Disorders of the Scapula: Winging and Snapping
Ben W. Kibler
Aaron D. Sciascia
Trevor Wilkes
INTRODUCTION
Optimal scapular function is a key component of all shoulder functions. The scapula plays many roles in shoulder function. Anatomically, it is the “G” of the glenohumeral (G-H) joint and the “A” of the acromioclavicular (A-C) joint. Physiologically, it is the “S” of scapulohumeral rhythm (SHR), the coupled and coordinated movement between the scapula and arm that allows the arm to be placed in the optimum position and motion to accomplish tasks. Biomechanically, it provides a stable base for muscle activation, a moving platform to maintain ball and socket kinematics, and an efficient link between the core, which develops force, and the arm, which delivers the force. Critical to these roles is normal scapular motion.
Since the scapula plays such key roles, it is not surprising that alterations in these roles are associated with altered motion and are frequently discovered in association with all types of shoulder pathology. These alterations may be a cause or an effect of the shoulder pathology, but they do play roles in maintaining and/or exacerbating the functional consequences of the shoulder pathology. As a result, clinicians evaluating and treating shoulder pathology should include evaluation and treatment of the scapula and scapular motion in their treatment of shoulder pathology. Frequently, knowledge regarding scapular motion and position can provide key information about treatment options and can guide rehabilitation and return to activity decisions.
This chapter addresses pertinent aspects of anatomy and biomechanics of the scapula, scapular roles in normal scapular function, scapular motion, scapular dyskinesis, the clinical examination for and treatment of scapular dyskinesis, and describes clinical presentation and treatment guidelines for primary problems of the scapula and scapular involvement in other shoulder pathology.
SCAPULA ANATOMY
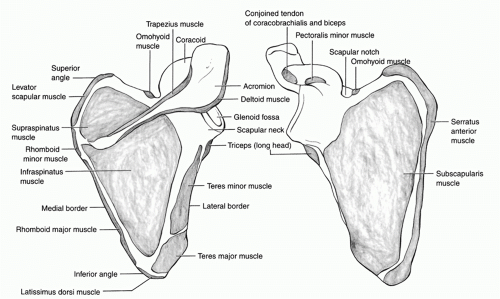
A thorough understanding of osteology and the muscular attachments of the scapula is required to grasp the complex movement patterns and function. The anatomy is predicated
on the developmental advantages of mobility, such as prehension and overhead use. This is reflected in several primary changes noted through time in the hominid scapula. First, the acromion has broadened and lateralized to allow mechanical advantage for the deltoid muscle. The coracoid has enlarged in a manner theorized to assist in the prevention of anterior dislocation at 90 degrees of abduction. Finally, broadening and alteration in the force vector of the infraspinatus and teres minor are postulated to increase both external rotation strength and humeral head depression.
on the developmental advantages of mobility, such as prehension and overhead use. This is reflected in several primary changes noted through time in the hominid scapula. First, the acromion has broadened and lateralized to allow mechanical advantage for the deltoid muscle. The coracoid has enlarged in a manner theorized to assist in the prevention of anterior dislocation at 90 degrees of abduction. Finally, broadening and alteration in the force vector of the infraspinatus and teres minor are postulated to increase both external rotation strength and humeral head depression.
The scapula is a large flat bone which forms from a collection of mesenchymal cells (Fig. 31-1). It shows signs of ossification by the fifth week of embryologic development. The scapula follows a predictable course in descending from the paracervical region to the thorax. Failure of this process leads to Sprengel’s deformity. By the seventh week the scapula has descended to its final position and the glenoid is easily identified.
The scapula is primarily formed through intramembranous ossification. The body and spine are ossified at birth and subsequently follow an expected pattern. However, there are several notable exceptions with clinical implications. The coracoid forms from two centers of ossification and is generally united by age 15. Rarely, a third ossification center at the tip can persist and present confusion with a fracture. The glenoid also forms from two separate ossification centers; one at the base of the coracoid and another with a horseshoe contour inferiorly. These are usually fused by 15 years of age as well. Finally, Os Acromiale may be noted in up to 8% of the population and is the result of two or three ossification centers which arise in puberty and fail to unite by the expected age of 22. The variable failures of fusion may result in the following abnormalities, from anterior to posterior: pre-acromion, meso-acromion (most common), meta-acromion, and basi-acromion.
Grossly, the scapula is a thin sheet of bone which serves as a critical site of muscle attachment. The blood supply is primarily through a network of periosteal vessels which take origin from muscular insertions. Thickening of the bone is notable at the lateral border, and at superior and inferior angles. Ventral concavity creates a smooth articulating surface against the ribs. Small oblique ridges exist ventrally for the tendinous insertions of the subscapularis. Similarly, small fibrous septa are present dorsally to attach and separate the infraspinatus, teres minor, and teres major. The dorsal surface is traversed by the scapular spine which divides two concavities; the supraspinatus and infraspinatus fossas. The medial two-thirds of these fossas give rise to the supraspinatus and infraspinatus muscles. The spine contains two important notches. The suprascapular notch at the base of the coracoid contains the suprascapular nerve and compression at this location will affect both the supraspinatus and infraspinatus muscles. Second, the spinoglenoid notch is present at the lateral border of the spine. Various causes can lead to compression of the suprascapular nerve here as well, producing isolated atrophy of the infraspinatus.
