Dynamic stabilization of the spine has applications in cervical and lumbar degenerative disease and in thoracolumbar trauma. There is little evidence to support the use of dynamic cervical plates rather than rigid anterior cervical fixation. Evidence to support the use of dynamic constructs for fusion in the lumbar spine is also limited. Fusion rates, implant loosening, and failure are significant concerns that limit the adoption of current devices. This article provides a synopsis of the literature on human subjects. There is a need for high-quality evidence for interventions for spinal pathology. An evidence-based approach to the management of spinal disorders will require ongoing assessment of clinical outcomes and comparison of effectiveness between alternatives.
Arthrodesis of the spine is an important and useful technique for the management of spinal disorders including deformity, trauma, segmental instability, and symptomatic disc degeneration. Rigid stabilization of the spine with segmental fixation, fixed axis screws, and large diameter rods creates a mechanical environment that is associated with higher fusion rates than noninstrumented or semirigid constructs. However, rigid segmental fixation may have significant adverse effects including an increase in the stress on adjacent mobile segments, and stress shielding the bone graft material within the regenerate. Dynamic stabilization of a painful motion segment is an alternative to rigid internal fixation that may be useful in improving rates of fusion, or in providing an alternative approach to the surgical management of a painful motion segment without arthrodesis. Techniques of dynamic stabilization have been developed and evaluated for the treatment of degenerative conditions of the cervical and lumbar spine, and for thoracolumbar trauma and deformity. The purpose of this article is to review and assess the evidence in the literature on the efficacy of dynamic stabilization techniques in the management of spinal disorders.
Dynamic stabilization of the spine is a mechanical constraint of spinal motion that allows selective motion of the functional spinal unit. Dynamic stabilization in the cervical spine with a dynamic plating system is intended to limit motion to compression without translation. Selective compression may improve interbody healing and fusion mass formation. In the lumbar spine, posterior dynamic stabilization devices may provide segmental distraction without fusion, or may limit the motion of an unstable motion segment. When not used for fusion, these devices are designed to be load sharing with the spinal segment, selectively reducing translatory stresses and potentially modifying axial pain. Dynamic stabilization encompasses motion-sparing options for spinal instrumentation. Total disc arthroplasty devices have limited constraint in flexion, extension, and rotation compared with the normal motion segment. Rigid fixation of a motion segment causes changes in motion segment kinematics in the adjacent segments and increases in the area of center axis of rotation and intradiscal pressure. Less constrained motion-sparing options, including total disc arthroplasty in the cervical and lumbar spine, may reduce the effect of instrumentation on adjacent segments. The association of adjacent segment degeneration and disease with altered segmental kinematics remains controversial. The efficacy of restoring kinemetics of the adjacent segment with motion-sparing devices on reducing adjacent segment degeneration and pathology has yet to be reported in long-term follow-up.
This article is a systematic review of the evidence for dynamic stabilization devices used for cervical fusion and lumbar posterior dynamic stabilization for degenerative disease and trauma. Selection of devices for discussion was limited to dynamic stabilization options with published clinical outcome studies, and including objective patient-based health-related quality of life outcomes. All devices included have been approved by the US Food and Drug Administration (FDA) through 510k regulatory provision. The studies of lumbar and thoracolumbar posterior dynamic stabilization devices include physician-directed, or off-label uses of the devices without fusion. The quality of the evidence is graded using the technique of the Center for Evidence-based Medicine. The article is intended to provide the reader with an overview of published evidence of efficacy for dynamic stabilization devices in the cervical and lumbar spine.
Cervical spine
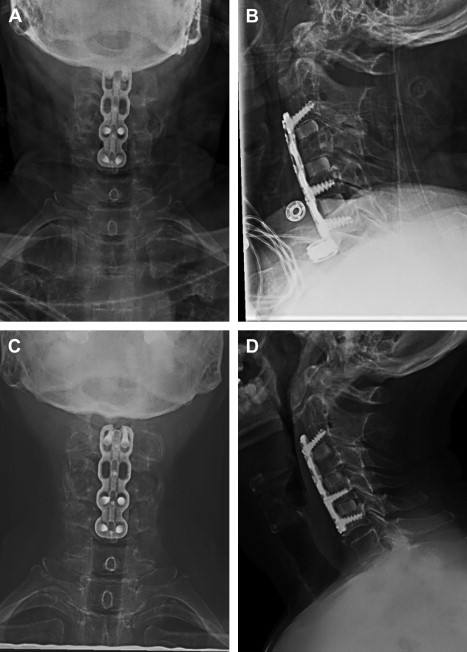
Anterior cervical plating is associated with decreased rates of graft dislodgement, kyphosis, and endplate fracture, and increased rates of fusion following multilevel anterior cervical discectomy and fusion. Rigid plating of multilevel constructs is believed to increase fusion rates by minimizing micromotion at the interbody spaces. With more than 2 treated levels, however, reported pseudarthrosis rates have been similar for instrumented and noninstrumented constructs. The rigid anterior cervical plate may prevent segmental subsidence, and loading of the interbody graft, allowing for gap formation and leading to nonunion. Dynamic cervical fusion plates are designed to compress the graft axially while preventing translation. There are 3 main types marketed and studied that are designed to load the interbody graft with variable axis of screws or axial compression capacity in the plate design. The first allows load sharing through screws that may toggle within the plate, allowing for compression through the graft. A second allows for graft compression through sliding screws within the plate, as the screw holes are oblong ( Fig. 1 ). A third design allows for rigid fixation through the screw holes, and allows for shortening of the plate itself through a telescoping design.
