Abstract
Objectives
To evaluate, in chronic heart failure (CHF) patients, feasibility, safety, compliance and functional improvements of an eccentric (ECC) cycle training protocol personalized by the rate of perceived exertion (RPE; 9–11 Borg Scale), compared to concentric (CON) training at workload corresponding to the first ventilatory threshold.
Methods
Thirty patients were randomly allocated to ECC or CON training (20 sessions). Compliance was evaluated with RPE, visual analog scale for muscle soreness and monitoring of heart rate (HR). Functional parameters were measured by the distance walked and the VO 2 uptake during the 6-minute walk test (6MWT) before and after training.
Results
Two patients were excluded due to adverse effects in each group. RPE was 9–11 in ECC training while it reached 12–14 in CON training. HR remained stable in ECC group during exercise whereas it increased during CON exercise. 6MWT distance improved in both group (ECC: +53 m; CON: +33 m). 6MWT VO 2 uptake remained stable in ECC group whereas it increased in CON group.
Conclusion
ECC training tailored by RPE appears to be an efficient and safe alternative for CHF patients. Indeed, it induces functional improvement similar to conventional CON training with lower demand on the cardiovascular system during exercise.
Résumé
Objectifs
Évaluer au cours de l’insuffisance cardiaque chronique (ICC), faisabilité, sécurité, compliance et amélioration fonctionnelle liées à un entraînement excentrique (ECC), personnalisé sur le niveau de perception de l’effort (RPE ; 9–11 échelle de Borg), comparativement à un entraînement concentrique (CON) à une puissance correspondant au premier seuil ventilatoire.
Méthode
Trente patients inclus et randomisé soit dans un entraînement ECC soit CON (20 sessions). La tolérance était évaluée par RPE, échelle visuelle analogique (douleurs musculaires) et fréquence cardiaque (FC). Les paramètres fonctionnels étaient la distance parcourue, la VO 2 durant un test de marche de six minutes (6MWT).
Résultats
Deux patients furent exclus pour effets indésirables dans chacun des groupes. La RPE était à 9–11 dans le groupe ECC et à 12–14 dans le groupe CON. La FC n’augmentait que dans le groupe CON. La distance du 6MWT était améliorée dans les deux groupes (ECC : +53 m ; CON : +33 m). La VO 2 au cours du 6MWT était stable dans le groupe ECC mais augmentée dans le groupe CON.
Conclusion
L’entraînement ECC personnalisé par RPE est une alternative efficace et sans danger au cours de l’ICC. L’amélioration fonctionnelle est similaire à celle obtenue lors d’un entraînement CON mais avec une sollicitation moindre du système cardiovasculaire.
1
English version
1.1
Introduction
Chronic heart failure (CHF) is a frequent disease affecting about 1,000,000 people in France, with growing incidence (120,000 new cases a year) . This is mainly due to an increase in life expectancy and to the advances in medical care during the acute phase of cardiovascular diseases. Asthenia and dyspnea are the main symptoms of CHF exercise intolerance, due to the alterations of the cardiac pump, but also to the muscle atrophy with impairment of skeletal muscle oxidative metabolism . These symptoms and potential cardiac risks, led to the exclusion of CHF patients from cardiac rehabilitations (CR) programs. However, it is now proven that exercise training is beneficial in patients with CHF, especially for the improvement of cardiorespiratory system and functional capacities , and the decrease of perceived fatigue and dyspnea . Quality of life is thus markedly improved by CR , but sometimes, by its severity, deconditioning represents a barrier to the comprehensive management of these patients.