Anatomic interest in the scapula is frequently directed at the coracoid, acromion, or glenoid. The name coracoid derives from the Greek word korakodes meaning “like a crow’s beak.” The
bent shape resembles a finger pointed toward the glenoid. From the Greek word “akros” for point, the acromion is often referred to as the point of the shoulder. The morphology of the acromion is among the most studied in the body. Considerable cadaveric research has been directed at the relative frequency and postulated causes of the Types 1 through 3 acromion, as described by Bigliani.8 However, the relationship between acromial shape and “impingement syndrome” or rotator cuff tear has not borne out in the literature. Similarly, the glenoid has been the subject of intensive study in an effort to define bony anatomy in shoulder instability. Average values for size include a height of 35 mm and width of 25 mm, but considerable variability exists. Comparison to the contralateral side may be required to precisely define bone loss. Glenoid version may also range widely. Retroversion, up to 6 degrees is most common, as seen in 75% of the population, but anteversion up to 2 degrees is reported.
bent shape resembles a finger pointed toward the glenoid. From the Greek word “akros” for point, the acromion is often referred to as the point of the shoulder. The morphology of the acromion is among the most studied in the body. Considerable cadaveric research has been directed at the relative frequency and postulated causes of the Types 1 through 3 acromion, as described by Bigliani.8 However, the relationship between acromial shape and “impingement syndrome” or rotator cuff tear has not borne out in the literature. Similarly, the glenoid has been the subject of intensive study in an effort to define bony anatomy in shoulder instability. Average values for size include a height of 35 mm and width of 25 mm, but considerable variability exists. Comparison to the contralateral side may be required to precisely define bone loss. Glenoid version may also range widely. Retroversion, up to 6 degrees is most common, as seen in 75% of the population, but anteversion up to 2 degrees is reported.
The function of the scapula is dependent on the complex recruitment patterns of the 18 muscular attachments. These muscles can generally be categorized as axioscapular, scapulohumeral, and muscles of the upper arm (coracobrachialis, biceps brachii, and triceps brachii).
The axioscapular muscles serve to anchor the scapula for its role as the foundation of the shoulder. In addition, they guide the scapula through the requisite degrees of freedom. These muscles include the serratus anterior, levator scapula, pectoralis minor, rhomboids, and trapezius. The trapezius is the largest and most superficial axioscapular muscle. The expansive muscle originates from the occiput, nuchal ligament, and spinous processes of C7 through T12. The upper trapezius inserts across the distal third of the clavicle and acromion. The middle trapezius inserts across the scapular spine and the lower portion at the base of the spine. The broad muscle allows complex function in scapular retraction, elevation, and posterior tilting based upon the recruitment pattern. Frequently, the upper and lower trapezius are activated separately. Motor innervation is through cranial nerve XI, the spinal accessory nerve.
The rhomboids are divided into the major and minor portions. The rhomboid minor originates from the spinous processes of C7 and T1 and inserts at the medial scapular border at the base of the spine. The rhomboid major begins from T2 through T5 and insets along the posterior aspect of the medial border from the base of the spine caudally to the inferior angle. This orientation allows an important role in scapular retraction. The dorsal scapular nerve (C5) provides innervation. The serratus anterior comprises three divisions taking origin from the anterolateral aspect of the first through ninth ribs. Innervation of the serratus is provided by the long thoracic nerve. The serratus produces protraction and upward rotation of the scapula with arm elevation while providing a critical stabilization function against excessive internal rotation throughout nearly all positions of arm forward flexion and elevation. The levator scapula is intimately associated with the serratus and serves a role to elevate and upwardly rotate the scapula. The levator originates from the transverse processes of C1 through C3, and at times C4. Insertion is found upon the superior angle. Innervation comes from the deep branches of C3 and 4. The pectoralis minor is often overlooked in its role in scapular position. The muscle originates from the second through fifth ribs and courses superolaterally to insert upon the coracoid. Chronic tightness can contribute to protracted, anteriorly tilted scapular positioning.
