Abstract
Purpose
Testing the new hip joint Helix 3D efficiency through clinical data and walking parameters.
Method
Three young hip-disarticulated patients (P1, P2 and P3) were assessed both with their previous prosthesis at first day, then four days and six months after being trained with a new prosthesis equipped with the Helix 3D hip joint. Assessments comprised a satisfaction questionnaire, a two-minute walk test and a recording of main spatiotemporal gait parameters
Results
After four days with the Helix 3D , the satisfaction for the prosthesis was improved for P1, unchanged for P2 and reduced for P3. Distance walked during two minutes increased for P1, unchanged for P2 and slightly improved for P3. Gait pattern was improved in P1, only. P1 abandoned the Helix 3D at six months due to an ischiatic wound. P2 and P3 chose not to use the Helix at the end of the four days training period because they could not adapt to the Helix 3D characteristics (hydraulic control of hip extension and assistance to hip flexion) and because they did not gain enough benefits. Despite much effort to adjust the prosthesis, the three patients definitively abandoned the Helix 3D because of comfort problems, and decided to walk with their previous prosthesis equipped with a monocentric hip joint or even with crutches only.
Conclusion
The Helix 3D hip joint may need further developments to get clinically relevant for hip-disarticulated amputees who may also need a long training period to adapt to its technical characteristics.
Résumé
Objectif
Tester l’efficacité de la nouvelle pièce de hanche Helix3D à l’aide de données cliniques et de paramètres de marche.
Méthode
Trois jeunes patients désarticulés de hanche (P1, P2 et P3) ont été évalués tout d’abord avec leur ancienne prothèse le premier jour, et ensuite à quatre jours et six mois après un entraînement avec leur nouvelle prothèse équipée de la pièce de hanche Helix3D. Les évaluations comprenaient un questionnaire de satisfaction, un test de marche de deux minutes et un enregistrement des principaux paramètres spatiotemporels de la marche.
Résultats
Après quatre jours d’entraînement avec l’Helix3D, le patient P1 rapportait une amélioration de la satisfaction vis-à-vis de sa prothèse, aucune amélioration n’était rapportée par le patient P2, et le patient P3 montrait une diminution de la satisfaction. La distance parcourue pendant deux minutes était augmentée pour le patient P1, ne montrait aucun changement pour P2 et était légèrement augmentée pour P3. Les paramètres de marche étaient améliorés pour le patient P1 uniquement. Ce même patient a abandonné l’Helix3D à six mois à cause d’une plaie ischiatique. Les patients P2 et P3 ont choisi de ne pas utiliser l’Helix3D à la fin des quatre jours d’entraînement car ils ne pouvaient s’adapter à ses caractéristiques (contrôle hydraulique de l’extension de hanche et assistance lors de la flexion de hanche) et n’en retiraient pas de bénéfices suffisants. Malgré leurs efforts pour s’adapter à cette prothèse, les trois patients ont abandonné définitivement l’Helix3D à cause de problèmes d’inconfort et ont décidé de reprendre leur prothèse précédente équipée d’une articulation monocentrique ou bien de se servir de béquilles.
Conclusion
La pièce de hanche articulée Helix3D et son protocole de mise en place semblent avoir besoin d’ajustements afin de se montrer cliniquement pertinents pour les patients désarticulés de hanche qui devront bénéficier d’une période d’entraînement plus longue pour s’adapter à ses caractéristiques techniques.
1
English version
1.1
Introduction
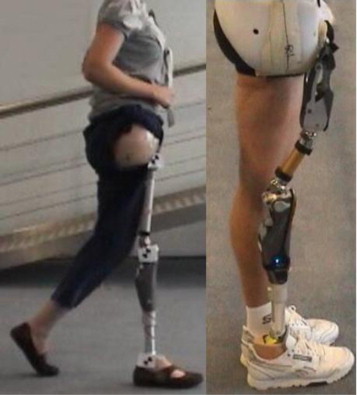
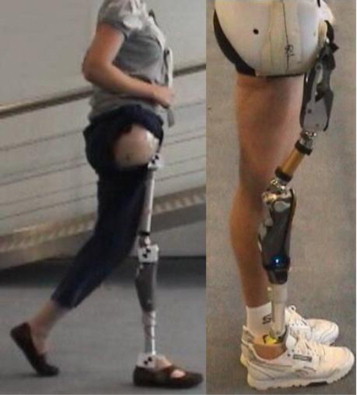
Although infrequent, hip disarticulation mainly concerns young, active, and demanding patients . Reducing their handicap by an appropriate prosthesis is a major challenge for rehabilitation medicine. For more than 50 years, prostheses for hip disarticulated amputees have been made of a hip joint behaving as a simple monocentric articulation 45 degree forwardly tilted as compared to a normal hip, that is, the Canadian prosthesis . Security of the stance phase on the prosthesis is allowed by a double recurvatum of hip and knee joints. Consequently, walking is possible with an artificial hip moving freely in one dimension, only (flexion-extension). This imposes body compensations such as leaning the trunk and performing a posterior tilt of the pelvis during the prosthesis swing phase . An innovation called Helix 3D (Ottobock ® ), consisting in a polycentric articulation, has been recently proposed ( Fig. 1 ). It is a four-bar-linkage polycentric joint with a hydraulic unit that provides controlled resistance to motion during both stance and swing phase . It allows an external rotation movement which facilitates the swing phase of gait, supposed to be similar to that of healthy subjects. Moreover, two flexible polyurethane springs help initiating the swing phase . A recent experimental study showed that the new hip joint Helix 3D can reduce gait abnormalities such as pelvic anteroposterior tilt .