At an early stage of CR of CHF patients, eccentric (ECC) training could be an interesting approach. Indeed, for healthy subjects, compared with conventional concentric (CON) training, ECC training leads to a greater gain in muscle strength, with lower energy expenditure and less demand on the cardiorespiratory system . However, ECC training is still underused in clinical practice in the field of physical exercise and rehabilitation. This is certainly due to fear of inducing pain or muscle damage, such as “delayed onset muscle soreness” (DOMS) or “exercise-induced muscle damage” (EIMD), observed when ECC exercise is used at a supramaximal level in athletic training . This poor tolerance to high-intensity ECC exercise is commonly reported and continues to limit its use in everyday clinical practice. Nonetheless, it has been shown that prior moderate-intensity ECC exercise has a protective effect on these muscle lesions and their consequences in terms of loss of capacity to produce strength . Moreover, several studies have shown the good tolerance and positive effects of submaximal ECC training, using a specific mode of personalizing ECC exercise, perceived exertion-based, in healthy subjects or in patients with chronic cardiorespiratory diseases without CHF . Thus, ECC training appears to be a potentially effective alternative to CON training in deconditioned subjects such as CHF, particularly for an exercise prescription at the initial stage of CR.
The aims of this study were therefore to evaluate, in CHF patients:
- •
the feasibility, the safety and the compliance of ECC training protocol;
- •
the functional improvement linked to ECC training, compared to CON training.
1.2
Subjects and methods
1.2.1
Subjects
Patients matching with the following criteria were included in this study: man or woman, aged between 45 and 80 years, with stable CHF diagnosis (left ventricular ejection fraction < 45% using the echocardiographic Simpson method) or plasma N-terminal pro-brain natriuretic peptide (NT pro-BNP level) three times superior to accepted value in healthy subjects in our hospital laboratory, New York Heart Association (NYHA) class superior or equal to 2. Patients were excluded if they suffered from severe obstructive heart disease, aortic valve stenosis, severe heart rhythm disorder during initial stress test, intracavitary thrombosis, severe pulmonary hypertension (>70 mmHg), venous thromboembolic history within the past 3 months, heart transplantation, and any associated disease limiting functional capacity beyond the CHF itself. Informed written consent approved by the local ethics committee was obtained for all participants after they had been informed of all potential risks, discomfort and benefits involved in the study. The study was registered by the French “ Agence nationale de sécurité du médicament ” (ANSM) database under reference no 2009-A01265-52.
1.2.2
Protocol design
After inclusion, the patients were randomly allocated to the CON training group or the ECC training group. All subjects followed the same rehabilitation protocol, including exercise training (3 sessions/week, during 7 weeks), associated with individual educational interventions based on the patient’s risk factors. All patients performed a prior graded maximal exercise test on a conventional cycle ergometer, with assessment of breath-by-breath gas exchange (K4b 2 , Cosmed, Italy) before entering the training procedure, in order to rule out any contra-indications, and to individualize training intensity for the CON group.
1.2.3
Training procedure
Patients had to perform 20 sessions of 32 minutes of cycling:
- •
in the CON group, workout was performed on a standard cycle ergometer (Custo med GmbH, Groz EC3000, Ottobrunn, Germany). After a 5-minute warm-up at half the target workload, they performed a 25-minute CON cycling bout at 60 revolutions per minute (RPM), at a workload leading to a heart rate (HR) target corresponding to the first ventilatory threshold determined by the Wasserman method during the initial graded maximal exercise test . HR was monitored with a HR device (Polar FT7) throughout the session. The workload exercise was adapted, if necessary (HR decrease of 5 beats per minute (BPM) for the same workload), every five sessions to match HR targeting. Each session ended with a 2-minute active recovery period at a workload corresponding to half the target workload, at 60 RPM;
- •
in the ECC group, patients performed a preconditioning session on the ECC semi-recumbent prototype (Tech med Tm, France; for detailed description ) before starting the training. During this former session, each patient was assisted by a physiotherapist who gave him some instructions about how to resist against the pedal during the cycle. This session was performed to maximize compliance and avoid DOMS and to manage patients’ training in safety and autonomy on the ergocycle prototype. During ECC training sessions, the pedal speed was set at 10 RPM during the 5-minute warm-up, then 15 RPM during 25 minutes. Even though energy efficiency is optimal at between 50 and 60 RPM for a CON ergocycle , we chose to impose a pedaling rate of 15 RPM during the ECC sessions because rotational ECC exercise was shown to be better tolerated at slow speed . Patients were instructed to resist to the pedaling movement without pulling upwards against the foot strap, in order to reach a rate of perceived exertion (RPE) between 9–11 on Borg scale (rated as “very light” and “fairly light”). If needed, they were asked to increase the resistance provided on the pedals every five sessions, in order to stay in this range on RPE. HR was checked regularly in order to not exceed 80% of maximum HR. The rotation speed was gradually decreased during the 2-minute active recovery period, until total stop of the motor.
