Abstract
Objective
To establish the value of an early post-stroke evaluation of cardiorespiratory fitness in hemiparetic patients using a one-leg cycling exercise test and to analyze the impact of an adapted physical activity programme 12 weeks after the stroke.
Protocol
Eighteen hemiparetic stroke patients participated in the study. The subjects were randomly assigned to one of two groups: the control group (CG) underwent 4 weeks of conventional rehabilitation, whereas the training group (TG) performed additional physical exercises. The initial evaluation (T1) was carried out after 1 week of exercise and the final evaluation (T2) was performed after 28 days. Both evaluations consisted of maximal graded tests performed with the valid leg, followed by completion of a questionnaire on personal autonomy in activities of daily living (ADL).
Results
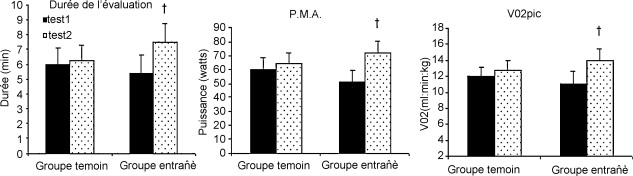
In the CG group, we recorded a 4 to 8% increase in peak oxygen uptake ( VO 2 peak). There was no significant increase in peak power output (Wpeak). However, the TG displayed significantly ( P < 0.05) greater peak values than those recorded on study entry (Wpeak: +30%, VO 2 peak: +20%). The TG showed a statistically significant improvement in the Barthel and Katz ADL scale scores, whereas the pre- and post-rehabilitation values did not differ significantly in the CG. However, there was no correlation between the Barthel/Katz scale scores and Wpeak.
Conclusion
Evaluation of cardiorespiratory fitness by using the valid leg seems to be feasible in hemiplegic patients 1 month post-stroke. Early post-stroke physical training appears to be needed to limit the negative effects of functional hypoactivity.
Résumé
Objectif
Montrer l’intérêt de l’évaluation précoce de l’aptitude aérobie chez des personnes hémiplégiques à partir d’un pédalage unilatéral et analyser chez ces patients, l’impact d’un reconditionnement à l’effort réalisé moins de 12 semaines après l’accident vasculaire cérébral (AVC).
Protocole
Dix-huit patients hémiplégiques, répartis de manière aléatoire en deux groupes de neuf, ont participé à cette étude. Les sujets ont été évalués à quatre semaines d’intervalle. L’évaluation initiale a été effectuée dès l’entrée dans le service soit en moyenne 21 jours après l’AVC. Les évaluations consistaient en une épreuve d’effort maximale réalisée à partir du membre inférieur valide, suivie de questionnaires évaluant l’autonomie. Le groupe témoin a bénéficié d’une rééducation pluridisciplinaire sans reconditionnement à l’effort tandis que le groupe entraîné a bénéficié en supplément d’un programme en activités physiques adaptées (APA).
Résultats
Une augmentation non significative ( p < 0,05) de la puissance maximale aérobie (PMA) et de la consommation pic d’oxygène ( VO 2 pic) de 4 et 8 % est enregistrée chez le groupe témoin. En revanche, le groupe entraîné obtenait des valeurs pics supérieures, comparativement aux valeurs d’entrée (PMA: +30 %; VO 2 pic: +20 %). Les scores enregistrés avec l’échelle de Barthel et de Katz sont statistiquement inchangés pour le groupe témoin signifiant l’absence d’amélioration de l’autonomie à la différence des scores du groupe entraîné qui ont significativement progressé. Aucune corrélation n’a été trouvée entre les scores de Barthel et Katz et la PMA.
Conclusion
Une épreuve d’effort effectuée à partir d’un pédalage unilatéral semble tout a fait réalisable chez des patients hémiplégiques à un mois de l’AVC. Un reconditionnement à l’effort précoce semble nécessaire pour limiter les effets de l’hypoactivité fonctionnelle et permettre au patient de participer pleinement à sa rééducation.