The scapulohumeral muscles produce G-H motion and are composed of the deltoid, supraspinatus, infraspinatus, subscapularis, teres minor, and teres major. The deltoid originates broadly across the acromion and scapular spine while inserting on the deltoid tubercle of the humerus. This structure allows it to power elevation in multiple planes. As previously noted the supraspinatus and infraspinatus originate from the medial two-thirds of their respective fossas while inserting in a complex arrangement on the greater tuberosity. The subscapularis originates from the anterior aspect of the scapula and attaches on the lesser tuberosity. The teres minor takes origin from the middle section of the lateral scapula and is innervated by the posterior branch of the axillary nerve. The teres major emerges from a more inferior position on the lateral scapula and shares a common tendinous insertion with the latissimus dorsi on the medial aspect of the bicipital groove. It shares innervation from the subscapular nerve and functions in internal rotation, adduction, and extension of the humerus.
Two major bursa exist persistently around the scapula. The infraserratus bursa resides between the serratus anterior and the chest wall. The supraserratus bursa occupies space between the subscapularis and serratus anterior. In addition, several minor bursa may be present at the superomedial border, the inferior angle, or the medial base of the spine. Bursa may become persistently inflamed through overuse and subtle abnormalities in mechanics.
Biomechanics of Normal Scapular Motions
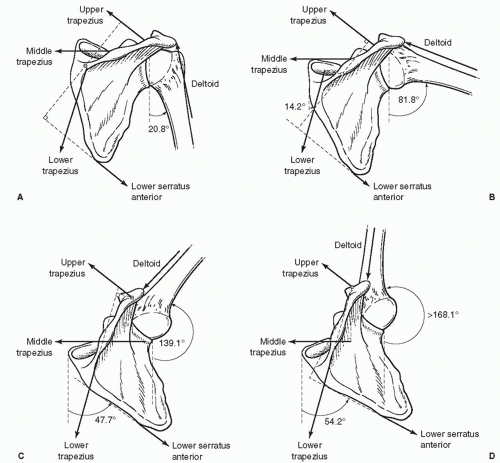
Scapular motion has traditionally been described in a single planar two-dimensional model, with scapular upward rotation and acromial elevation as the end point (Fig. 31-2).3,45 Upper trapezius activation to pull the acromion up and serratus anterior activation to move the inferior border laterally were described as the key muscle force couples.3,4,111 The magnitude of the upward rotation varied between studies but averaged 60 degrees, establishing the 1:2 scapula/humerus motion ratio for total scapulohumeral rhythm (SHR).
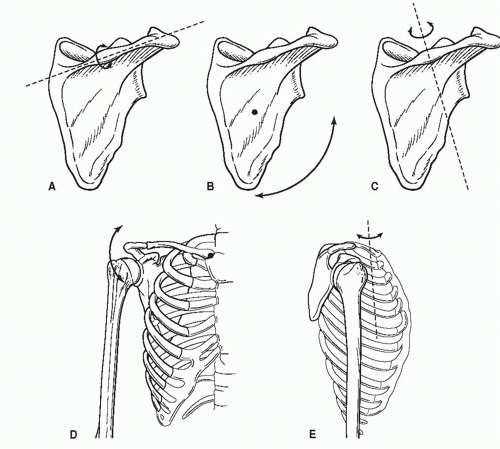
Recent studies show that scapular motion is actually multiplanar and three-dimensional. This work, using motion tracking systems and indwelling bone pins,71,73,76,80,117 demonstrates that total scapular movement is a composite of motions (rotations around axes) and translations (sliding along a surface).
The three observable rotary motions are upward/downward rotation around an axis perpendicular to the scapular body, internal/external rotation around a vertical axis along the medial border, and anterior/posterior tilt around a horizontal axis along the scapular spine (Fig. 31-3). The absolute amount of each rotation varies within the studies. The indwelling bone pin study by Ludewig is probably the most accurate.73 It shows that the resting position, in relation to the thorax, is 5.4 degrees of upward rotation, 41.1 degrees of internal rotation, and 13.5 degrees of anterior tilt. As the arm moves to maximum elevation, the scapula moves in all three motions. It upwardly rotates 45 degrees, posteriorly tilts 21 degrees, and moves into internal and then external rotation with a net change toward external rotation of 2 degrees.74 The largest part of these motions occurs in arm elevations above 80 degrees.
Two translations can occur in the presence of an intact clavicular strut and A-C joint. They are upward/downward sliding on the thorax due to clavicular upward/downward motion
at the sternoclavicular (SC) joint and anterior/posterior sliding around the curvature of the thorax due to clavicular anterior/posterior motion at the SC joint.
at the sternoclavicular (SC) joint and anterior/posterior sliding around the curvature of the thorax due to clavicular anterior/posterior motion at the SC joint.