1.2.4
Measurements
1.2.4.1
Six-minute walk test (6MWT)
This test has been shown to be highly correlated with functional capacities and to be useful as predictor of all-causes of hospitalization and all-cause of mortality . Patients performed two 6MWT, before (S0) and at the end (S20) of the CR program. This test was performed on a 50-meter unobstructed corridor. Each patient was instructed to walk at his self-selected (comfortable) pace and was informed on the time due every 2 minutes. Slowing down and stopping to rest were allowed . Patients did not perform familiarization test, as learning effect was shown to be trivial in CHF patients with poor walking abilities . The total distance walked was measured (6MWD), as well as averaged HR and oxygen uptake during the last 30 seconds, measured by portable device (k4b 2 , Cosmed, Italy).
1.2.4.2
Rate of perceived exertion and visual analogic scale (VAS)
At the end of each training session, patient reported the perceived level of exertion on 6–20 Borg scale and the pain related to muscle soreness on a VAS (0–10. 0: no pain and 10: unbearable pain). Patients were excluded if VAS exceeded 5 at the beginning of the subsequent session. Each patient’s HR was monitored throughout all training sessions and was averaged by bloc of five sessions.
1.2.4.3
N-terminal pro-brain natriuretic peptide
Blood sample was taken in patients of both groups every five training sessions in order to measure level of NT pro-BNP. The measure was given in pg/mL.
1.2.5
Statistical analysis
Statistical analyses were performed using Statistica ® (the statsoft, USA) for Windows ® . Each parameter was averaged and presented as a means ± standard deviation (SD). Due to exploratory nature of the study and the small number of patients, the Mann-Whitney test was used to assess difference between groups at each time (five times comparison). Wilcoxon paired test was used to examine the effect of training (five times comparison in the same group). The Bonferroni correction was applied to those tests. A P -value < 0.01 was considered significant. Statistical Differences between S0 and S20 for the 6MWTparameters (distance, HR, and VO 2 ) was considered significant for P < 0.05.
1.3
Results
1.3.1
Patients
Thirty patients aged between 45 and 80 years were included in this study. Their main anthropometric and clinical characteristics are presented in Table 1 . Briefly, they were mainly slightly overweight males, with a moderate alteration of ventricular function, but mean NT pro-BNP level superior to 10 fold accepted superior value of the laboratory (no significant difference between groups; Mann-Whitney, P > 0.24). As expected, modifications of NT pro-BNP levels were significantly different between S0 and S20 in CON group (Wilcoxon, P < 0.002) and not different for ECC group (Wilcoxon, P > 0.05). Medications were similar between the two groups ( Table 1 ).
| Concentric group | Eccentric group | |
|---|---|---|
| Patients (men/women) | 15 (11/4) | 15 (11/4) |
| Age (mean ± SD) | 60.7 ± 11.8 years | 63.3 ± 10.1 years |
| Height (mean ± SD) | 170.0 ± 7.0 cm | 170.9 ± 7.8 cm |
| Weight (mean ± SD) | 74.7 ± 14.5 kg | 70.3 ± 15.6 kg |
| NT pro-BNP at inclusion (mean ± SD) | 1336 ± 1555 pg/mL | 1640 ± 2249 pg/mL |
| LVEF (% ventricular capacity) | 43.42 ± 15.81 | 39.6 ± 14.7 |
| VO 2peak (mean ± SD) | 19.1 ± 5.2 mL/min per kg | 17.0 ± 4.9 mL/min per kg |
| Medications (number of patients) | ||
| Beta blocker | 15 | 15 |
| CEI | 11 | 14 |
| ARA2 | 3 | 1 |
| Anti-aldosterone | 1 | 2 |
| Diuretic | 7 | 9 |
| Statin | 12 | 12 |
| Anticoagulant | 1 | 3 |
| Antiplatelet | 12 | 13 |
1.3.2
Tolerance
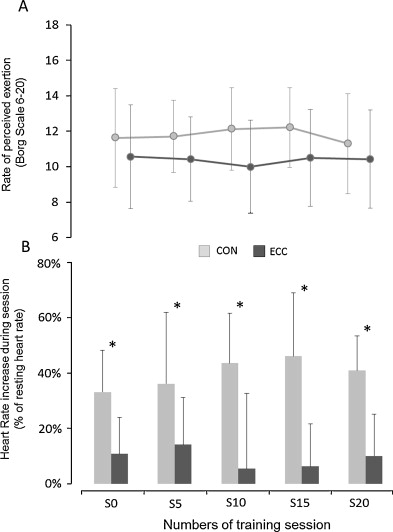
All of the exercise and testing procedures were well tolerated. The ECC trained patients had no difficulty to understand the training instructions. During training sessions, patients in ECC training rated RPE between 9 and 11 during the 20 sessions of the training program, while those in the CON group rated between 10 and 12 (no difference at each time session considered: Mann-Whitney P > 0.05). The Fig. 1 A shows the detailed values of the RPE for each group, throughout training program.