The present observational study aimed to test efficiency of the new hip joint Helix 3D through clinical data and walk parameters.
1.2
Methods
Three hip-disarticulated patients (P1, P2 and P3) participated in this study. Patients were aware of the possible risks and informed consent was obtained. A Functional Independence Measure was realised for each patient at the inclusion. All patients were independent for daily life and their limitations concerned mostly gait and stairs climbing. All patients used previously a Canadian prosthesis with the same monocentric hip joint (7E7, OttoBock ® ). Only P1, who most of the time did not use his prosthesis needed a cane to walk with it. Detailed patients’ information is presented in Table 1 .
| Participants | P1 | P2 | P3 |
|---|---|---|---|
| Gender | Male | Male | Female |
| Age (years) | 33 | 41 | 37 |
| Height (cm) | 173 | 173 | 166 |
| Weight (kg) | 57 | 70 | 53 |
| Cause of hip-disarticulation | Trauma (work accident as elevator manufacturer) | Trauma (work accident as lumberjack) | Osteosarcoma of the femur |
| Side of hip disarticulation | Right | Right | Right |
| Time since the first prosthesis (year) | 1.8 | 4.5 | 24 |
| Rate of prosthesis utilisation | Very seldomly | Daily | Daily |
| Functional independence measure | 124/126 | 123/126 | 124/126 |
| Employment | No | Yes (carpenter) | Yes (biologist) |
| Previous prosthesis (hip, knee, and feet) | 7E7 3R15 1D10 | 7E7 C-Leg Variflex | 7E7 C-Leg 1C30 |
| New prosthesis (hip, knee, and feet) | Helix 3D C-Leg 1C40 | Helix 3D C-Leg Variflex | Helix 3D C-Leg 1C30 |
Patients were admitted for four consecutive days for training and adaptation of their novel apparatus with adjustments made several times a day by trained prosthetic technicians and physiotherapists. The sockets were made in polyethylene laminated, and embedded the whole pelvis with a moveable part fixed above the iliac crest on the non-amputated side. Socket conception for the Helix 3D was made by an experienced prosthetic technician trained to the characteristics of this new hip joint.
Training concerned mainly gait, stairs climbing, and adaptation to the characteristics of the Helix 3D . Assessments comprised a satisfaction questionnaire (SatPro) , a two minute walk test (2MWT) and a gait pattern assessment. The SatPro is an auto-questionnaire with 15 items estimating comfort, facility to use, and effectiveness of the prosthesis on a four points scale from 1 ‘completely agree’ to 4 ‘do not agree at all’. It provides a satisfaction score expressed in percentage ( Table 2 ). The 2MWT measures the maximal distance covered in two minutes at maximal gait speed on flat ground, indoor, and with usual shoes. The spatiotemporal parameters of gait were quantified using a GaitRite ® walkway . It consists of a 518 cm long walking carpet integrating pressure sensitive sensors. Patients walked 35 m in several sequences. The outcome parameters were: speed, single support time at prosthesis side, step time differential between prosthetic and sound limbs, step length differential between prosthetic and sound limbs, and step length for both sides. SatPro, 2MWT and gait pattern analysis were performed the first day (D1) with the monocentric hip (7E7, OttoBock ® ) and at the end of the four days adaptation session (D4) with the Helix 3D . A follow-up was performed, including a consultation at six months.