1
English version
1.1
Introduction
Stroke is the third-ranked cause of mortality after myocardial infarction and cancer. It constitutes the leading cause of acquired handicap in adults . After the age of 60, this pathology is the leading cause of death in women and the second-ranked cause in men. The frequency, severity and cost of stroke make it an important public health problem. In 2002, the French National Agency for Accreditation and Evaluation (ANAES) emphasized the importance of functional and cardiovascular deconditioning in stroke patients. The severity of this deconditioning depends on the lesion’s location and size . Ramas et al. reported that exercise capacities are 25 to 45% lower in hemiplegic patients than in age-matched, healthy subjects. After a stroke, the maximum oxygen consumption ( VO 2 ) falls to a mean value of between 10 and 20 ml/kg per minute. Given that a value of 15 ml/kg per minute is required to perform most activities of daily living (ADL), improving the VO 2 during rehabilitation becomes a crucial issue. In a study of hemiplegic vascular stroke patients, Courbon et al. found a significant relationship between the maximal effort and walking ability. A certain number of studies have highlighted the importance of post-stroke exercise training . In view of these observations, it is essential that healthcare establishment offer their patients muscle strengthening and cardiovascular training programmes. To counter deconditioning and accelerate recovery, stroke rehabilitation protocols indeed recommend cardiorespiratory training but there is no consensus on training in a broader sense.
In fact, there are significant disparities in the literature concerning the intensity, frequency and duration of exercise and the equipment to be used (treadmills, cycle ergometers, etc.) . There is also heterogeneity in terms of the time interval between the initial stroke and the start of the training programme (generally very long – over a year ). We believe that this time interval is too long, in view of the average length of a hemiplegic patient’s stay in a rehabilitation unit. In fact, the crucial period for rehabilitation is between 3 and 6 months post-stroke , meaning that rehabilitation should start as soon as possible. The neurological consequences of hemiplegia and improvements in the affected leg may limit the reliability of the effort tests described in the literature. This is why most researchers only perform cardiorespiratory evaluations 6 months after the accident, when neurological symptoms have stabilized. Nevertheless, Tang et al. have demonstrated the feasibility of testing soon after the stroke. Implementation of an early post-stroke evaluation (on a treadmill with bodyweight support) has also been suggested by MacKay-Lyons and Makrides . However, VO 2 measurement is difficult in this type of protocol. To counter this problem, the evaluation could be performed with the valid leg, since the feasibility of this approach has been demonstrated in patients with orthopaedic conditions . To the best of our knowledge, the impact of a training programme (based on one-leg cycling) 1 month after stroke has not previously been studied.
Thus, the main objective of the present study was to show that a one-leg cycling evaluation of the aerobic capacity in hemiplegic patients is feasible soon after stroke. Our study also sought to determine the effects of exercise training initiated only a few weeks after the stroke.
1.2
Patients and methods
1.2.1
Population
Eighteen hemiplegic patients participated in the study. The subjects’ anthropometric measurements are given in Table 1 . At the start of the study, the mean time since stroke was 20 ± 2 days, with uninterrupted hospitalization. The inclusion criteria were as follows: right or left hemiplegia following ischaemic or haemorrhagic hemispheric stroke; a full set of aetiological data (CT and/or MRI scans, Holter ECG, Doppler, cardiac ultrasound); a stable clinical state; well-balanced treatment (particular in terms of antihypertensives and anticoagulants). The exclusion criteria were as follows: existence of disorders associated with hemiplegic motor damage, such as cognitive and memory disorders; hemisensory neglect; the existence of an intercurrent affection or unstable brain lesions. The volunteer subjects had received information on the study goals and procedures and had given provided their written, informed consent. The study’s protocol and ethical aspects were approved by our hospital’s investigational review board.
| Control group, n = 9 | Trained group, n = 9 | |
|---|---|---|
| Age (years) | 60.6 ± 8.2 | 59.1 ± 9.4 |
| Time since stroke | 20 ± 2 | 21 ± 3 |
| Number of women | 3 | 4 |
| Number of men | 6 | 5 |
| Ischaemic stroke | 5 | 5 |
| Haemorrhagic stroke | 4 | 4 |
| Left-side stroke | 5 | 5 |
| Right-side stroke | 4 | 4 |
1.2.2
Experimental protocol
The study population was randomized into two groups of nine subjects. The subjects were evaluated twice, with a 4-week interval. The initial evaluation was performed as soon as the subject entered the service, i.e. around 3 weeks after the stroke. All the tests took place in the afternoon, under similar conditions. They consisted in a maximal effort test performed on the valid leg, followed by the completion of questionnaires evaluating personal autonomy. The control group underwent a standardized, multidisciplinary rehabilitation programme (comprising physiotherapy, occupational therapy and neuropsychological/speech therapy) in the absence of exercise training, whereas the trained group performed an additional adapted physical activity (APA) programme.
