Abstract
Adolescent idiopathic scoliosis (AIS) is a tridimensional deformity of the spinal column. This frequent disease, which has no clearly identified pathogenic mechanism, can have serious consequences. It has been hypothesized that unilateral and isolated vestibular disorders could be the origin of AIS. The objective of this work is to verify this hypothesis and to establish a pathophysiological model.
Method
We performed a Pubmed-NCBI search, for the period 1966–2013, crossing the keyword scoliosis with the following keywords: vestibular, labyrinthine, postural control.
Results
This search retrieved 66 articles. Twenty controlled studies were considered for study. Their analysis showed discordant results. This review cannot confirm a link between isolated vestibular disorder and occurrence of development of scoliosis.
Conclusions
There is not enough evidence to show a link between unilateral, isolated, vestibular dysfunction and AIS. From these findings, we propose a more global pathophysiological concept, which involves a trouble of the orthostatic postural control, with disturbance in the multisensory integration of vestibular, visual and somesthesic inputs. AIS could be the consequence of a reorientation of the longitudinal body axis in accordance with an erroneous central representation of verticality. An assessment of the sense of verticality would allow evaluate this hypothesis.
Résumé
La scoliose idiopathique de l’adolescent (SIA) est une déformation tridimensionnelle du rachis, fréquente, susceptible de conséquences graves, sans explication pathogénique claire. L’hypothèse d’une perturbation vestibulaire, unilatérale, isolée, à l’origine de la SIA a été proposée. L’objectif de ce travail est de vérifier cette hypothèse et d’en déduire un modèle physiopathologique.
Méthode
Nous avons effectué une recherche sur Pubmed-NCBI, sur la période 1966–2013, en croisant le mot clé scoliosis avec les mots clés : vestibular , labyrinthine , postural control .
Résultats
La recherche a permis de recueillir 66 articles. Vingt études contrôlées ont été retenues. Cette revue ne confirme pas de lien entre une atteinte vestibulaire unilatérale, isolée et l’apparition d’une scoliose.
Conclusions
Les preuves ne sont pas suffisantes pour établir un lien entre une atteinte vestibulaire isolée et l’apparition d’une SIA. À partir de ces résultats, nous proposons un modèle physiopathologique plus global faisant intervenir un trouble du contrôle postural orthostatique par perturbation de l’intégration centrale multisensorielle des différentes informations vestibulaires, visuelles, et somesthésiques. La SIA pourrait être la conséquence d’une réorientation de l’axe corporel longitudinal sur une représentation centrale erronée de la verticale. Une évaluation du sens de la verticalité permettrait d’explorer cette hypothèse.
1
English version
1.1
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional spinal deformity that affects 1–3% of the population aged 10–16 years. Female predominance is noted but no etiopathogenic mechanism has been identified. AIS is a progressive disease that can have serious consequences in adult life . Most authors consider AIS to be multifactorial, involving genetic, tissular, hormonal, biomechanical and neurosensorial factors . De Sèze et Cugy combine these factors into 4 distinct pathogenic categories : asymmetric bone growth deregulation (autonomic nervous system dysregulation, asymmetrical activity of neurocentral cartilages); susceptibility of bones to deformation (hormonal and hematologic phenomena regulating bone metabolism); abnormal passive spine maintenance systems with an impact on the skeleton structure (intervertebral disc collagen, elastic fibres of vertebral ligaments); disturbance to the active spine maintenance systems which modify muscle tone applied to the musculoskeletal spine architecture . Abnormalities of orthostatic postural control belong to this latter category . Due to their role in orthostatic postural control, several authors have suggested an involvement of different sensory modalities in the genesis of scoliosis: the vestibular system , the visual system , and somesthesia .
Concerning the visual modality, several studies show a high incidence of scoliosis in the visually impaired population: Catanzariti et al. found 5 times more incidents of scoliosis in these patients versus the control group; Grivas et al. found 42% of scoliotic deformities in blind women. Oculomotor abnormalities are described in some patients with AIS: more than 50% have an abnormal optokinetic nystagmus , other work concludes with abnormal saccadic eye movements .