| Items | P1–D1 7E7 | P1–D4 Helix 3D | P2–D1 7E7 | P2–D4 Helix 3D | P3–D1 7E7 | P3–D4 Helix 3D |
|---|---|---|---|---|---|---|
| My prosthesis is comfortable | 3 | 2 | 4 | 2 | 1 | 3 |
| I feel comfortable with people other than my close relatives | 3 | 2 | 3 | 3 | 1 | 4 |
| My prosthesis is easy to clean | 2 | 2 | 1 | 1 | 2 | 3 |
| My prosthesis function properly whatever the temperature | 2 | 2 | 1 | 1 | 1 | 2 |
| My prosthesis is easy to put on | 3 | 2 | 1 | 1 | 1 | 3 |
| It is likely that my prosthesis will wound me | 3 | 3 | 1 | 3 | 3 | 1 |
| I feel it easy to move about with my prosthesis | 3 | 2 | 1 | 3 | 1 | 3 |
| Repairing/adjustment of my prosthesis don’t take too long | 2 | 1 | 1 | 2 | 3 | 2 |
| My prosthesis is going to last long | 3 | 1 | 1 | 2 | 2 | 1 |
| I can do more things when I wear my prosthesis, than when I don’t | 3 | 1 | 1 | 1 | 1 | 2 |
| I’m satisfied of the appearance of my prosthesis | 2 | 2 | 1 | 1 | 2 | NR |
| I understood easily how to use my prosthesis | 2 | 2 | 1 | 1 | 1 | 2 |
| I feel it easy to use a cane with my prosthesis | 3 | NR | 2 | 2 | NR | NR |
| My prosthesis causes me pain | 2 | 2 | 1 | 2 | 3 | 2 |
| Generally, I am satisfied of my prosthesis | 3 | 2 | 1 | 1 | 1 | 1 |
| Total score of satisfaction (%) | 47 | 71 | 73 | 75 | 79 | 50 |
1.3
Results
The satisfaction score increased from 47 to 71% with the Helix 3D hip joint for P1, from 73 to 75% for P2, and reduced from 79 to 50% for P3 ( Table 2 ). P2 and P3 found it more difficult to move with the Helix 3D than with the monocentric hip, whereas P1 expressed an opposite opinion. These opinions were consistent with the patients’ choice to return home with or without the Helix 3D . Furthermore, equipment with the Helix 3D allowed P1 to walk without crutches whereas he needed them with his previous prosthesis.
Changes in gait pattern are summarized in Table 3 . Distance at 2MWT was increased for P1 and P3 but unchanged for P2. P1 exhibited improved gait parameters whereas P2 and P3 exhibited a deterioration of their walking pattern after equipment with the Helix 3D as illustrated by a greater step length differential and shorter steps with the new prosthesis.
| Parameters | P1–D1 7E7 | P1–D4 Helix 3D | P2–D1 7E7 | P2–D4 Helix 3D | P3–D1 7E7 | P3–D4 Helix 3D |
|---|---|---|---|---|---|---|
| 2MWT (m) | 117 | 138 | 118 | 118 | 162 | 167 |
| Speed (cm/s) | 97.6 | 104.0 | 92.8 | 88.7 | 120.8 | 118.2 |
| Single support on the prosthesis (% stride time) | 30.8 | 34.2 | 31.5 | 32.0 | 32.7 | 31.8 |
| Step time differential (sec) | 0.14 | 0.09 | 0.15 | 0.14 | 0.02 | 0.04 |
| Prosthetic step length (cm) | 67.8 | 64.4 | 66.0 | 56.8 | 59.0 | 54.6 |
| Sound limb step length (cm) | 56.7 | 61.6 | 68.7 | 69.9 | 75.4 | 73.5 |
| Step length differential (cm) | 11.1 | 2.8 | 2.7 | 13.1 | 16.4 | 18.9 |
For P1, the follow-up at six months showed an ischiatic wound due to the socket system which imposed to stop using the prosthesis. Much effort was made to adjust the prosthesis but the patient rejected it, mainly because of comfort problems such as stump pain and difficulties to walk. He finally decided to come back to an ambulation with crutches and without prosthesis. P2 and P3 rejected the Helix 3D at the end of the four days training session. They came back to the use of their previous prosthesis with the monocentric hip joint. P2 reported more difficulties for climbing stairs and impossibility to accelerate gait at any moment due to the hydraulic control of hip extension. P2 also complained about the weight of the Helix 3D (1265 g vs. 875 g for the 7E7 hip joint). P3 reported difficulties and losses of balance when standing up due to the hydraulic resistance to hip extension. P2 and P3 also complained about the assistive springs as they experienced falls or hazardous situations due to unexpected flexion of the prosthetic hip.
1.4
Discussion
This was one of the first studies testing the clinical interest of the new hip joint Helix 3D for hip disarticulated amputees. Although it substantially improved gait parameters in one patient, after four days of training only, the prosthesis was abandoned by all three patients mainly because of comfort problems, and despite much effort was put to adjust the prosthesis strictly following the manufacturer protocol and recommendations.