1.2.3
The maximal aerobic power tests
The patients performed a triangular maximal aerobic power (MAP) test using a standard cycle ergometer equipped with an electromagnetic brake (TUNTURI E80). To facilitate the pedalling action, the pedal on the affected side was removed and replaced by a 2 kg weight, which served as a counterweight and thus increased the inertia of the movement . The foot of the pedalling leg was strapped to the pedal with a Velcro band. The affected limb was not attached and the foot was positioned on a foam cushion. The initial target power level was set to 30 W, with the power then increasing in 10-W steps every 2 minutes. Subjects were told to reach the highest possible power level and were given verbal encouragement throughout the test. The subjects were free to choose their own pedalling frequency. The test ended when the subject was unable to maintain the effort and/or when cardiac risks appeared on the ECG. Respiratory parameters ( VO 2 ) were measured continuously with an open-circuit exercise spirometer (the CPX (D) from Medical Graphics, Saint-Paul, MN, USA). The system was calibrated before each evaluation, according to the manufacturer’s recommendations. The data were averaged by taking the last 10 seconds of each step. The parameters used in the present study were the MAP, test duration and peak oxygen consumption. In fact, given the peripheral limitations, it is unlikely that the subjects reach VO 2max ; we thus prefer to refer to VO 2 peak, as proposed by Kelly et al. . We decided not to measure the heart rate because the study population included five patients on betablockers.
1.2.4
Evaluation of autonomy in activities of daily living
Two scales were used to evaluate the change over time in the patients’ personal autonomy in ADL. We decided to use two reference ADL scales. The Barthel scale is widely used in the field of rehabilitation and has been shown to be relevant (notably in the management of hemiplegic patients ). The Katz ADL scale was also used.
Scoring of the Katz and Barthel scales was standardized and performed in random order. To avoid “therapist-dependent” effects, the information was collected by the same state-registered nurse in all cases.
The questionnaires were scored on programme entry and 4 weeks after the start of the rehabilitation.
1.2.5
The conventional rehabilitation protocol
All the patients received full hospital care from Monday to Friday, with 5 hours per day of rehabilitation. The standardized, multidisciplinary rehabilitation protocol combined physiotherapy, occupational therapy, speech therapy and neuropsychological therapy for 3 hours a day . The impact of daily nursing care (in term of rehabilitation and readaptation) should not be forgotten. The rehabilitation programme was mainly based on improving personal autonomy in ADL, with work focused on use of the legs: gait exercises, stance exercises, the treatment of orthopaedic disorders, balance work (with a view to subsequently withdrawing gait aids), use of support stockings and braces and maintenance of the freedom of movement of the proximal-distal limb joints. Learning to use a wheelchair and performing transfers were also priorities. For the arms, the application of compression strapping, prehension work and coordination exercises were combined with balance work in the sitting and standing positions. All the therapists were involved in rehabilitation of the higher functions (cognition, memory, etc.). The choice of the techniques used (e.g., Perfetti, Bobath, Kabat and other methods) was left to the therapists.
1.2.6
Adapted physical activities
APA programmes were personalized to suit each patient’s motor capacity and initial exercise results. General exercise training was implemented, with cardiorespiratory exercise (monitored by a heart rate monitor), muscle strengthening, gait exercises and work focused on executive functions. The APA lasted for between 40 and 60 minutes per day, four times a week. In order to develop the patients’ aerobic capacities, steady exercise on a semi-recumbent cycle ergometer (with both feet pedalling) was performed at between 70 and 80% of the maximum power (in W) achieved in the test. We ensured that the patient had already performed a warm-up session. Stretching-based physiotherapy sessions were often scheduled after the exercise training session, to aid the patient’s recovery. The aerobic programme was modified as a function to the tests performed throughout the rehabilitation care, according to the recommendations of Tailliar et al. .
To promote independent gait, we used a treadmill (with or without use of a technical aid, such as an ankle-foot orthosis) and a stepper.
Symmetric balancing stances and leg motor control were developed by using an isokinetic exercise machine (the Cybex Kinetron). For arm exercises, we used visual biofeedback. The shoulder girdle muscles, trunk muscles and main gait muscles were primarily exercised by using multiple, high-rep series (i.e. six series of 10 repetitions) of moderate intensity (i.e. between 50 and 60% of the force measured in three maximal, concentric-mode repetitions). Muscle strength tests on loaded machines were performed 2 weeks after the initial evaluation, in order to adjust the training loads. The load was incremented according to the improvement in the patient’s motor capacity, transfer ability and pain levels (as measured on a visual analogue scale, a numerical scale and a behavioural pain evaluation scale).