Some authors found poorer somatosensory performance in SIA: in Kessen et al. study , the patients with AIS and right hand dominant, have a proprioceptive deficit in the upper limbs (assessed by the precision positioning of the fingers). Another study shows an increase in vibration thresholds of metatarsophalangeal joints, in patients with AIS .
Assessments by brain imaging in the AIS show abnormalities of the structures involved in the orthostatic postural control. For example, some parts of the vestibular cortex (such as the lateral sulcus) have a lower cortical thickness in AIS patients , on the other hand, the cerebellum has a larger volume in scoliotic subjects .
Among the sensory factors which may participate in the formation of a structural scoliosis, the vestibular system is certainly the most involved in studies . An unilateral and isolated vestibular dysfunction, would, through the vestibulo-spinal pathway, give rise to an asymmetric paraspinal muscle tone, which, during spinal growth, could lead to scoliosis .
Our purpose was to determine whether data in the literature confirms this hypothesis proposition and, from the results of this review, to propose SIA pathophysiological model.
1.2
Methods
We performed a Pubmed-NCBI search, for the period 1966–2013, crossing the keyword “scoliosis” with the following keywords: “vestibular”, “labyrinthine”, and “postural control”. We distinguished clinical studies and experimental animal studies. We retained four types of studies:
- •
controlled experimental animal studies evaluating the effect of destroying the vestibular structures on spinal posture;
- •
controlled clinical studies comparing standard clinical vestibular tests in adolescents aged 10–18 years with and without AIS. Two categories of tests were considered depending on the vestibular subsystem studied: semi-circular canal (SCC) or otolith systems. For the SCC system, we retained studies on stimulation and/or measuring the vestibulo-ocular reflex (VOR). For the otolith system, we retained studies using otolithic stimulation tests and/or measuring the subjective visual vertical (SVV). To be retained for analysis, clinical studies had to use at least one of the above-mentioned tests;
- •
controlled studies (AIS versus controls, age 10–18 years) investigating the imaging of the vestibular system;
- •
controlled studies evaluating the incidence of AIS in a population defined by a vestibular disorder.
1.3
Results
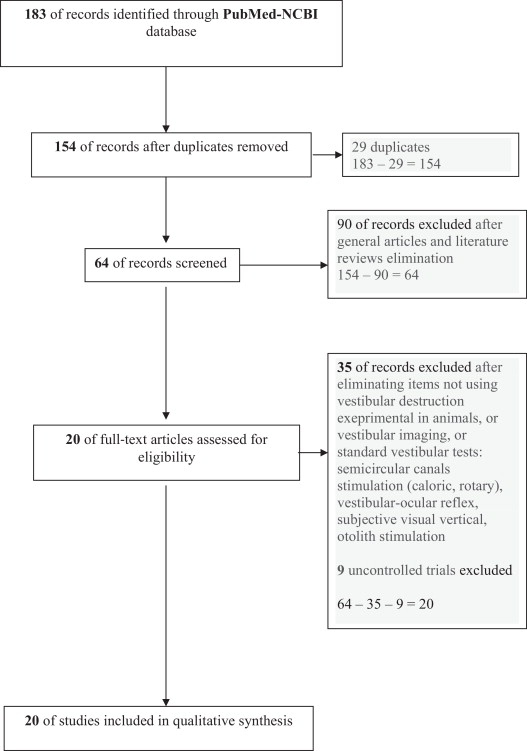
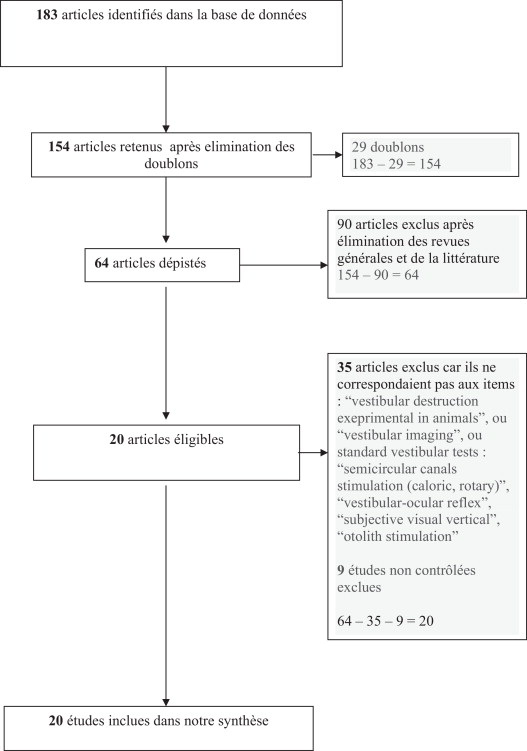
The results were: “vestibular and scoliosis” = 44 articles; “labyrinthine and scoliosis” = 26 articles; “postural control and scoliosis” = 113 articles. After eliminating duplicates, reviews of the literature, non-controlled studies, general articles, and studies not corresponding to the four categories defined in the protocol, we selected 20 controlled studies investigating the vestibular system in AIS ( Fig. 1 ):
- •