The clavicle and the S-C and A-C joints are major factors in creating the scapular positions, motions, and translations. The clavicle is the only bony connection of the scapula to the axial skeleton. To maximize scapular movement and scapulohumeral motion during maximal arm elevation, the clavicle retracts 16 degrees, elevates 6 degrees, and posteriorly rotates on its long axis 31 degrees.74 All these motions are based on the S-C joint. A-C joint motions resulting from acromial motion on the clavicle demonstrated 8 degrees of internal rotation, 11 degrees of upward rotation, and 19 degrees of posterior tilting.74 These constrained motions create a reproducible screw axis of motion between the clavicle and scapula through the A-C joint and allows the three-dimensional motions.104
Because of the relatively limited bony attachment, the scapula is mainly dependent upon muscle activation for mobility and stability. The only connections of the entire medial scapular border to the axial skeleton are muscular. This allows a great amount of mobility and accommodation to many demands for different arm positions, but also creates large demands for eccentric muscle activation to withstand high distraction loads in activities involving forward arm motions or withstanding loading in the arm. Multiple periscapular muscles are activated to maintain this stability and activate the mobility.
Most research reveals that the upper and lower trapezius muscles, which are usually activated independently, and the
serratus anterior muscle, contribute the most to scapular stability and mobility.3,52,111 The upper trapezius acts on the acromion and upper lateral border of the scapular spine, and the serratus anterior acts on the inferior medial border. Coupling of activation of these two muscles initiates upward rotation and posterior tilt.111 This force couple is especially active at the beginning of arm elevation3 and with arm elevation below 90 degrees. As the arm elevation exceeds 90 degrees the lower trapezius is precisely positioned to increase and maintain upward rotation through a direct line of pull.3,74 In this arm position, the serratus anterior works to stabilize the medial border against the thorax, acting as a scapular external rotator. Lower trapezius activation is also important in the descent from maximum elevation, being activated eccentrically to control excessive anterior tilt. Other intrinsic muscles, the rhomboids and pectoralis minor, play important but not primary roles. The rhomboids are important muscles to initiate and maintain external scapular rotation in arm elevation and to control against excessive internal scapular rotation in arm descent. The pectoralis minor assists the serratus anterior as a scapular protractor in pushing activities but frequently becomes tight and shortened. Extrinsic muscles, mainly the latissimus dorsi and pectoralis major, create scapular motion through their effect as prime movers of the arm. Humeral motion also can create scapular motion by tension on the GH capsule and muscles, especially when glenohumeral internal rotation deficit (GIRD) is present. Finally, the scalenes and sternocleidomastoid muscles may affect scapular position due to their effect on clavicle motion.
serratus anterior muscle, contribute the most to scapular stability and mobility.3,52,111 The upper trapezius acts on the acromion and upper lateral border of the scapular spine, and the serratus anterior acts on the inferior medial border. Coupling of activation of these two muscles initiates upward rotation and posterior tilt.111 This force couple is especially active at the beginning of arm elevation3 and with arm elevation below 90 degrees. As the arm elevation exceeds 90 degrees the lower trapezius is precisely positioned to increase and maintain upward rotation through a direct line of pull.3,74 In this arm position, the serratus anterior works to stabilize the medial border against the thorax, acting as a scapular external rotator. Lower trapezius activation is also important in the descent from maximum elevation, being activated eccentrically to control excessive anterior tilt. Other intrinsic muscles, the rhomboids and pectoralis minor, play important but not primary roles. The rhomboids are important muscles to initiate and maintain external scapular rotation in arm elevation and to control against excessive internal scapular rotation in arm descent. The pectoralis minor assists the serratus anterior as a scapular protractor in pushing activities but frequently becomes tight and shortened. Extrinsic muscles, mainly the latissimus dorsi and pectoralis major, create scapular motion through their effect as prime movers of the arm. Humeral motion also can create scapular motion by tension on the GH capsule and muscles, especially when glenohumeral internal rotation deficit (GIRD) is present. Finally, the scalenes and sternocleidomastoid muscles may affect scapular position due to their effect on clavicle motion.
Since these stability and mobility muscles all attach to the axial skeleton, control of posture and stability in the core is as important for maximal activation of these muscles as control of the scapula is important for maximal rotator cuff activation. Maximal activation of these muscles and force couples only occurs through patterns of activation that start from the core and proceed to the extremities.43,91,136 These patterns coordinate co-contractions and force couples and synergize activation to maximize the developed strength.55,56,134 Recent research shows that lower trapezius and serratus anterior activation is maximized when the recruitment is in a diagonal direction, from the contralateral hip through the lumbodorsal fascia to the lower trapezius.25
Roles of the Scapula in Normal Shoulder Function
The complex motions and translations are necessary to allow the scapula to function as part of SHR, the integrated coupled motion of the moving arm and scapula that is the basis for effective upper extremity use. Dr Carter Rowe has characterized this coupling as “a ball on a sea lion’s nose.” The sea lion moves its body (the scapula) to keep its nose (the glenoid) in line with the moving ball (the humerus) so there is no instability. This dynamic analogy is more physiologic than the static “golf ball on a tee.” The scapula plays several roles to achieve efficient SHR.