In order to improve the stroke patients’ psychological and physical status, games and group activities (such as balneotherapy and table tennis) were also scheduled, depending on each patient’s motor capacities. These activities stimulated and optimized motor control, executive functions and balance.
1.3
Statistical analyses
All statistical analyses were performed with SYSTAT 7.0 software. Means and standard deviations were calculated for all measured and calculated variables. For each parameter, a Shapiro-Francia normality test was performed. A two-tailed analysis of variance (ANOVA) for repeated measures was used to test for changes in the various parameters at T2. Correlations (MAP vs. Barthel and Katz scale scores) were tested with Spearman’s coefficient. The statistical significance threshold was set to P < 0.05.
1.4
Results
1.4.1
The study population
There were no statistically significant differences between the two study subgroups in terms of demographic and anthropometric data ( Table 1 ).
1.4.2
The exercise tests
Fig. 1 presents the test data collected at the end of the exercise programme. Significant improvements ( P < 0.05) in the peak oxygen consumption (+20%), MAP (+30%) and test duration (+30%) were observed for the trained group, whereas these parameters hardly changed in the control group ( VO 2 peak: +8%; MAP: +4%; duration: +1%). At T1, the two groups had identical results, whereas the results of the trained group were significantly better at T2.
1.4.3
The autonomy scores
After 4 weeks of early post-stroke APA training in our service, the trained patients had improved ( P < 0.05) their Barthel and Katz ADL scale scores by 37.04% and 22%, respectively ( Table 2 ). The ADL scores in the control group did not change significantly ( P = 0.07 for the Barthel scale score and P = 0.08 for the Katz scale score).
| Control group | Trained group | |
|---|---|---|
| Barthel scale score (T1) | 39.5 ± 16.2 | 42.5 ± 17.3 |
| Barthel scale score (T2) | 42.3 ± 17.4 | 67.5 ± 44.3 a |
| Katz scale score (T1) | 18.7 ± 3.2 | 17.6 ± 2.8 |
| Katz scale score (T2) | 17.8 ± 3.1 | 15.6 ± 3.4 a |
1.4.4
Relationship between the maximal aerobic power and autonomy
There was no apparent correlation between the Barthel and Katz ADL scores and the MAP ( Fig. 2 ).

1.5
Discussion
Our data show that it is feasible to perform a one-leg cycling exercise test in hemiplegic patients at 1 month post-stroke. Our results also revealed that conventional rehabilitation does not increase aerobic capacities.
1.5.1
Conventional rehabilitation
After 4 weeks of rehabilitation in the absence of specific exercise training, the physiological parameters hit a ceiling ( Fig. 2 ). It is difficult to compare our results with the literature because no other studies have looked at the repercussions of rehabilitation care on cardiovascular functions so soon after stroke and under real-life conditions. Existing experimental protocols do not take account of the particular condition of stroke patients. It appears that the various conventional techniques implemented over the 4 weeks of standard rehabilitation had little effect on the subjects’ reconditioning and do not favour readaptation to physical exercise. It is likely that the control group will go on to experience (primarily cardiac) deconditioning in the mid-term . This de-adaptation could be characterized by perturbation of venous return, together with an increase in blood viscosity and total peripheral resistance . These factors would lead to lower heart filling and a decrease in cardiac preload capacities. In future work, we intend to extend the protocol to a period of several months and perform cardiac ultrasound assessments to analyze this key parameter in deconditioning. We would also like to gather near infra-red spectrometry data and study peripheral adaptations.
Even though patients find walking with crutches difficult at first, we encourage therapists to try to implement gait exercises (with appropriate technical aids) as soon as possible. For example, walking with crutches results in much greater energy expenditure than normal gait does, as shown by Vezirian et al. . This means locomotion may constitute an excellent exercise for limiting physical deconditioning. Hickson et al. have suggested that to maintain the benefits of training, the exercise intensity must be around 70% of the VO 2 peak, with at least three sessions per week. Given our results and the characteristics of our population, we believe that it is essential to prescribe endurance exercises as soon as possible during the rehabilitation period. This is especially born out by the fact that the Barthel and Katz ADL scale scores did not change significantly in the control group – meaning that these patients did not gain any additional autonomy over the 4 weeks.