controlled experimental animal studies evaluating the effect of destroying the vestibular system on spinal posture (3 articles);
- •
controlled clinical studies in adolescents aged 10–18 years comparing standard clinical vestibular tests in groups with and without AIS (13 articles);
- •
controlled imaging studies of the vestibular system (AIS versus controls, age 10–18 years) (5 articles);
- •
controlled studies evaluating the incidence of AIS in a population with vestibular disease (1 article). Two articles belonged to two categories.
To facilitate the presentation, the results are listed by 5 categories as follows:
- •
experimental animal studies;
- •
SCC and AIS, with:
- ∘
SCC direct stimulation and AIS,
- ∘
and study of the VOR and AIS;
- ∘
- •
otolith system and AIS with:
- ∘
stimulation of the otolith system and AIS,
- ∘
and measurement and AIS;
- ∘
- •
vestibular system imaging and AIS;
- •
incidence of AIS in populations with vestibular disease.
1.3.1
Experimental animal studies
These studies examined the effect of destroying the vestibular structures on spinal balance. Three studies met the defined criteria ( Table 1 ). Unilateral destruction of the otolith system in animal models led to a contralateral effect with rotation of the thoracic vertebrae and head tilt that could lead to structural scoliosis . Nevertheless, this deformity was temporary, probably due to compensation of the antigravity muscle proprioception. Lambert et al. were able to create sustained structural scoliosis by unilateral destruction of the peripheral vestibular system in the guinea pig at different stages of neurological maturity . The deformity was characterized by tilt and rotation contralateral to the vestibular destruction that developed only when the stage of maturity corresponded to an absence of antigravity muscle proprioception. Otherwise, the scoliosis did not develop because muscle proprioception compensated for the vestibular destruction. Similarly, Barrios and Arrotegui showed that unilateral central destruction of the lateral vestibular nucleus led to the development of structural scoliosis in only 15% of cases (with no data on the side of the scoliosis) .
| Author | Population | Protocol | Results |
|---|---|---|---|
| De Waele et al., 1989 | Adult guinea pigs n = 4 | Selective unilateral destruction of the otolith system | Structural scoliosis with rotation ipsilateral to the vestibular destruction |
| De Waele et al., 1989 | Adult guinea pigs n = 4 | Selective unilateral destruction of the posterior semi-circular canals | No scoliosis |
| Barrios and Arrotegui, 1992 | Albino Wistar rats n = 13 | Selective destruction of the right vestibular nucleus | 2/13 structural scoliosis |
| Lambert et al., 2009 | Xenopus laevis frogs n = 19 | Unilateral vestibular destruction at different stages of maturity | Structural scoliosis contralateral to the vestibular destruction if destruction before maturity |
1.3.2
SCC and AIS
We distinguish two types of studies, those evaluating the effects of direct stimulation of the SCC, and those studying the VOR.
