinetic evaluations at angular speeds of 60 and 180°/s was perhaps not the right test procedure, given the significant differences in the speed-strength relationship, the angular displacements, and muscle contraction mode of the knee’s extensors and flexors during running activities. A fatigability test based on 30 repetitions at angular speeds of 180 and 240°/s would have perhaps produced different results.
Given that the speed-strength relationship is characterized by the predominance of eccentric hamstring contractions during running, Aagaard et al. have suggested using an eccentric “functional” ratio for knee flexors and a concentric “functional” ratio for knee extensors for evaluating retraining programs . Croisier et al. have shown the advantages of eccentric knee flexor evaluations for identifying the strength deficit compared to the non-operated knee and determining the level of flexor/extensor imbalance in the operated knee . Still, Impellizzeri et al. have shown the low reliability of the agonist/antagonist strength ratios (detection of a change at 17%), and their results suggest that the knee’s eccentric/concentric ratio at 60°/s is especially useful for detecting important changes, like those observed after retraining programs . A more rapid isokinetic angular speed (240 or 450°/s) could have perhaps been used to measure the knee’s joint movement since these speeds are more like the ones observed during running .
The frequency and the intensity of the retraining program were perhaps insufficient to stimulate enough anaerobic capacity to obtain a significant improvement in muscular strength. We chose the frequency of three times a week because it corresponded to the number of times per week that our athletes played their sport. As for the intensity, we chose to have the athletes perform at 70% of their maximal heart frequency during the first 4 weeks of our retraining program in order to stimulate their aerobic capacity without damaging the recently operated knee. However, it would have perhaps been desirable to propose specific muscular reinforcement exercises, such as those done on the leg press or the hamstring machine, in order to obtain a significant improvement in isokinetic strength of the knee’s extensors and flexors.
Mikkelsen et al. have shown that, after exercise in closed kinetic chains or a blend of open and closed chains, strength improved only in the knee extensors, but not in the knee flexors . On the other hand, Heijne and Werner reported no influence of open kinetic chain exercises on quadriceps strength in subjects undergoing hamstring ACL reconstruction . Specific hamstring reinforcement exercises seem to be needed, particularly after hamstring ACL reconstruction, given that this muscle group remains weak for the first 6 weeks after surgery .
Nonetheless, our retraining protocol involving interval training and speed exercises was well-tolerated by our subjects, as indicated by the Lysholm Scores, which increased from the 4th month after surgery to the 6th month after surgery; the clinical and instrumental laxity scores, which did not increase compared to the control group; and in particular, the fact that no subjects abandoned the program because they could not tolerate it. Only five subjects reported anterior or posterior pain in the 1st week of the retraining program.
1.5
Conclusion
Despite our study’s limitations (i.e., the absence of an eccentric isokinetic knee evaluation paired with an evaluation of the subject’s aerobic potential), although the retraining program was well-tolerated by our subjects, running did not appear to influence the knee’s muscular and functional recovery. In the absence of painful complications, strength recovery depends more on the surgical technique used. Thus, to improve the strength of the knee, a program of muscular reinforcement appears to be necessary.
Conflict of interest statement
The authors have not declared any conflict of interest.
Appendix A. Lysholm Score
| Instability | Pain | Blockage | Swelling | ||||
|---|---|---|---|---|---|---|---|
| Never gives way | 25 | Never | 25 | Never | 15 | Never | 10 |
| When exercising, rarely | 20 | When exercising, moderate | 20 | Catching without blocking | 10 | During intense exercise | 6 |
| When exercising, frequently | 15 | When exercising, great | 15 | Occasional blocking | 6 | During daily activities | 2 |
| Occasional, daily life | 10 | Walking > 2 km | 10 | Frequent blocking | 2 | Constant | 0 |
| Often, daily life | 5 | Walking < 2 km | 5 | Severe blocking when examined | 0 | ||
| With every step | 0 | Constant | 0 | ||||
| Stairs | Squatting | Limping | Use of cane | ||||
|---|---|---|---|---|---|---|---|
| No problems | 10 | No problems | 5 | No limp | 5 | Never | 5 |
| Slight handicap | 6 | Slight handicap | 4 | Occasional limp | 3 | Constant use | 2 |
| One step at a time | 2 | Not more than 90° | 2 | Severe and constant limp | 0 | Standing upright impossible | 0 |
| Impossible | 0 | Impossible | 0 | ||||
Lysholm – Tegner activity level:
10 – Competitive sports: national or international level – soccer.
9 – Competitive sports: lower level – soccer, ice hockey, gymnastics.
8 – Competitive sports: squash, badminton, athletics (jumping), downhill skiing.
7 – Competitive sports: tennis, athletics (running), motocross, speedway, handball, basketball.
Leisure sports: soccer, ice hockey, squash, cross-country.
6 – Leisure sports: tennis, badminton, handball, basketball, downhill skiing, jogging (5×/week).
5 – Competitive sports: cycling.
Leisure sports: jogging (2×/week) on uneven terrain, construction work (heavy).
4 – Leisure sports: cycling, jogging (2×/week) on flat terrain, domestic work (average).
3 – Competitive or leisure sports: swimming, forest hiking, general work (slight).
2 – General work (slight), forest hiking impossible.
1 – Sedentary work, walking on flat terrain possible.
0 – Professional handicap.
2
Version française
2.1
Introduction
De nombreux sujets bénéficient chaque année d’une reconstruction du ligament croisé antérieur (LCA). Les ligamentoplasties au tendon rotulien et aux ischiojambiers sont fréquemment recommandées afin de redonner un genou stable et indolore et si possible, afin de permettre la reprise des activités sportives antérieures . Le réentraînement sportif progressif est alors nécessaire en raison du désentraînement qui est apparu depuis l’arrêt sportif . En l’absence de traumatisme, quatre semaines d’inactivité entraînent une perte de 10 % de la force et de 25 % des capacités aérobies . Après reconstruction du LCA, un déficit de force isocinétique est attendu par rapport au genou controlatéral. Ce déficit isocinétique dépend du type de chirurgie. À quatre mois d’une ligamentoplastie au tendon rotulien, le déficit des extenseurs et des fléchisseurs du genou évalué à la vitesse angulaire de 60°/s peut atteindre 36 à 47 % et 7 à 13 %, respectivement . Au même délai et pour la même vitesse angulaire, le déficit isocinétique des extenseurs et fléchisseurs du genou après ligamentoplastie aux ischiojambiers est évalué entre 25 et 35 % et 8 à 34 %, respectivement . Ainsi, différents programmes de réentraînement sont proposés pour diminuer le déficit la force mais, sans réellement savoir si ce déficit peut s’améliorer. Le réentraînement par certaines activités aérobies comme la pratique de la bicyclette ou d’exercices dans les escaliers a déjà été étudié mais aucune efficacité sur la récupération de la force isocinétique des extenseurs et fléchisseurs du genou n’a été rapportée . Nous avons également étudié l’effet de la course à pied selon une intensité continue sans pouvoir démontrer un effet significatif par rapport à un groupe non réentraîné . Pourtant, les tests isocinétiques concentriques aux vitesses angulaires de 60 et 180°/s sont connus pour être objectifs afin de suivre l’évolution après chirurgie du genou . À partir de ce constat, le but de cette étude a été d’analyser, à partir d’évaluations isocinétiques, l’impact d’un réentraînement par la course à pied, mais cette fois-ci avec des vitesses variées sur la force musculaire des fléchisseurs et extenseurs du genou à quatre et six mois postopératoires. Durant la même période, la tolérance de ce programme de réentraînement a été étudiée selon le score de Lysholm, en termes de laxité instrumentale et de la survenue de douleur subjective.
2.2
Matériel et méthode
2.2.1
Population
Entre janvier 2005 et 2006, 117 sportifs ont été adressés par deux chirurgiens afin de bénéficier de tests isocinétiques. Sont présentées dans le Tableau 1 les données anthropométriques des sujets. À partir de ce recrutement, qui a été à l’origine d’autant de greffons au tendon rotulien qu’aux ischiojambiers, les sujets ont été inclus prospectivement selon les critères suivants : âge compris entre 18 et 50 ans, absence d’antécédent de chirurgie de genou, première reconstruction du LCA, genou controlatéral sain, pratique d’un sport pivot contact trois fois par semaine avant la rupture du LCA. Les critères d’exclusion ont été représentés par une reconstruction bilatérale des genoux, la présence de douleurs antérieures ou postérieures du genou, d’un syndrome douloureux régional complexe à quatre mois postopératoires et d’une complication méniscale durant le suivi. Aucune intolérance cardiovasculaire et maladie du genou ne devait être présente. Tous les sujets ont été informés du protocole et ont donné leur consentement sans percevoir d’avantage financier. L’étude a été approuvée par le comité d’étique de l’institut régional de médecine du sport.