1.5.2
Early implementation of exercise training
After 4 weeks of exercise training, the trained group increased on its VO 2 peak value by an average of 20.33% (with an increase from 11.13 (± 4.60) to 19.44 (± 4.59) ml/min per kilogramme). An increase in MAP was also recorded (+31.25%). Our data are in agreement with the literature: Kelly et al. observed a VO 2 peak value of between 15.8 and 16.1 ml/min per kilogramme in hemiplegic patients evaluated 30 days post-stroke. The control group progressed only slightly; in our opinion, this corresponds to a spontaneous change over time in these patients . We suggest that an evaluation performed on the valid leg should be used as the starting point for a cardiovascular reconditioning programme based on one-leg cycling – even during the immediate post-stroke period of hemiplegic weakness. This evaluation would not only provide therapists with information on their patients’ physical condition but also screen for post-stroke cardiac risks. Even though our results are interesting and encouraging, they must be considered with a degree of caution because of the small number of subjects tested and the heterogeneity of this population. Although one-leg cycling certainly appears to be very well suited to this pathology, it is nevertheless an atypical type of exercise; at present, we lack data on the reproducibility of this type of effort.
In view of the observed improvements in cardiorespiratory parameters, early implementation of care does not appear to be risky and may enable patients to rapidly regain physical condition without having to first recover use of the affected limb. During the exercise tests, we noticed that peripheral (muscle-related) parameters restricted the test progression and thus led to underestimation of central (cardiac) parameters. The physiological response to exercise depends on the muscle groups used. Nevertheless, one-leg cycling appears to be a very appropriate type of exercise for evaluating stroke patients. It could even be prescribed in the first weeks of rehabilitation. Olivier et al. demonstrated that endurance exercise training with the healthy leg improves functional and ventilatory capacities and increases VO 2 peak. This improvement could be mainly due to muscle adaptations: an increase in the number and size of mitochondria, increased capillarization and better vasodilatation. Small, trained muscle masses may restrict central improvements . However, the latter work focused on orthopaedic pathologies, with relatively young, moderately deconditioned patients; we believe that exercise training with the healthy leg in stroke patients could lead to much more than muscle adaptation alone.
The patients’ training modes were chosen in order to enable compliance with the rehabilitation programme and avoid increasing any pain present, while enabling a gain in endurance capacity. However, the choice of the muscle contraction modes should be investigated in more detail.
Improved aerobic performance (even if it is a major public health and quality of life issue) only makes sense when it helps to improve the patient’s rehabilitation and reduce dependence. Our analysis of the Barthel and Katz scale scores revealed a major change in some ADL. The Barthel scale score rose significantly by 37%, with the mean value changing from 42.5 (± 17.32) to 67.50 (± 24.64) (with 100 corresponding to full autonomy). The scores on the Katz scale fell (T1: 17.6; T2: 15.6); it should be noted that this scale is scored out of a total of 24, with a minimum threshold of six corresponding to complete autonomy in ADL. We observed an increase in the patients’ degree of autonomy, notably in terms of movement, dressing and transfers. One can consider that after having been boosted physically and psychologically during the APA, the patient becomes more conscious of (and confident in) his/her motor capacities and is thus less apprehensive of trying to move. This stimulates the hemiplegic patient to become more independent in ADL. However, we did not observe a correlation between cardiorespiratory performance in the exercise tests on one hand and the Barthel or Katz ADL scores on the other ( Fig. 2 ). This absence could be explained by the fact that the scales take account of a large number of items (prehension, sphincter-related parameters, etc.), some of which are unrelated to cardiorespiratory data.
1.6
Conclusion
A one-leg cycling exercise test appears to be completely feasible in hemiplegic patients 1 month after stroke. This test could rapidly provide therapists with information on a patient’s cardiovascular status. Our results tend to show that the conventional rehabilitation cannot increase aerobic capacities as rapidly and as soon after stroke as an additional APA training programme.
Conflicts of interest statement
The authors have not declared any conflicts of interest.