1.3.2.1
SCC direct stimulation in AIS
Five studies investigated stimulation of the horizontal SCC in patients with AIS ( Table 2 ). These studies compared AIS populations with matched non-AIS populations. The most commonly used endpoint was unilateral vestibular-stimulation-induced nystagmus. The goal was to detect unilateral involvement of the vestibular system. Four of the five studies used the caloric test . The fifth study used rotation to stimulate the vestibular system . Two studies failed to find any significant difference compared with the control population . The other studies demonstrated an impaired vestibular system in the AIS group: dysrhythmic post-stimulation nystagmus ; increased post-stimulation body oscillations ; asymmetrical vestibular involvement correlated with the side of scoliosis . The results were discordant: one study showed hypoexcitability of the horizontal SCC ipsilateral to the convexity of the scoliosis curvature , while another reported hyperexcitability of the horizontal SCC ipsilateral to the convexity of the scoliosis curvature . Two complementary studies showed that these anomalies were not correlated with the angle of the scoliosis, or with the progression of the scoliosis .
| Author | Population | Test | P | |
|---|---|---|---|---|
| AIS n ≥ 30/< 30 | Controls n ≥ 30/< 30 | |||
| Krodel et al., 1997 | < 30 | < 30 | Post-CVS ENG | NS |
| Kapetanos et al., 2002 | < 30 | < 30 | Post-CVS ENG | NS |
| Sahlstrand and Petruson, 1979 | ≥ 30 | ≥ 30 | Post-CVS ENG | < 0.05 |
| Sahlstrand et al., 1979 | ≥ 30 | ≥ 30 | Post-urography > CVS | < 0.05 |
| Jensen and Wilson, 1979 | < 30 | < 30 | ENG > RVS | < 0.01 |
1.3.2.2
Study of the VOR and AIS
The VOR stabilizes the image on the retina, allowing clear vision during head movements ( Table 3 ). Measuring the VOR evaluates SCC function . Among the three controlled studies exploring the VOR in AIS , only the study by Rousie et al. found VOR disorders in AIS patients presenting dysgenesia of the SCC .
| Author | Population | Test | P | |
|---|---|---|---|---|
| AIS n ≥ 30/ < 30 | Control n ≥ 30/< 30 | |||
| Rousie et al., 2009 | ≥ 30 | ≥ 30 | VOR | 0.05 |
| Simoneau et al., 2009 | < 30 | < 30 | VOR | NS |
| Lion et al., 2013 | ≥ 30 | ≥ 30 | VOR | NS |
1.3.3
Otolith system and AIS
Two types of studies were distinguished, those evaluating the effect of stimulating the otolith system and those studying the SVV.
1.3.3.1
Stimulation of the otolith system and AIS
Two studies investigated otolith function in AIS, mainly by recording vestibular evoked myogenic potentials ( Table 4 ). These otolith evoked potentials are recorded ipsilaterally to an acoustic stimulation. The otolithic stimulation with off-vertical axis rotation (OVAR) was also studied . These two studies showed involvement of the otolith system, especially on the right, in 67% of AIS patients , with no correlation with the Cobb angle, AIS progression, or side of the scoliosis convexity .
| Author | Population | Test | P | |
|---|---|---|---|---|
| AIS n ≥ 30/< 30 | Control n ≥ 30/< 30 | |||
| Wiener-Vacher and Mazda, 1998 | n = 30 | < 30 | OVAR | < 0.05 |
| Pollak et al., 2013 | < 30 | < 30 | VEMP | < 0.05 |
1.3.3.2
SVV measurement and AIS
The SVV is the estimation of the gravitational vertical by a subject ( Table 5 ). It is measured by the angle between the physical vertical gravity and the position of a linear reference, vertically adjusted by the investigator or the patient . His perception is the result of multimodal sensory integration (vestibular, visual and somatosensory) . Each sensory reference contributes, with a varying weight depending on the circumstances and pathologies .