First, it allows a congruent ball and socket arrangement through the full ranges of arm motion by keeping the alignment of the humerus and glenoid within physiologic limits. These limits have been calculated to be ±29.3 degrees of G-H angulation.92 This arrangement maximizes the concavity/compression capability of the joint.70 The relatively straight alignment of the bones also allows the rotator cuff muscles
to maximize their efficiency in co-contraction and compression, pulling in straight lines on both sides of the joint. The relatively equivalent amounts of joint compression around the glenoid allows the labrum to work most effectively as a washer for the joint, decreasing peak joint loads and spreading compression effects.126
to maximize their efficiency in co-contraction and compression, pulling in straight lines on both sides of the joint. The relatively equivalent amounts of joint compression around the glenoid allows the labrum to work most effectively as a washer for the joint, decreasing peak joint loads and spreading compression effects.126
Second, it creates a stable base for optimal activation of the scapular-based muscles. Studies in asymptomatic subjects have documented that maximal demonstrated rotator cuff strength can be developed when the scapula is stabilized in a position of neutral retraction.109 Excessive protraction or retraction decreased the developed strength by 11%. In symptomatic subjects, the change was even greater. Stabilization of the scapula in retraction increased the developed strength by 24%.58,114 These changes result from improved stability of the scapula and from the facilitation of rotator cuff activation by increased muscle activation. The use of the stabilized retraction position in the clinical evaluation of rotator cuff strength will increase the test/retest reliability and lead to accurate assessment of changes in strength with treatment.
A third role is one of clearance of the acromion as the arm elevates. Most kinematic studies show that posterior tilt is necessary, in addition to upward rotation, to allow maximum arm flexion.47,74,80 This position allows optimal function in overhead activities, and reduces the occurrence of external impingement symptoms.
The final role is of optimal force transfer from the site of largest force development, the core, to the most common force delivery site, the hand, as part of the kinetic chain of all integrated dynamic body activities. The shoulder acts as a funnel, transmitting and concentrating the developed forces. This function requires dynamic stability for the efficient transfer of energy. The dynamic stability is created by the actions of the scapular stabilizers which are maximized when hip and trunk strength is maximized.25
Alterations of Scapular Motions and Roles: Scapular Dyskinesis
Most discussions regarding alterations in scapular motion center on the terms “winged scapula”62 and “snapping scapula.”63 The “winged” scapula is a descriptive term generally used to identify the patient with an asymmetrically prominent medial scapular border, either at rest or upon arm motion.62 There is commonly a deficit in shoulder function due to the scapular instability. In the past literature, it was assumed that the large majority of cases were due to injury to one of the nerves supplying the scapular stabilizing musculature, either the long thoracic nerve (serratus anterior), accessory nerve (trapezius), or dorsal scapular nerve (rhomboids), or an underlying neuromuscular problem such as muscular dystrophy.9,41,112,133 More recent research has shown that this biomechanical position or motion is more frequently associated with alterations in the supporting bony structure, in the joints of the thoracoscapulohumeral complex, and/or in the strength, flexibility, activation sequencing, and attachment of the stabilizing musculature.12,72,37,48 Therefore, the evaluation of a patient with a winged scapula must be comprehensive enough to identify which of these factors may be causing the altered position and motion.
Similarly, the “snapping” scapula is a descriptive term identifying a patient with painful crepitus along the medial scapular border with arm motion.63 These symptoms have been traditionally ascribed to osteochondromas or other bony pathology, or thickened bursitis in the thoraco-scapular space. More recent research has shown that alterations in normal SHR underlie most of the cases of snapping scapula.63 These alterations create increased compressive pressure along the medial border and contribute to the symptoms. Once again, a comprehensive evaluation of the flexibility and strength of all the surrounding musculature must be done to identify the causative factors.
Since most of the clinical problems associated with the scapula involve some type of alteration of scapular resting position and dynamic motion, it appears that a more general framework should be developed to provide a more effective understanding of the roles of the scapula in shoulder pathology. The most basic concept to unify these thoughts would be the biomechanical term “scapular dyskinesis.”
“Dys” (alteration of) “kinesis” (motion) is a more general term that reflects loss of control of normal scapular physiology, mechanics, and motion. It has the advantage of unifying the thoughts on the scapula and grouping all of the resulting biomechanical deficits and the possible causative factors into a framework for evaluation and treatment, and indicates the possible connections with shoulder pathology.
Dyskinesis by itself is not an injury, not a guarantee of an injury, or directly related to a specific injury. It is characterized by medial or inferior medial border prominence, early scapular elevation or shrugging upon arm elevation, and/or rapid downward rotation upon arm lowering (Fig. 31-4) (Second Scapula Summit. Unpublished consensus statement. Lexington, KY July 20, 2006). The alteration of motion reduces the efficiency of shoulder function in several ways, including changes in threedimensional G-H angulation, A-C joint strain, subacromial space dimensions, maximal muscle activation, and optimal arm
position and motion. If these suboptimal capabilities are combined with functional demands such as joint stability, maximal muscle activation, repetitive joint motions, high joint loads, or specific overhead or forward flexion activities, there may be problems with decreased performance or increased injury risk. In this way it should be considered as a capsular laxity or a sulcus sign, in that it can be a factor producing symptoms, and should be ruled in or out as part of the comprehensive evaluation.
position and motion. If these suboptimal capabilities are combined with functional demands such as joint stability, maximal muscle activation, repetitive joint motions, high joint loads, or specific overhead or forward flexion activities, there may be problems with decreased performance or increased injury risk. In this way it should be considered as a capsular laxity or a sulcus sign, in that it can be a factor producing symptoms, and should be ruled in or out as part of the comprehensive evaluation.