1.3.3
Assessment of pain
Concerning the assessment of pain, the specific VAS was close to zero in both groups at each time. One patient of the ECC group suffered of knee pain and another of diffuse thigh pain (VAS > 7) and were therefore excluded. The former suffered from a knee osteoarthritis that did not limit his performance neither during initial graded test nor during 6MWT. In CON group, one patient complained of diffuse muscle pain and one patient was excluded due to acute decompensated heart failure apparently not related to training. Two patients in CON training and one in ECC training complained of muscular or joint pain (VAS > 7) during 48 hours. One patient suffered of arrhythmia during ECC but without any complication, leading to a well tolerated modification in medication. All other patients were highly compliant with training procedures.
1.3.4
Resting heart rate (HR)
Values (before starting session), in each group were not different at each time considered (Mann-Whitney, P > 0.33). During exercise, relative increase in HR throughout session was significantly higher in CON group than in ECC group (34% to 52% and 8% to 17%; respectively, Mann-Whitney, P < 0.007; Fig. 1 B).
1.3.5
Functional capacities
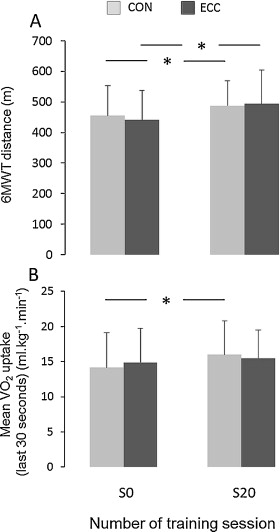
6MWT relative improvements were significant for the ECC and CON training group (53 m increment for ECC group, Wilcoxon P < 0.03; and 33 m increment for CON group, Wilcoxon P < 0.03; Fig. 2A ). Cardiopulmonary response to the 6MWT after training was found to differ only in CON group, with an increase of VO 2 uptake during the last 30 seconds at S20 compared to S0 (+13% Wilcoxon, P < 0.03; Fig. 2 B).
1.4
Discussion
Our results shown that this type of ECC training on a semi-recumbent cycle ergometer tailored on Borg scale is well tolerated and can be implemented in patients with CHF with a good compliance. Despite the low stress induced by ECC exercise on the cardiovascular system, functional capacities increased in ECC groups after 20 training sessions in a similar way than in CON group. Moreover, bio-energetic response during the 6MWT is markedly lower in ECC group than in CON group at the end of the training protocol.
To the best of our knowledge, this is the first study to report feasibility and tolerance of this mode of ECC exercise in CHF patients. In fact, in our work, the rate of tolerance was comparable in both groups and we did not witness any serious side effects. Our training protocol was different to that usually performed in most of the studies investigating the effects of ECC training in chronic diseases, such as coronary artery disease (CAD) or chronic obstructive pulmonary disease. These works usually compared ECC training with CON training at the same metabolic exercise intensity or workload (between 60 and 65% of the VO 2 peak or at 85% of the peak HR) . However, the results concerning the tolerance are conflicting. Some studies demonstrated that ECC training is feasible and as well – or even better – tolerated as CON training . In contrast, one other study found a lesser tolerance from the beginning of the ECC training . Some studies have shown that a preconditioning session could improve the tolerance due to the protective effect of ECC training .