| Author | Population | Test | P | |
|---|---|---|---|---|
| AIS n ≥ 30/< 30 | Controls n ≥ 30/< 30 | |||
| Krodel et al., 1997 | < 30 | < 30 | SVV | NS |
| Cheung et al., 2002 | ≥ 30 | ≥ 30 | SVV | NS |
| Cakrt et al., 2011 | < 30 | < 30 | SVV | < 0.01 |
The influence of vestibular cues on verticality perception has also been confirmed by several studies with galvanic and rotary vestibular stimulation . For example, among patients with unilateral peripheral vestibular dysfunction, without visual cue, the SVV is tilted towards the lesion side . The otolith’s sensitivity in the gravitational vector suggests that, within the vestibular complex, the role of the otolith system is important for estimating the SVV . But, according to the nature of its multisensory estimation, SVV is not a specific measure of the otolith system. Nevertheless, its disturbance seems to be a good indicator of an asymmetric otolithic performance .
Three studies investigated the SVV in AIS . Two of these studies found no significant difference between AIS and control populations .
1.3.4
Vestibular imaging and AIS
Four studies using 1.5 T magnetic resonance imaging (MRI) with 3D reconstruction using T2 sequence images of the internal ear revealed probably congenital dysgenesia of the superior and lateral SCC in AIS ( Table 6 ). Other anomalies were described but were not reported by all authors: abnormal connection between the lateral and posterior SCC ; difference between the left and right SCC . A fifth study evaluated the thickness of different cortical regions using 1.5 T MRI . This study showed a significant decrease in the thickness of the temporo-parietal junction near the lateral sulcus (or Sylvian fissure), a structure belonging to the “vestibular cortex” .
| Author | Population | Test | P | |
|---|---|---|---|---|
| AIS n ≥ 30/< 30 | Control n ≥ 30/< 30 | |||
| Rousie et al., 2009 | ≥ 30 | ≥ 30 | MRI of the SSC + 3D reconstruction | < 0.001 |
| Zeng et al., 2010 | < 30 | < 30 | MRI of the SSC + 3D reconstruction | < 0.05 |
| Xin et al., 2011 | < 30 | < 30 | MRI of the SSC + 3D reconstruction | < 0.05 |
| Shi et al., 2011 | < 30 | < 30 | MRI of the SSC + 3D reconstruction | < 0.05 |
| Wang et al., 2012 | ≥ 30 | Yes | Encephalic MRI + measure of cortex thickness | < 0.03 |
1.3.5
Incidence of AIS in a population of hearing impaired students
Vestibular disorders are observed in 30–86% of populations with congenital hearing impairment . Woods et al. found a lower incidence of AIS in a population of 3127 hearing impaired students (1.2%) compared with the general population (4–10%) .
1.4
Discussion
This literature review does not confirm our initial hypothesis. An unilateral, isolated, vestibular disorder, may not induce a structural scoliosis. In animal models, unilateral destruction of the vestibular system does not induce a permanent structural scoliosis, except in the presence of an associated defect of proprioceptive signal .
We noted the disparity of the reported results. One-third studies were “negative” (not in favour of vestibular origin in SIA), and the results of the “positive” studies (in favour of vestibular origin in SIA) were discordant. For example, studies evaluating the effect of stimulating the SCC in AIS produced contradictory results concerning the correlation between observed anomalies and the side of the spinal convexity . Among the three studies assessing the VOR, only one reported disorders in certain AIS patients presenting an abnormal connection between the lateral and posterior SCC . Imaging studies using MRI 3D reconstructions have reported a variety of SCC anomalies, dysgenesia of the superior and lateral SCC being the only constant feature .
Such variability compromises interpretation and might possibly suggest that SCC explorations may not be pertinent in AIS. Moreover, the potential impact of the spinal deformity on vestibular function cannot be ignored. Bruyneel et al. showed secondary disturbances of the postural system, adaptive to scoliosis, by postural and biomechanical reorganization, with compensatory dynamic posture of sitting and walking . For Gauchard et al., in patients with a single scoliosis major curvature spinal deformation induces abnormal cephalic position, leading to a vestibular asymmetry .