Causative Factors for Scapular Dyskinesis
Normal scapular motion and the alterations that create dyskinesis have been demonstrated by many biomechanical studies utilizing Moire topographic analysis,127 skin electrode monitors,72,76,80,93,123 and indwelling bone pins,73 and it is well established that scapular motion and position are truly altered in many shoulder and arm conditions.72,75,76,79,93
The scapula is stabilized on the axial skeleton and the curved ellipsoid thoracic wall by the bony strut of the clavicle, the intact A-C and S-C joints, and coordinated integrated muscle activation patterns.74 Alterations in all the areas can create dyskinesis.
Excessive thoracic kyphosis or scoliosis can change scapular motion. Acquired thoracic kyphosis creates increased scapular internal rotation and elevation and decreased scapular upward rotation and posterior tilt. These kinematic alterations lead to decreased maximal arm elevation in forward flexion and abduction.32,47
The loss of clavicular strut function can be seen as a result of clavicular fracture, nonunions, or shortened/rotated malunions. In the presence of an intact A-C joint, scapular dyskinesis will result as the scapula follows the position of the distal clavicle fragment. Most frequently, there will be increased scapular internal rotation, increased anterior tilt, and varying degrees of interference with upward rotation. Maximal rotator cuff strength and decreased functional outcomes scores related to decreased strength have been reported in these patients.82
High grade (Types III—VI) A-C separations also impair clavicular strut function by allowing the scapula to move inferiorly and medially to the clavicle creating the “third translation.” This motion results in increased internal rotation and inhibits posterior tilt, creating all of the unfavorable scapular kinematics. It has been documented in greater than 70% of high grade A-C separations.37
Lesions of the nerves that supply the scapular supporting, stabilizing, or moving musculature will create dyskinesis. These include the long thoracic nerve, the accessory nerve, and the dorsal scapular nerve. In addition, cervical disk disease with involvement of the C5-C6 nerve roots can affect scapular muscle function. A rare but frequently missed neurogenic cause is the acute brachial plexitis, or Parsonage-Turner syndrome, most commonly associated with viral illness. Dyskinesis can be associated with both acute nerve deficit and the chronic muscle weakness seen as the nerve injury is healing.
The most common causative mechanisms for scapular dyskinesis involve alterations in the soft tissues. Inflexibility and stiffness of the pectoralis minor and biceps short head create anterior tilt and protraction due to their pull on the coracoid.12 The most common soft tissue inflexibility is GIRD, which creates a “wind-up” of the scapula on the thorax with arm internal rotation or horizontal abduction (Fig. 31-5). GIRD has been frequently associated with impingement and other rotator cuff disease.10,39,49,121
Several studies have documented alterations in periscapular muscle activation in patients with scapular dyskinesis and rotator cuff disease. Serratus anterior activation and strength is decreased in patients with impingement and shoulder pain, contributing to loss of posterior tilt and upward rotation causing dyskinesis.21,69,72 In addition, the upper trapezius/lower trapezius force couple may be altered, with delayed onset of activation in the lower trapezius, which alters upward rotation and posterior tilt.19,20 Finally, fatigue in the periscapular muscles will alter kinematics. The lower portion of the stabilizing force couple, the lower trapezius and serratus anterior, are most susceptible to the effects of fatigue.28,118
An uncommon muscle problem creating dyskinesis is scapular muscle detachment. In this problem, the lower trapezius and rhomboids are anatomically or functionally detached from their scapular attachment sites, almost always secondary to acute tensile trauma. The resulting dyskinesis is associated with pain and impairment of shoulder function because of the deficit in muscle control.
The end result of almost all of these causative factors is the protracted scapula at rest, or the excessively protracting scapula with arm motion. This position which usually results from increased internal rotation and anterior tilt is unfavorable for every shoulder function except the “plus” position in weightlifting. It creates decreased subacromial space and increases impingement symptoms,47,76,110 decreases demonstrated
rotator cuff strength,58,108,109,114 increases strain on the anterior GH ligaments,128 increases the risk of internal impingement,86 and increases strain on the scapular stabilizing muscles. Most of the major goals of treatment of scapular dyskinesis relate to regaining functional retraction capability.
rotator cuff strength,58,108,109,114 increases strain on the anterior GH ligaments,128 increases the risk of internal impingement,86 and increases strain on the scapular stabilizing muscles. Most of the major goals of treatment of scapular dyskinesis relate to regaining functional retraction capability.