P1 who obtained the greatest benefits with the Helix 3D was the patient who had his knee joint and prosthetic feet changed at the same time as the hip joint because Helix 3D have to be used with a C-Leg ® knee. Thus, the benefits observed for P1 may be partially due to the transition to a microprocessor controlled knee with hydraulics. Indeed, hip-disarticulated patients of our amputee unit often reported that equipment with a C-Leg ® knee provides an important benefit for walking and comfort. Since P1 had poor gait capabilities at day 1 it may be that he benefited more from the four days training session than the two other patients who already used their prosthesis in daily life.
The ischiatic wound reported by P1 at six months could be explained by the fact that his stump skin had never been adapted to bear weight in a prosthesis and was too sensitive to wear a Canadian prosthesis on a daily basis (4 hours/day with the new prosthesis). The final reasons for prosthesis rejection by P1 were consistent with those previously described in the literature, that is, pain, fatigue, and difficulty to use the prosthesis . Though using crutches only induced a greater energy cost than using a prosthesis , P1 finally chose to abandon his prosthesis.
The unexpected hip flexions experienced by P2 and P3 were a major concern in their decision to reject the Helix 3D because it questioned their ability to realise their professional activities.
A limit of this observational study is that four days may be too short to get used to a new prosthetic joint with hydraulic control and spring assisted flexion . Changes in gait pattern might have been positive for all patients after several weeks of daily ambulation and training with the Helix 3D hip joint .
The fact that the Helix 3D was rejected by the two more experienced patients emphasised the difficulty for disabled people to change their assistive device and adapt to a new one. More generally, this questions the brain plasticity and the possibility for patients to change their motor strategies during the rehabilitation process. In the present case, P2 and P3 had a professional activity which may explain that they could not wait to be used to the weight and technical characteristics of this new prosthetic component and chose to keep their previous prosthesis with a monocentric hip joint.
Finally, we hypothesised that the difficulties experienced by HDA were also due to the manufacturer protocol aiming at optimizing the Helix 3D mechanical properties. When following this protocol, patients were put in a difficult situation regarding balance because of a lower knee recurvatum than with the previous prosthesis. The prosthesis instability may have prevented the patients to become confident in the prosthesis and limited the possibility to use the technical characteristic of the Helix 3D .
Based on the difficulties experienced in the equipment of these three HDA patients, we suggest a different protocol to set up the Helix 3D . The prosthesis adjustments should be first directed toward patient’s balance confidence with the “classical” knee and hip recurvatum. Then, the prosthesis alignment could be slowly modified through training toward the optimal alignment recommended by the manufacturer while preserving the patient’s balance confidence.
1.5
Conclusion
This three cases study showed that experimental and clinical assessments and satisfaction scales must be associated for the validation of technical innovations in amputees . It also suggested the need for further developments of the Helix 3D equipment protocol before getting clinically relevant for hip-disarticulated amputees. A prolonged training period might be also necessary to improve confidence in the prosthesis equipped with Helix 3D , especially when equipping hip-disarticulated patients used to another prosthesis.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Bien que rare, la désarticulation de hanche concerne souvent des patients jeunes, actifs et exigeants . La compensation de leur handicap par une prothèse appropriée reste un challenge majeur pour la médecine de réadaptation. Depuis plus de 50 ans, les prothèses pour désarticulés de hanche, comme la prothèse Canadienne, comprennent une articulation de hanche se comportant comme une simple articulation monocentrique, inclinée de 45 degrés vers l’avant . La sécurité de la phase d’appui est assurée par un montage en double recurvatum de hanche et de genou. En conséquence, la marche est possible avec une hanche artificielle bougeant librement mais dans une dimension uniquement (flexion-extension). En revanche, le patient doit compenser en inclinant le tronc vers l’avant et en effectuant une bascule postérieure du bassin durant la phase pendulaire de la prothèse . Récemment, une nouvelle technologie, l’Helix3D (Ottobock ® ), est apparue sur le marché ( Fig. 1 ). Il s’agit d’une articulation polycentrique, montée sur quatre axes, composée d’une unité hydraulique qui fournit une résistance contrôlée au mouvement pendant la phase d’appui et la phase pendulaire . Ce système permet un mouvement de rotation externe facilitant la phase pendulaire de la marche, supposée être ainsi similaire à celle de sujets sains. De plus, deux ressorts flexibles en polyuréthane assistent l’initiation de la phase pendulaire . Une récente étude expérimentale montrait que l’Helix3D permettait une réduction des anomalies de marche telles que les bascules antéropostérieures du bassin .