However, there is no specific recommendation yet on how to determine the initial ECC exercise intensity and how to increment the intensity during training program in deconditioned patients. In our protocol, RPE target was easily achieved without pain, from the first sessions. The preconditioning session performed might partly explain the good tolerance of our training protocol. In addition, our prior experience in the use of this ECC ergocycle confirmed the better muscle tolerance at 15 RPM in both healthy and CAD subjects . This low rotation speed probably decreases the difficulties in coordinating ECC movement. Indeed, ECC contraction involves more complex neuromotor task than CON contraction, as it requires recruitment of larger areas of the cortex .
We did not assess the force applied on the pedals, but we have previously demonstrated in healthy subjects that a rating of 12 on Borg scale during CON exercise leads to a RPE of 8 for an iso-workload ECC cycling exercise . Moreover, this 12 level in CON cycling exercise has been previously shown to roughly correspond to an effort performed at the first ventilator threshold level in CAD patients . In our study, patients in ECC group have shown a RPE between 9 and 11 during exercise, associated with an improvement of distance walked without increase of VO 2 uptake during 6MWT. Hence, some studies have suggested that this could be related to an increased participation of anaerobic metabolism during ECC training . Other studies propose the involvement of a strong elastic component in ECC exercises , with a reduced use of adenosine triphosphate and an improvement in strength . These properties could be transferred during walking and thus lead to its greater metabolic efficiency after ECC training. This may optimize muscular contraction and power output, with greater solicitation of fast muscle fibers, potentially allowing an increase in walking speed and an improvement in participation in daily activities. This improvement in muscle strength could partly explain the discrepancy between functional improvement and the lesser aerobic capacities increase during ECC training . Such results are to be highlighted because of its potential implications for deconditioned patients, to improve their functional capacities, autonomy and quality of life. In this study, 6MWT significantly increased in both groups, confirming previous works in CAD patients , or in cardiopulmonary diseases patients . 6MWT is known to be useful tool for the assessment of benefits following CR, strongly correlated with changes in symptoms in CHF patients , aerobic capacity and NYHA functional class .
1.4.1
Limits
Some potential limitations of the study should be considered. This is a pilot study on a relatively small sample of highly selected patients, and thus the statistical power is low. Hence, our results have to be considered with caution and they need to be confirmed on a larger sample with various severity of CHF. On the other hand, the advantage inherent in this limitation is that only very strong relationships could be demonstrated.
The total work during sessions was not recorded. However, it is of lesser importance because the internal mechanical power, determined by all of the internal forces involved in the movement (inertia, frictions, work done against gravity…), is widely different in CON and ECC exercises . The quantification of the effort remained subjective for ECC patients, compared to CON group. Indeed, in ECC, patients increased the pedalling resistance in order to reach a 9–11 level on Borg scale, but we could not check out the power output, while on the bike CON we controlled the workload increase. However, we observe interesting results in terms of functional improvement, which remains the main goal of CR. This also indicates that patients are able to manage themselves their effort level based on Borg scale during ECC exercise .
1.5
Conclusion
Based on different findings in previous studies regarding its physiological properties and on our results, ECC training RPE-based appears to be an efficient and safe alternative for CHF patients, even at the early stage of CR. It may induce functional improvement similar to conventional CON training, with a lower demand on the cardiovascular system during exercise. Further studies are needed to confirm these results, investigate more thoroughly its effects, and to help optimize the design of ECC training protocols in patients with chronic cardiorespiratory diseases.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
The authors thank A. Hannequin, C. Lejeune and A. Dedoncker for their roles during training and tests and all patients for their participation. The present study was supported by the “Fondation de l’Avenir pour la Recherche Médicale Appliquée” (study n o ET8-518), Paris, France.