Studies of the otolith system are fewer. It is therefore difficult to draw general conclusions. The only two studies using otolith stimulation are in favor of a dysfunction in AIS populations compared to control groups . These reports were reinforced by MRI abnormality found in the lateral sulcus where otolith information is processed . This type of study should be nevertheless repeated particularly by recording vestibular evoked myogenic potentials . Conversely, studies exploring the SVV are not in favour of an asymmetry of the otolith system. Two out of three showed no difference, concerning SVV estimation, between scoliosis patients and controls . This may be due to recording conditions. It would be interesting to multiply them to change the available sensory information for assessing the vertical (standing on stable surface or foam, seated, supine, static or dynamic visual situation…) . It should also couple the SVV with an assessment of subjective postural vertical .
The epidemiological study of congenital hearing impairment showed a lower incidence of AIS versus general population . If the vestibular system is directly involved in the pathogenesis of AIS, one would have expected, in these patients who present between 30 and 86% of vestibular abnormalities, a higher incidence of the AIS. This result is also an argument against our initial hypothesis.
From this review, we do not believe that vestibular lesion, unilateral and isolated, without deficiency to the somatosensory system and/or the visual system, can induce permanent deformation of the human spine.
A disturbance in the multisensory integration and/or interaction, physiologically required for orthostatic postural control, seems more plausible. This possibility is supported by different authors who have shown, in patients with AIS, difficulties in orthostatic postural control, in cases of sensory conflicts . The central nervous system uses all sensory information available, according to the circumstances and current activity, to control body position relative to the earth-vertical . This sensory information is used to develop three referential. The egocentric referential, represented by the vertical axis Z body or longitudinal body axis, is provided primarily by somatosensory informations . The vertical Z axis, i.e. longitudinal body axis, is an imaginary line located at the intersection of the sagittal and frontal body planes, perpendicular to the transverse body plane. It connects the “just under the head” to the sole of the feet . The longitudinal body axis passes through the spinal axis and normally superimposes on the earth-vertical . The second, visual allocentric referential, situates the body in space and locates objects in the environment . The third, geocentric referential, fundamental invariant of posture, corresponds to the earth-vertical . It provides an absolute referential, independent of the position of the body or objects in space. These three references are normally concordant and allow the central nervous system to organize the orthostatic posture in reference to the earth-vertical . They allow the building of a sense of verticality, which is the ability to explicitly perceive the direction of the earth-vertical . The orthostatic posture is stabilized on the earth-vertical and allows body orientation in space, limb coordination, locomotion and the alignment of the longitudinal body axis on the vertical .
The redundancy of these three referential explains the possibilities of compensation in pathological situations, such as a unilateral vestibular deficit . Consequently, the deformation of the spinal axis, result of longitudinal body axis deviation, cannot be the result of a unilateral, isolated, vestibular deficit. To impact the longitudinal body axis, spatial referential must be biased, as described by Pérennou et al. in stroke patients . These authors describe errors for estimating SVV after hemispheric stroke . The patients align their orthostatic posture on an erroneous vertical reference. From these results, the existence of an internal model of sense of verticality has been suggested .
This internal model of verticality suggests the capacity to elaborate a mental representation of the earth-vertical from “bottom up” mechanisms by integrating the different multisensorial inputs coming from the vestibular (otolith), visual, and somesthesic systems, and from “top down” cognitive mechanisms . It is constructed progressively during childhood. It is based on sensorial and motor experiences of the body and its interactions with the environment .
This neurophysiological process can be applied to the etiopathogenesis of AIS, according to the following hypothesis: in AIS, the loss of concordance between central internal representation of verticality and earth-vertical would lead to a perturbation of longitudinal body axis, by impaired postural adjustment of the trunk, in the 3 planes of space, in relation to the earth-vertical . AIS would thus be the result of a reorientation of the longitudinal body axis, consequently of the spinal axis, in accordance with an erroneous central representation of verticality. Bruyneel has already showed that the scoliotic patient must organize and stabilize their balance from a disrupted spatial reference . This type of reorganization of the longitudinal body axis is also described in vestibular pathology and stroke .
This deformation of the longitudinal body axis persists because, during adolescence, multisensory interaction, supposed to compensate for this type of ambiguity, is limited. Indeed, adolescence is a period of transitional reorganization of certain postural strategies, in particular negligence of proprioceptive inputs and weaker performance of the vestibular system, preferring visual inputs? .
This disturbance of the sense of verticality might be determined genetically, possibly relating to immaturity of the central nervous system in the region of the vestibular cortex responsible for multisensorial integration and interaction, particularly the ventro-postero-lateral thalamus, the insula at the lateral sulcus and parietal cortex . These regions show a decrease in cortical thickness in patients with AIS .
This concept of cortical immaturity could explain the stabilization or even regression observed in certain cases of AIS subsequent to secondary maturation . The excess of osteopontin seen in AIS, due to defective melatonin signaling, could explain this immaturity . Osteopontin interferes in the differentiation and maturation of nerve fibers, in the cerebellum, brainstem, optic chiasm . It is expressed in trunk muscle spindles and contributes to the transfer of proprioceptive information to the central nervous system . So, osteopontin is concerned by various sensorineural structures of the internal representation of verticality.
Well-targeted complementary studies are necessary. Future work should couple a measure of the subjective postural vertical and the SVV under different conditions (standing with and without foam, sitting, supine, static vision or after optokinetic stimulation…), with an assessment of cognitive processes verticality .
1.5
Conclusion
This literature review cannot retain that unilateral and isolated vestibular lesion induces an AIS. In our etiopathogenic hypothesis, the AIS is secondary to an erroneous internal representation of verticality, causing a persistent tilt of the longitudinal body axis, with default of postural trunk adaptation on the earth-vertical, in a period of spinal growth and little possibility of sensory compensation. Well-targeted complementary investigations are needed to confirm this hypothesis. If confirmed, it would establish new rehabilitation protocols.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgments
For her help in the translation of this work, we thank Pamela Deegan, Vice-Consul in the Consular Services of the British Embassy in Paris, British Empire Medal in the 2014 New Years Honours. The authors are grateful to the HARPS Association members their helpful comments.
2
Version française
2.1
Introduction
La scoliose idiopathique de l’adolescent (SIA) est une déformation tridimensionnelle du rachis, avec une prévalence = 1 à 3 % entre 10 et 16 ans, potentiellement évolutive, prédominant chez la fille et d’étiologie inconnue, susceptible de conséquences néfastes à l’âge adulte . Il est classiquement admis une origine polyfactorielle, avec participation de facteurs génétiques, tissulaires, hormonaux, biomécaniques et neurosensoriels . De Sèze et Cugy regroupent ces différents facteurs en 4 catégories pathogéniques distinctes : dysrégulation asymétrique de la croissance osseuse (dysrégulation du système nerveux autonome, asymétrie d’activité des cartilages neurocentraux); susceptibilité osseuse à la déformation (phénomènes hormonaux et hématologique régulant le métabolisme osseux) ; anomalies des systèmes de maintien passif qui agissent sur le squelette (le collagène du disque intervertébral, le tissu conjonctif des fibres élastiques des ligaments vertébraux) ; perturbations des systèmes de maintien actif qui modifient le tonus musculaire appliqué sur l’architecture ostéoarticulaire du rachis . Les anomalies du contrôle postural orthostatique entrent dans cette dernière catégorie . En raison de leur rôle dans le contrôle et le maintien de la posture orthostatique, plusieurs auteurs ont suggéré une participation des différentes modalités sensorielles dans la genèse de la scoliose : le système vestibulaire , l’appareil visuel , et la somesthésie .
Concernant la modalité visuelle, plusieurs travaux montrent une incidence élevée de scolioses dans la population des déficients visuels : Catanzariti et al. dépistent 5 fois plus de scolioses chez ces patients en comparaison avec une population témoin, Grivas et al. trouvent 42 % de déformations scoliotiques en cas de déficience visuelle. Des anomalies oculomotrices sont décrites chez certains patients porteurs d’une SIA : plus de 50 % présentent une perturbation du nystagmus otpocinétique , un autre travail conclut à des anomalies des saccades oculaires .
Des auteurs trouvent de moins bonnes performances somesthésiques dans la SIA : dans l’étude de Keessen et al. , les patients, droitiers manuels avec une SIA, présentent un déficit proprioceptif des membres supérieurs (évaluée par la précision de positionnement des doigts). Une autre étude met en évidence une augmentation des seuils vibratoires des articulations métatarso-phalangiennes chez les patients porteurs d’une SIA .
Des évaluations par imagerie cérébrale dans la SIA montrent des anomalies de structures impliquées dans le contrôle postural orthostatique. Par exemple, certaines régions du cortex vestibulaire (comme la scissure de Sylvius ou sillon latéral) présentent une moindre épaisseur corticale chez les patients SIA , le cervelet à l’inverse présente un volume plus important chez les sujets scoliotiques .
Parmi les facteurs sensoriels qui pourraient participer à la constitution d’une scoliose structurale, le système vestibulaire est certainement celui qui a été mis le plus en cause . Une atteinte vestibulaire, unilatérale, isolée, induirait, via les faisceaux vestibulo-spinaux, une asymétrie du tonus de la musculature paravertébrale, qui, en période de croissance vertébrale, pourrait aboutir à une déformation scoliotique .
Notre objectif est de vérifier si la littérature permet de confirmer cette hypothèse, et à partir des résultats de cette revue, de proposer un modèle étiopathogénique de la SIA.
2.2
Méthode
Une recherche par Pubmed-NCBI, de 1966 à 2013, a été réalisée, en croisant le mot-clé scoliosis (scoliose) avec les mots-clés suivants : vestibular (vestibulaire), labyrinthine (labyrinthique), et postural control (contrôle postural). Pour retenir les études, nous distinguons celles chez l’homme et les études expérimentales chez l’animal. Nous retenons 4 types d’études :
- •
études contrôlées, expérimentales, chez l’animal, évaluant les conséquences, sur la statique rachidienne, de la destruction de structures vestibulaires ;
- •
études contrôlées chez l’homme, SIA versus témoins, âgés de 10 à 18 ans, évaluant des bilans vestibulaires standard. Les examens sont classés en fonction des 2 sous-systèmes vestibulaires étudiés : les canaux semi-circulaires (CSC) ou le système otolithique. Pour l’évaluation des CSC, nous avons retenu les études avec stimulation directe des CSC et l’étude du réflexe vestibulo-oculaire (RVO). Pour le système otolithique, nous avons conservé les études avec stimulation otolithique et/ou avec mesure de la verticale visuelle subjective (VVS). Les études doivent évaluer au moins un des examen sus-cités ;
- •
études contrôlées, SIA versus témoins, âgés de 10 à 18 ans, évaluant l’imagerie du système vestibulaire ;
- •
études contrôlées évaluant l’incidence des SIA dans une population présentant une pathologie vestibulaire.
2.3
Résultats
Les résultat sont les suivants : vestibular and scoliosis = 44 articles ; labyrinthine and scoliosis = 26 articles ; postural control and scoliosis = 113 articles. Après élimination des doublons, des revues de la littératures, des études non contrôlées, des articles généraux, des travaux ne correspondant pas à une des 4 catégories définies dans le protocole, nous avons sélectionnés 20 études contrôlées évaluant le système vestibulaire dans la SIA ( Fig. 1 ) :
- •
études contrôlées, expérimentales, chez l’animal, évaluant les conséquences, sur la statique rachidienne, de la destruction de structures vestibulaires (3 articles) ;
- •
études contrôlées chez l’homme, SIA versus témoins, âgés de 10 à 18 ans, évaluant des bilans vestibulaires standard (12 articles) ;
- •
études contrôlées, SIA versus témoins, âgés de 10 à 18 ans, évaluant l’imagerie du système vestibulaire (5 articles) ;
- •
études contrôlées évaluant l’incidence des SIA dans une population présentant une pathologie vestibulaire (1 article). Un article appartient à 2 catégories.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