The biomechanical advantages of a dynamic cervical plate have been validated in basic scientific investigations. In a cadaveric C5 corpectomy model, Reidy and colleagues compared compressive forces borne by rigid and dynamic cervical plates. With optimally sized grafts, the rigid plate bore 23% of the load, versus 9% for the dynamic plate. The interbody graft handled 23% more force with the dynamic plate, which supports the intent of loading the interbody graft. With an undersized graft, a situation similar to graft subsidence or contact osteolysis, the dynamic plate allowed for more force transmission through the graft, although the greatest increases in forces were seen in the posterior elements. Brodke and colleagues, in a subsequent C5 corpectomy model, showed a significant increase in the load borne by the rigid plate with graft subsidence. In this model, graft subsidence did not affect the load-sharing properties of a dynamic cervical plate.
Clinical efficacy of dynamic cervical plates has been studied in several retrospective and prospective studies including prospective randomized controlled trials. Epstein reported on 42 patients undergoing single-level anterior cervical disc fusion (ACDF) with a dynamic plate. The results confirmed excellent fusion rates, and documented compression of the graft construct beneath the plate. However, the plate failure rate was 9.5%. Similar results were reported by Casha and Fehlings in their study of dynamic plating for cervical fusion. The cases reviewed were not limited to single-level ACDF, however, and included nearly equal numbers of single- and multilevel ACDF and single- and multilevel corpectomy. They reported an overall fusion rate of 93.8% at 2 years follow-up, with an implant complication rate of 8.2%. Implant failure correlated with an increasing length of construct. Radiographic measurements confirmed the dynamic properties of the plate.
Pitzen and colleagues presented level I data from a trial of 132 patients, comparing rigid with dynamic cervical plating for 1- and 2-level ACDF for degenerative disease or cervical trauma. The outcomes assessed were implant-related complication rates, time to radiographic fusion, loss of lordosis, and outcomes as assessed by the Visual Analog Scale (VAS) and the Neck Disability Index (NDI). The rigid plating group experienced a significantly higher rate of implant complications including plate loosening and screw breakage ( P = .045) The rigid plating group did have better preservation of cervical lordosis at 2 years follow-up ( P = .003). There were no significant differences in the clinical outcomes assessments. Because of the difference in complication rates, and despite the differences in cervical lordosis, the investigators concluded that dynamic plates are the preferable method of fixation for 1- and 2-level ACDF.
Nunley and colleagues performed a randomized controlled trial of a heterogeneous mix of patients undergoing single- or multilevel ACDF with rigid or dynamic fixation. They found no difference in outcomes for the groups undergoing single-level ACDF, but did find an advantage to dynamic instrumentation for multilevel ACDF. In contrast, DuBois and colleagues reviewed 52 patients undergoing 2- and 3-level ACDF, comparing rigid with dynamic anterior cervical plating. They found an increase in the rate of nonunion when using the dynamic cervical plate ( P = .05). They measured the amount of construct settling over 1 to 2 years, and found no difference between the plating systems, thus questioning the compressive properties of the plate in vivo. Clinical outcomes were similar among the groups, which led the investigators to conclude that the more expensive dynamic plates do not offer any clear benefit compared with rigid plates.
Anterior cervical plating is associated with adjacent-level ossification which may be due to impingement from the plate on the adjacent level disc space ( Fig. 2 ). Although comparative series have shown no difference in incidence of this complication when comparing rigid with dynamic cervical plating, special attention must be paid to technique when using a dynamic plate. Park and colleagues noted that the incidence of moderate to severe adjacent-level ossification was increased with less than 5 mm of space between the adjacent disc and plate. The implication for those using dynamic plates is that the subsidence of the bodies and graft must be accounted for at the time of surgery, as the plates may encroach on the adjacent levels in follow-up, as the graft is compressed. This problem requires the surgeon to know the amount of subsidence allowed by the plate, and to understand the method of dynamization to optimize plate and screw placement.