2
Version française
2.1
Introduction
Troisième cause de mortalité après l’infarctus du myocarde et les cancers, les accidents vasculaires cérébraux (AVC) constituent la première cause de handicap acquis chez l’adulte . Au-delà de 60 ans, cette pathologie est la première cause de décès chez la femme et la seconde chez l’homme âgé. La fréquence, la gravité et le coût des AVC en font un problème de santé publique considérable. En 2002, l’Agence nationale d’accréditation et d’évaluation (Anaes) souligne l’importance du déconditionnement fonctionnel et cardiovasculaire chez des patients atteints d’un AVC. La gravité de cette désadaptation dépend de la localisation et de la taille de la lésion . Ramas et al. rapportent que les capacités d’effort du patient hémiplégique sont inférieures de 45 à 25 % comparativement à un sujet sain d’âge identique. La consommation maximale d’oxygène ( VO 2max ) diminue après un AVC pour atteindre en moyenne 10 à 20 ml/kg par minute. Sachant qu’il faut au moins 15 ml/kg par minute pour réaliser la plupart des activités de la vie quotidienne, l’enjeu d’une amélioration de la VO 2 lors de la rééducation devient alors primordial. Courbon et al. constatent chez des sujets hémiplégiques vasculaires une relation significative entre les performances maximales à l’effort et la capacité de marche. Un certain nombre d’études mettent en évidence l’importance d’un reconditionnement à l’effort . À la vue de ces constatations, il devient crucial que les établissements de santé proposent un reconditionnement musculaire et cardiovasculaire pour leurs patients. Pour lutter contre le déconditionnement et pour accélérer la récupération, les protocoles de rééducation des AVC préconisent certes un entraînement cardiorespiratoire mais il n’existe aucun consensus concernant le réentraînement au sens large.
En effet, de grandes disparités sont observées dans la littérature sur les intensités, la fréquence, les durées d’exercice et sur les moyens utilisés: tapis de marche, cycloergomètres . Il existe aussi une hétérogénéité sur les délais entre l’AVC et les débuts de programmes de réentraînement. Généralement, une longue période s’écoule (plus d’une année) entre l’accident initial et le réentraînement . Cette période nous paraît trop longue en regard des durées moyennes de séjour des patients hémiplégiques. En effet, l’essentiel des progrès et des enjeux de rééducation se font entre les trois et six premiers mois post-AVC , d’où l’intérêt d’une rééducation la plus précoce possible. Les conséquences neurologiques de l’hémiplégie et l’évolution favorable de la jambe lésée sont une limite à la fiabilité des tests proposés dans la littérature. C’est pour cette raison que la plupart des auteurs ne réalisent des évaluations cardiorespiratoires qu’à six mois de l’accident lorsque les aspects neurologiques sont stabilisés. Cependant, Tang et al. ont montré la faisabilité d’un test proche de l’AVC. La mise en place d’évaluation précoce sur tapis avec décharge a été aussi mise en avant par MacKay-Lyons et Makrides . En revanche, la mesure du VO 2 est difficile sur ce type de protocole. Pour palier à ce problème, l’évaluation pourrait être effectuée avec le membre inférieur valide, la faisabilité de cette approche a été démontrée chez des patients présentant des lésions orthopédiques . À notre connaissance, aucun protocole n’a évalué l’impact d’un programme de réentraînement à un mois de l’AVC à partir d’un pédalage unilatéral.
Ainsi, l’objectif principal de ce travail est de montrer que l’évaluation de l’aptitude aérobie chez des personnes hémiplégiques est possible précocement à partir d’un pédalage unilatéral. Notre étude analysera aussi les effets du reconditionnement à l’effort réalisé seulement quelques semaines après l’AVC.
2.2
Patients et méthodes
2.2.1
Population
Dix-huit patients hémiplégiques ont participé à cette étude. Les mesures anthropométriques des sujets sont présentées dans le Tableau 1 . Ces personnes ont été prises en charge à 20 ± 2 jours de l’AVC en hospitalisation complète. Les critères d’inclusion étaient les suivants: le sujet présente une hémiplégie droite ou gauche, suite à un AVC hémisphérique (ischémique ou hémorragique), le sujet a bénéficié d’un bilan étiologique complet (scanner et/ou IRM, holter ECG, Doppler, échographie cardiaque), le patient a un état clinique stable et bénéficie d’un traitement bien équilibré, en particulier antihypertenseur et anticoagulant. Les critères d’exclusion étaient les suivants: existence de troubles associés à l’atteinte motrice hémiplégique comme les troubles de compréhension et de mémoire, patient présentant une hémi-négligence, existence d’une affection intercurrente ou absence de stabilité de l’état lésionnel cérébral. Le protocole a été réalisé chez des sujets volontaires ayant eu une information sur les modalités du protocole et les procédures utilisées (consentement écrit et signé). Cette étude a reçu l’accord du comité médical de l’établissement sur le protocole expérimental et sur les considérations éthiques de l’étude.