The relationship between dyskinesis and shoulder symptoms is not clear in all cases. In cases of nerve injury, fracture, AC separation, or muscle detachment, the injury creates the dyskinesis which affects shoulder function. In other cases, such as rotator cuff disease, labral injury, and multidirectional instability, it may be that the dyskinesis is causative; creating pathomechanics that predispose the arm to injury, or it may be response to the injury, creating pathomechanics that increase the dysfunction. In either case, dyskinesis is present and must be addressed.
These multiple possible causative mechanisms are frequently not isolated, and several may be present in the same patient. Careful examination for the presence or absence of scapular dyskinesis and each of the causative mechanisms should be done as part of the comprehensive evaluation of patients with shoulder injury.
CLINICAL EVALUATION OF THE SCAPULA
The clinical evaluation of the scapula should be inclusive for all possible local and distant contributors to dyskinesis, and also dynamic, since the motion of the scapula is the key component of dyskinesis.
Important questions to ask in the history include past or present trauma to the scapula, clavicle or AC joint, chronic or acute spinal symptoms, recent or remote hip or leg injuries, any surgical procedures on the shoulder, neck symptoms, or viral illness. All of these may have effects on the bony or muscular stabilizing mechanisms. Many patients will have had “therapy,” but it is important to find out the specific content and results of the therapy programs. Physical therapy protocols that emphasize modalities, early open chain rotator cuff exercises with resistance, shoulder shrugs, and shoulder protraction exercises have not been found to be effective for scapular dyskinesis.
The “non scapula” part of the scapular exam can be done mainly by a screening examination. Areas proximal to the scapula to be emphasized include knee, hip, and trunk. Leg and trunk muscle activity and flexibility is important in scapula/shoulder function, as the stable proximal base for distal mobility, as the core for developing force for the arm and hand, and as facilitation for scapula/shoulder muscle activity.
An effective “non-scapula” screening examination includes a one-leg stability series and tests for hip rotation, lumbar flexion/extension, lumbar lordosis/thoracic kyphosis, and cervical lordosis. More detailed analysis can be focused if deficits are found on the screening examination.
The one-leg stability series assesses the patient’s capability of controlling the trunk and body over the planted leg. It has two components, the single leg standing balance test, which evaluates dynamic control of position, and the single-leg squat test, which evaluates dynamic control of motion. In the standing balance test, the patient is asked to place his hands over his chest and stand on one leg with no other verbal cue. Deviations such as a Trendelenburg posture or internally or externally rotating the weight-bearing limb indicates inability to control the posture and has been found to correlate with proximal core weakness, especially in the gluteus medius.38 The single-leg squat is the next progressive evaluation. Assuming the same starting point as the standing balance test, the patient is asked to do repetitive partial half squats going down and returning to the standing position with no other verbal cues. Similar deviations in the quality of the movement are assessed as in the standing balance test. A Trendelenburg posture which may not be noted on standing balance may be brought out with a single-leg squat. The patient may also use his arms for balance or may go into an exaggerated flexed or rotated posture—“corkscrewing”—in order to put the gluteal or short rotator muscles on greater tension to compensate for muscular weakness.24
The scapular examination should concentrate on the evaluation for the presence or absence of scapular dyskinesis and determining the possible effects on the symptoms and signs of the dysfunction. Six main components should comprise the examination of the scapula54: (1) localization of periscapular symptoms; (2) observational scapular assessment; (3) manual muscle testing; (4) posture; (5) muscle tightness; and (6) symptom/sign alteration maneuvers. The results of the examination will aid in establishing the involvement of the scapula and some of the causative factors of the dyskinesis and will help guide treatment and rehabilitation.
Localization of Symptoms
Localization of pain is helpful in the clinical examination. Pain to palpation is commonly found along the medial scapular border, especially close to the scapular spine. Other common areas are the upper trapezius/levator scapulae area along the superior edge, the serratus anterior, and the latissimus dorsi along the lateral scapular border, and the anterior coracoid muscles, pectoralis minor and short head of the biceps. These point tender areas are thought to represent tight, shortened, or spastic muscles and are managed by mobilization techniques. In patients with scapular muscle detachment, the pain is localized along the medial border, and is quite intense, averaging 6.7-8.3/10 numeric pain rating.