Professional relationships with manufacturer: the ergometer prototype was designed in partnership with Technologies machines spéciales (TMS, Tech Med ® ) and Holiste, and was manufactured by TMS. A research collaboration contract has been signed between the Dijon university hospital and TMS.
2
Version française
2.1
Introduction
L’insuffisance cardiaque chronique (ICC) est une pathologie fréquente touchant environ 1 000 000 de personnes en France, avec une incidence en constante augmentation (120 000 nouveaux cas par an) . Cela peut s’expliquer notamment par une augmentation de l’espérance de vie et les progrès lors de la prise en charge médicale au cours de la phase aiguë des maladies cardiovasculaires. La fatigue et la dyspnée sont les symptômes principaux de l’intolérance à l’exercice chez le patient ICC, tout d’abord à cause de l’altération de la pompe cardiaque, mais également de la dégradation du métabolisme oxydatif musculaire avec amyotrophie, perte de force et d’endurance . Ces symptômes et les risques cardiovasculaires potentiels ont longtemps conduit à exclure les patients en ICC des programmes de réadaptation cardiaque (RC). Cependant, il est maintenant prouvé que l’entraînement est bénéfique pour les patients ICC, tout spécialement du fait de l’amélioration du système cardiorespiratoire et des capacités fonctionnelles , ainsi que d’une diminution de la fatigue perçue et de la dyspnée . La qualité de vie des patients ICC peut donc être notablement améliorée par la RC , mais parfois, par sa gravité, le déconditionnement représente une barrière à la prise en charge de ces patients.
À la phase initiale de la RC des patients ICC, l’entraînement excentrique (ECC) pourrait être une approche intéressante. En effet, chez le sujet sain, comparé avec l’exercice concentrique (CON) traditionnel, l’entraînement ECC permet un gain de force musculaire plus important, avec une dépense énergétique plus faible et une sollicitation moindre du système cardiorespiratoire . Cependant, l’entraînement ECC reste sous-utilisé en pratique clinique courante de reconditionnement à l’effort et de rééducation. Cela est certainement dû à la crainte d’entraîner des douleurs ( delayed onset muscle soreness [DOMS]) ou des lésions musculaires ( exercise-induced muscle damage [EIMD]), telles que celles, observées lorsque l’exercice ECC est utilisé à une intensité supramaximale au cours de l’entraînement sportif . Cette mauvaise tolérance à l’exercice ECC a été fréquemment rapportée dans la littérature et contribue à limiter son utilisation en pratique clinique. Néanmoins, il a été rapporté qu’un entraînement ECC préalable d’intensité modérée a un effet préventif sur ces lésions musculaires et leurs conséquences en termes de perte de capacité à produire de la force . De plus, certaines études ont rapporté la bonne tolérance et les effets positifs d’un entraînement ECC d’intensité sous-maximale utilisant un mode de personnalisation basé sur la perception de la fatigue, chez le sujet sain ou chez les patients atteints de maladies cardiorespiratoires chroniques sans ICC . L’entraînement ECC peut donc représenter une alternative intéressante à l’entraînement CON pour les patients déconditionnés à l’effort – comme au cours de l’ICC –, tout particulièrement à la phase initiale de la RC.
Les objectifs de cette étude étaient donc d’évaluer chez les patients ICC :
- •
la faisabilité, la sécurité et la compliance à un protocole d’entraînement ECC ;
- •
l’amélioration fonctionnelle à l’issue de ce protocole ECC comparée à un entraînement CON.
2.2
Sujets et méthodes
2.2.1
Sujets
Les critères d’inclusion étaient : homme ou femme ; entre 45 et 80 ans, diagnostic d’ICC stable (fraction d’éjection du ventricule gauche < 45 % mesurée par échocardiographie trans-thoracique selon la méthode de Simpson), ou dosage de plasma N-terminal pro-brain natriuretic peptide (NT pro-BNP) trois fois supérieur aux valeurs retenues chez le sujet sain par notre laboratoire hospitalier d’analyses biologiques, et enfin classe supérieur ou égal à 2 sur l’échelle de la New York Heart Association (NYHA). Les critères d’exclusion étaient : cardiomyopathie obstructive sévère, rétrécissement valvulaire aortique, troubles sévères du rythme cardiaque durant l’épreuve d’effort initiale, thrombus intra cavitaire, hypertension artérielle pulmonaire sévère (> 70 mm Hg), antécédents de maladie thromboembolique veineuse au cours des trois derniers mois, transplantation cardiaque et tout autre pathologie associée à l’ICC limitant d’autant plus la capacité fonctionnelle. Après avoir reçu une information complète sur les risques potentiels, inconforts et bénéfices de l’étude, les patients ont signé un consentement éclairé, préalablement approuvé par le Comité local de protection des personnes. L’étude était enregistrée auprès de l’Agence nationale de sécurité du médicament (ANSM) sous la référence n o 2009-A01265-52.
2.2.2
Déroulement du protocole
Après inclusion, les patients étaient randomisés dans l’un des deux groupes d’entraînement, le groupe CON ou le groupe ECC. Tous les sujets ont suivi le même protocole de réadaptation qui comprenait un reconditionnement à l’effort (trois sessions/semaine, pendant sept semaines), ainsi que des sessions d’éducation thérapeutique individualisées en fonction des facteurs de risque du patient. Tous les patients ont bénéficié préalablement d’une épreuve maximale d’effort sur un cyclo-ergomètre conventionnel, avec mesures des échanges gazeux (K4b 2 , Cosmed, Italie) avant de commencer le protocole d’entraînement, afin d’éliminer toute éventuelle contre-indication, et d’individualiser l’intensité de l’entraînement pour le groupe CON.
2.2.3
Déroulement de l’entraînement
Les patients devaient compléter 20 sessions d’exercice sur cyclo-ergomètre de 32 minutes chacune :
- •
dans le groupe CON, l’exercice se faisait sur un cyclo-ergomètre traditionnel (Custo med GmbH, Groz EC3000, Ottobrunn, Allemagne). Après cinq minutes d’échauffement, les patients effectuaient une session de 25 minutes de pédalage CON à 60 tours par minute (tr/min), avec une charge de travail permettant d’atteindre la fréquence cardiaque (FC) cible correspondant au 1er seuil ventilatoire calculé selon la méthode de Wasserman lors de l’épreuve d’effort initiale . Pour la surveillance de la FC un cardiofréquencemètre (Polar FT7) été utilisé tout au long de chaque session. Si nécessaire, l’intensité de l’exercice était adaptée (baisse de la FC de cinq battements par minute pour la même charge de travail), toutes les cinq sessions pour atteindre la FC cible. Chaque session se terminait par une période de deux minutes de récupération active, avec une charge de travail correspondant à la moitié de la charge cible à 60 tr/min ;
- •
dans le groupe ECC, les patients commençaient par une session de préconditionnement sur un cyclo-ergomètre ECC prototype en position semi-allongé (Tech med Tm, France ; pour une description détaillée ), avant de commencer l’entraînement. Durant cette pré-session, un kinésithérapeute donnait des instructions aux patients sur la force de résistance à appliquer sur les pédales à chaque cycle du pédalier. Cette session était destinée à favoriser la compliance et à prévenir les DOMS, tout en s’assurant que l’entraînement des patients se déroulait en toute sécurité et en autonomie sur le cyclo-ergomètre ECC. Durant les sessions d’entraînement ECC ; la vitesse de pédalage était fixée à 10 tr/min pendant l’échauffement de cinq minutes et ensuite à 15 tr/min au cours des 25 minutes suivantes. Bien que l’efficience énergétique soit optimale entre 50 et 60 tr/min pour un cyclo-ergomètre CON, , nous avons choisi d’imposer une fréquence de pédalage de 15 tr/min pendant les sessions ECC car il a été montré que l’exercice de pédalage ECC était mieux toléré à vitesse lente . Les patients avaient comme instruction de résister au mouvement de rotation du pédalier, jusqu’à atteindre un niveau de perception de la fatigue (RPE) situé entre 9–11 sur l’échelle de Borg (c’est-à-dire « très facile » ou « assez facile »). Si nécessaire, les patients devait augmenter cette résistance à chaque bloc de cinq sessions, afin de rester au même niveau de RPE. La fréquence cardiaque était surveillée, afin de ne pas dépasser 80 % de la FCmax. La vitesse de pédalage était diminuée graduellement pendant les deux minutes de récupération active, jusqu’à l’arrêt total du moteur.
2.2.4
Mesures
2.2.4.1
Le test de marche de six minutes (6MWT)
Il a été démontré que ce test était hautement corrélé aux capacités fonctionnelles des patients et qu’il était un moyen utile de prédire le risque d’hospitalisations et de mortalité de toute origine . Les patients effectuaient deux 6MWT, avant (S0) et à la fin (S20) du programme de réadaptation. Ce test se déroulait dans un couloir de 50 mètres de long, libre de tout obstacle. Les instructions données aux patients étaient de marcher à une vitesse confortable et ils étaient informés du temps écoulé toutes les deux minutes. Les patients pouvaient ralentir et se reposer si nécessaire . Il n’y avait pas de test de familiarisation avec le 6MWT, car il a été démontré qu’un apprentissage était inutile chez les patients en ICC avec de faibles capacités de marche . La distance totale parcourue était mesurée (6MWD), ainsi que la FC moyenne et la consommation d’oxygène (VO 2 ) au cours des dernières 30 secondes à l’aide d’un appareil portable (k4b 2 , Cosmed, Italie).
2.2.4.2
Perception de la fatigue et échelle visuelle analogique (EVA)
À la fin de chaque session d’entraînement, le patient rapportait son niveau de fatigue perçue de 6 à 20 sur l’échelle de Borg et ses douleurs musculaires éventuelles à l’aide d’une EVA (0–10. 0 : aucune douleur et 10 : douleur insoutenable). Les patients étaient exclus si leur EVA était supérieure à 5 au début de la session d’entraînement suivante. La FC de chaque patient était surveillée tout au long des sessions et une moyenne était calculée par tranche de cinq sessions.
2.2.4.3
N-terminal pro-brain natriuretic peptide
Un échantillon de sang était prélevé sur chaque patient dans les deux groupes et cela toutes les cinq sessions d’entraînement afin de mesurer le niveau de NT pro-BNP. Le résultat était donné en pg/mL.
2.2.5
Analyse statistique
Les analyses statistiques ont été réalisées avec le logiciel Statistica ® (StatSoft, États-Unis) pour Windows ® . Chaque paramètre était présenté en tant que moyenne ± écart-type (SD). Au vu de la nature préliminaire de l’étude et du faible nombre de patients, le test de Mann-Whitney a été utilisé pour comparer la différence entre chaque groupe à chaque fois (comparaison des 5 blocs de sessions au cours du protocole). Le test apparié de Wilcoxon a servi à examiner l’impact de l’entraînement (comparaison de 5 temps dans le même groupe). La correction de Bonferroni était appliquée à tous ces tests. Une valeur p < 0,01 était considérée comme significative. Pour les paramètres du 6MWT (distance, FC et VO 2 ), les différences statistiques entre S0 et S20 étaient jugées significatives pour p < 0,05.
2.3
Résultats
2.3.1
Patients
Trente patients dont l’âge variait entre 45 et 80 ans ont été inclus dans cette étude. Leurs principales caractéristiques cliniques et anthropométriques sont présentées dans le Tableau 1 . Brièvement, la plupart d’entre eux étaient des hommes en léger surpoids, avec une altération modérée de la fonction ventriculaire, mais avec une moyenne de NT pro-BNP dix fois plus élevée que la valeur supérieure acceptée comme normale par le laboratoire d’analyse de notre hôpital (aucune différence significative entre les groupes ; Mann-Whitney, p > 0,24). Comme attendu, les changements de niveau de NT pro-BNP étaient significativement différents entre S0 et S20 dans le groupe CON (Wilcoxon, p < 0,002) et à l’inverse aucune différence n’était notée dans le groupe ECC (Wilcoxon, p > 0,05). Les traitements médicamenteux étaient similaires dans les deux groupes ( Tableau 1 ).