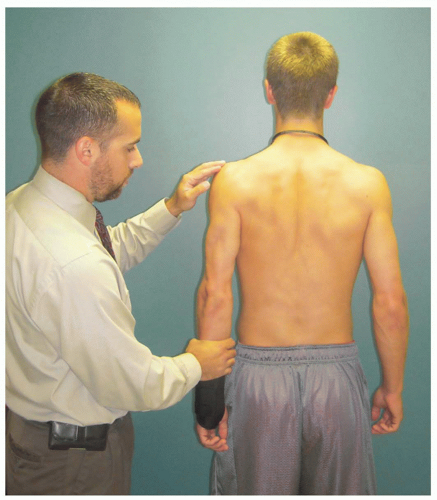
Observational Scapular Assessment
Observational scapular assessment can be difficult due to the overlying tissue and lack of reliable imaging techniques. Much effort has been directed toward developing clinically useful methods for this. A panel of experienced researchers and clinicians reviewed the literature and developed a consensus document reflecting best practices for the scapular examination. This evaluation method involves using the medial border of the scapula as the landmark for scapular orientation, and uses both static position at rest and dynamic motion with arm elevation as observation points. Medial border prominence patterns may be predominantly inferior medial border (Type I), entire medial border (Type II), or superior medial border pattern (Type III), or may be a combination of these patterns.
The scapular examination should largely be accomplished from the posterior aspect. The scapula should be exposed for complete visualization. This can be down by gowning, a tank top, or by removing the shirt. The resting posture should be checked for side-to-side asymmetry but especially for evidence of inferior medial or medial border prominence. If there is
difficulty with determining scapular positions, marking the superior and inferior medial borders may help ascertain the position.
difficulty with determining scapular positions, marking the superior and inferior medial borders may help ascertain the position.
Dynamic scapular motions may be evaluated by having the patient move the arms in ascent and descent three to five times. This will usually bring out any weakness in the muscles and display the dyskinetic patterns. Motion in forward flexion is most likely to demonstrate medial border prominence. Prominence of any part of the medial border is recorded in a “yes” (present) or “no” (absent) fashion.123 This evaluation system shows a clinical utility of 0.64 to 0.84 between the clinical examination and the biomechanical findings.126 If necessary, more repetitions, up to 10, or addition of 3 to 5 pound weights will highlight the weakness even more.81,115 Once this has been demonstrated, tests for strength and flexibility can help determine some of the causative factors.
Manual Muscle Testing
One test advocated to assess the integrity of the lower trapezius and serratus anterior muscles is that of the low row.60 To perform this maneuver, the patient is standing with the involved arm resting at the side with the palm facing posteriorly. The patient is instructed to extend his trunk and push his hand maximally against an examiner’s resistance in the direction of shoulder extension and is instructed to retract and depress the scapula (Fig. 31-6). This maneuver assesses both muscles’ ability to actively stabilize the scapula while providing the examiner a visual depiction of lower trapezius muscle contraction. Other tests such as active scapular squeezing or pinching (rhomboids and middle trapezius) and the wall push-up (serratus anterior) have also been advocated as maneuvers to employ to assess scapular muscle function.49
Posture and Flexibility
Coracoid-based inflexibility can be assessed by palpation of the pectoralis minor and the short head of the biceps brachii at their insertion on the coracoid tip. They will usually be tender to palpation, even if they are not symptomatic in use, can be traced to their insertions as taut bands, and will create symptoms of soreness and stiffness when the scapulae are manually maximally retracted and the arm is slightly abducted to approximately 40 to 50 degrees.57 A rough measurement of pectoralis minor tightness may be obtained by standing the patient against the wall and measuring the distance from the wall to the anterior acromial tip. This can be done using a “double square” device with a patient standing with his back against a wall61 (Fig. 31-7). A bilateral measurement is taken (in inches or centimeters) to determine if there is a notable difference between the involved and non-involved shoulder, with a side-to-side asymmetry > 3 cm considered abnormal.
To obtain accurate G-H internal rotation measurements, the patient should be positioned supine on a flat level surface. A second examiner should be positioned behind the athlete in order to properly stabilize the scapula by applying a posteriorly directed force to the coracoid and humeral head to ensure that scapular movement does not occur. The humerus is supported on the surface with the elbow placed at 90 degrees and the arm on a bolster in the plane of the scapula (Fig. 31-8). A measurement is obtained using a standard bubble goniometer where the fulcrum is set at the olecranon process of the elbow, the stationary arm perpendicular to the table as documented by the bubble on the goniometer, and the moving arm in line with the styloid process of the ulna. The clinician passively moves
the arm into internal and external rotation. Rotation is taken to “tightness,” a point where no more G-H motion would occur unless the scapula would move or the examiner applies rotational pressure. This measurement should be taken bilaterally, and side-to-side differences are calculated. Side-to-side differences in internal rotation greater than 20 degrees are considered a pathologic G-H internal rotation deficit (GIRD).130
the arm into internal and external rotation. Rotation is taken to “tightness,” a point where no more G-H motion would occur unless the scapula would move or the examiner applies rotational pressure. This measurement should be taken bilaterally, and side-to-side differences are calculated. Side-to-side differences in internal rotation greater than 20 degrees are considered a pathologic G-H internal rotation deficit (GIRD).130
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree