Most lumbar disk herniations improve over time with or without medical treatment. Disk herniations and annular tears may not be symptomatic and are shown to exist in patients without any symptoms. In some patients, chronic low back pain may result from the syndrome of internal disk disruption. Treatment of chronic pain of diskal cause can be challenging and have varying results in terms of success. The diagnosis, cause, and treatment options are reviewed in this article.
Key points
- •
The intervertebral disk can be a common source of acute or chronic low back pain.
- •
A thorough history and physical examination are needed to assess patients with discogenic low back pain.
- •
Lifestyle modifications including smoking cessation, proper lifting mechanics, ergonomics, and lower body mass index are helpful.
- •
Discogenic pain results from changes in the nucleus pulposus and tears in the annulus fibrosis.
- •
Psychological support, including treatment of underlying or coexistent depression, is highly recommended.
- •
Conservative treatment, including home exercise for chronic lower back pain, is recommended.
- •
Injection of corticosteroids for discogenic lower back pain shows mixed efficacy and should be performed judiciously.
- •
Surgery for this condition should be reserved for cases of significant refractory cases with profound disability and should be confirmed with diskography.
Introduction
Nature of the Problem
Chronic low back pain is a common and challenging problem presenting to a variety of practitioners. It is estimated that up to 90% of people experience significant lower back pain in their lifetime. Although low back pain was traditionally believed to be self-limited in most cases, data have emerged showing that many low back pain sufferers have recurrences or go on to a more chronic course.
The economic burden of lower back pain is staggering. It is estimated that the annual cost in the United States for the treatment of lower back pain is between 20 and 50 billion dollars. The pain can be debilitating in many cases and is a major reason for absence from work.
In most cases of acute lower back pain, a definite pain generator cannot be defined. For chronic low back pain sufferers, an estimated 39% of cases can be attributed to the intervertebral disk. This situation is complicated because not all degenerated or herniated disks are painful. Disk degeneration is a natural part of the aging process and normally begins about the third decade of life. In the right clinical setting, the disk can become a primary source of pain. The following sections address the challenging problem of pain emanating from the damaged and sensitized lumbar intervertebral disk.
Anatomy
The human intervertebral disk consists of a firm, collagenous exterior annulus fibrosis and a gelatinous interior nucleus pulposus. It is often compared with a jelly donut. This structure offers shock absorption and allows for the dispersion of axial and torsional forces at each level through the spine. The annulus is thicker anteriorly than superiorly, therefore herniations and tears are more common posteriorly. The nerve supply to the human intervertebral disk consists of contributions from the sinuvertebral nerves and gray rami communicantes. These nerves are segmental and from the dorsal ramus, but recent studies have shown some contributions from the sympathetic chain in a nonsegmental distribution.
Pathophysiology
Pain from lumbar disks can occur from 3 main causes, as described extensively by Bogduk. These causes include disk infection, torsion injury, and internal disk disruption (IDD). This review focuses on torsion injury and IDD.
Torsion injury is believed to result from forcible rotation of the intervertebral joint. Rotational forces around an impacted zygapophysial joint produce a lateral shear force on the disk, which can lead to circumferential tears. This cause of disk pain is difficult to prove with objective testing. It is a clinical diagnosis related to patient history, often related to a rotational strain injury.
IDD results from lumbar disk degradation, its nuclear components, and development of radial fissures that extend from the nucleus into the annulus. IDD is believed to be the most common type of discogenic pain. Disk disruption is not to be confused with degenerative changes, which are a normal part of aging. Studies have suggested IDD to be independent of degenerative changes that are seen with aging. Furthermore, it is well known that degenerative disk changes related to aging do not correlate with pain.
The development of radial fissures is believed to be related to repetitive shear, axial loads, and compression of the disk. This process leads to vertebral endplate fractures, in which the fissures can develop followed by disk degradation over time as nuclear material leaks out of the disk or desiccates.
Radial fissures may correlate with pain. A process of sensitization and neural ingrowth are proposed mechanisms of the development of IDD. Pain-associated proinflammatory mediators including calcitonin gene-related peptide, tumor necrosis factor α, interleukin 1, interleukin 6, and substance P have been isolated from disks with this morphology.
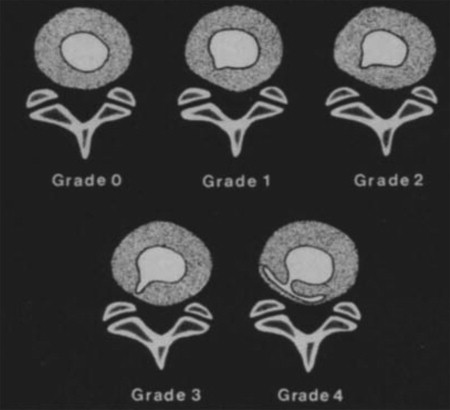
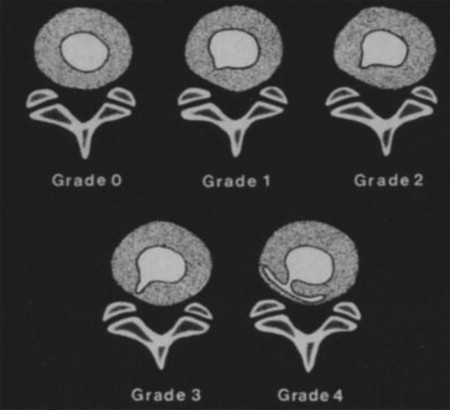
The modified Dallas diskogram scale is a descriptive way to categorize the severity of IDD after diskography ( Fig. 1 ). Using this scale, grade 1 and 2 fissures often produce no pain, whereas grade 3 and 4 fissures frequently produce pain.
Patient History
Patients may describe an injury such as a bending, lifting, twisting event and the sensation of a pop in the lower back. In some cases, no inciting event may occur.
The typical patient history is of pain in the center of the lower back with minimal radiation, usually to 1 or both buttocks. Radiation may occur to 1 or both sides of the lower back. The pain may have an absent or intermittent radicular component. The back pain is the most severe element of the syndrome. Pain may be reduced with extension and is better with standing and lying flat.
The pain is often described as a deep, dull ache. There is often tightness in the paraspinal and gluteal muscles. Pain is often worsened with sitting/driving, lumbar flexion, bending, twisting, Valsalva maneuver, and coughing. Increased intrathecal and intradiskal pressures are believed to play a role. The pain in some cases can be constant or mechanical, often worse with activity and toward the end of the day. Bending and twisting may provoke symptoms.
Smokers, the obese, those with jobs requiring prolonged sitting, and those with physical jobs, especially with repetitive lifting and vibration exposure, are at increased risk of discogenic lower back pain and lumbar disk disease.
Genetics may play a role in disk degeneration. One study of twins showed an increased relationship with disk degeneration. A systematic review of 52 articles on degenerative disk disease looking at different genetic markers showed poor data and association.
Physical Examination
- •
Observe the patient’s posture, spinal curvature, and gait.
- •
Look for asymmetry or atrophy.
- •
Patients are often more comfortable standing than sitting in the examination room.
- •
Lumbar range of motion is often reduced in flexion, but may be reduced in all planes because of pain.
- •
Strength and sensation are usually normal. Reflexes are often normal, but may be blunted if there was a previous associated radiculopathy.
- •
Provocative maneuvers for neural tension such as straight leg raise, seated straight leg raise, and slump test may cause lower back or buttock pain that is concordant because of the flexion moment created in the lumbar region.
- •
Femoral nerve stretch test can be negative, because an extension moment is created with these maneuvers.
- •
Transmitting vibration via the spinous process may cause pain at the symptomatic level but is not sensitive or specific.
Imaging and Additional Testing
Radiographs are often performed as an initial screening tool but are not sensitive or specific for discogenic low back pain. Radiographs are useful in determining if there is an associated spondylolithesis, compression fracture, sacroiliac sclerosis, some bony disease, or other potential mimickers. The only finding that may support discogenic lower back pain may be disk space narrowing.
Magnetic resonance imaging (MRI) can show disk degeneration. A commonly used grading system for disk degeneration was described by Pfirrman and colleagues. This system assigns grades I to V to assess the degree of disk degeneration and looks at the structure, morphology of the annulus and nucleus, the signal intensity of the disk, and the disk height. Degeneration, even a Pfirrman grade V, is not necessarily painful, and disk degeneration is considered a natural phenomenon of aging.
Tears in the annulus may also be present and appear as a high signal in the posterior annulus on T2-weighted images, or high intensity zone. These tears are shown to have a high incidence of concordant pain when stimulated during provocative diskography. However, the presence of a high intensity zone on MRI does not necessarily mean the patient has pain.
Provocative diskography remains the gold standard for the diagnosis of discogenic lower back pain. This test was first performed in 1948 and remains a source of controversy. It consists of accessing the intervertebral disk through the placement of needles into the nuclei with the use of fluoroscopy ( Fig. 2 ). Contrast is administered under live or intermittent fluoroscopy, and pressures are measured with a manometer. Pain level on a visual analog scale, location of pain, similarity to typical pain, facial grimacing, and morphology of the disk after contrast administration are recorded. A positive disk reproduces the patient’s typical pain (concordant pain) and is considered consistent with IDD. A negative disk causes no pain or production of dissimilar (discordant) pain. Control disks are also necessary for more accurate results. For example, if stimulation of the L5-S1 disk reproduces the patient’s typical pain and has abnormalities on the fluoroscopy pictures, but the L4-5 and L3-4 disks do not, this would be considered a more reliable result.

The Derby criteria are a well-described method of interpreting diskography, in which concordant responses must produce pain greater than 6 out of 10 on a numeric pain scale at a pressure of less than 50 psi above the opening pressure of the disk and having a negative control disk. The opening pressure is the manometry reading when dye is first observed to enter the disk. In addition, a nucleogram is performed after the disk stimulation, and this must be abnormal, showing a grade 3 tear or higher on the modified Dallas diskogram scale, to prove a diagnosis of IDD.
Patients with suspected IDD are identified and informed as to the risks and benefits of the procedure. The procedure need not be performed if the patient and physician are not seriously considering surgery or an intradiskal procedure as treatment (see later discussion). Because of the relatively avascular nature of the disk, infection is a serious potential risk. It is recommended that periprocedure intravenous antibiotics be administered and the procedure performed under sterile conditions. Many practitioners use a 2-needle technique, in which an introducer needle is placed through the skin and soft tissues and a spinal needle placed into the disk through the needle.
Diskography, when performed by skilled practitioners under sterile technique, has historically been viewed as a safe procedure. In reviewing the usefulness in surgical planning, studies have supported its role. However, Carragee and colleagues recently followed patients who underwent lumbar diskography and found an increased risk of far lateral disk herniations and a more rapid rate of disk degeneration over a 10-year period compared with controls.
Management of Discogenic Low Back Pain
Goals of management of IDD are:
- •
Improvement in pain threshold, quantified on a pain rating scale
- •
Improvement in function, shown by a reduction in dependence on caregivers, return to work, and participation in recreational activities
Pharmaceutical management
Pharmacologic management is for analgesic purposes. The use of opioid medications is discouraged as a long-term treatment. Neuropathic pain agents may be used for concomitant radicular symptoms. For a complete discussion of medications, please refer to the separate medication section.
Acetaminophen
Acetaminophen or paracetamol continues to be recommended by the American Pain Society (APS)/American College of Physicians (ACP) as a first-line pharmacologic option for back pain of any duration because of its comparable efficacy and safety considerations. No clear difference has been established comparing acetaminophen with nonsteroidal antiinflammatory drugs (NSAIDs).
NSAIDs
NSAIDs have both antiinflammatory and analgesic properties via inhibition of the cyclooxygenase 2 enzyme, which confers efficacy in management of discogenic back pain. A high-quality Cochrane review of 51 trials analyzing NSAIDs for acute low back pain found nonselective NSAIDs superior to placebo for global improvement and for not requiring additional analgesics. This study did not show that any nonselective NSAID was superior to any other for pain relief. The review showed that there was no clear difference in efficacy between NSAIDs and opioid therapy, spinal manipulation, physical therapy, and bed rest when studying pain reduction.
Skeletal muscle relaxants
Skeletal muscle relaxants are medications grouped together because they are used for the treatment of spasticity and musculoskeletal conditions such as tension headaches and back pain. A variety of skeletal muscle relaxants are available in the United States. Dantrolene, a peripheral calcium channel blocker, and baclofen, a γ aminobutyric acid modulator in the spinal cord, have not been shown to have any significant benefit in reducing back pain, which is logical given their mechanisms of action. Some evidence supports the short-term use of muscle relaxants for acute lower back pain. However, it remains unclear whether any of these medications truly relax muscles or if their effects on pain are related to sedation.
Tramadol
Tramadol is a μ-opiate agonist and a norepinephrine and serotonin reuptake inhibitor. It has shown significant efficacy in the treatment of lower back pain. It has the potential to have an effect on the radicular or neurogenic components, if present, with discogenic pain.
Tramadol has also shown significant potential in the combination setting, effectively addressing chronic lower back pain in a double-blind randomized controlled trial, and allowing for dose-reduction with NSAIDs.
Corticosteroids
Many practitioners prescribe a short course of oral corticosteroids for an acute flare or episode of lower back pain. Typically, a tapering dose of methylprednisolone or prednisone is used. The appeal is the high potency of the antiinflammatory effects and the short duration (days) of treatment with few contraindications. However, data are lacking on the efficacy of this treatment.
Opioids
The role of opioids remains controversial, because they may lead to physical dependence and tolerance and have many undesirable effects when used chronically. There is some low-level evidence that for severe low back pain, opioids may have benefit. Data on the effectiveness of long-term opioids for discogenic back pain are lacking, and studies indicate no significant reduction in pain or improvement in quality of life. Extensive monitoring and close follow-up are crucial to safe use of opioids for analgesia.
Nonpharmacologic strategies
Physical therapy
A variety of physical therapy approaches have been used to address discogenic back pain. Adams and colleagues suggest that extension-biased therapy program may be superior. The McKenzie extension program for lumbar disk herniations with associated radicular pain has been shown to be effective as well, but not so effective if the pain is purely axial. There is also literature to suggest that combining physical therapy with education and manual therapy is superior to physical therapy alone.
Cognitive behavioral therapy with pain education
Although many consensus statements and a recent Cochrane review have recommended a cognitive behavioral approach to maximize physical and psychological well-being, the effect is often minimal and short-term. Van Hooff and colleagues sought to identify risk factors by multivariate analysis of a prospective study of the effect of combined physical and cognitive behavioral therapy (CBT) in patients with chronic low back pain. Patients’ work status and lower pretreatment disability are important predictors of 1-year success after treatment. This factor may help guide patient selection for this therapy.
Acupuncture
Originating from traditional Chinese medicine, acupuncture is increasingly used as an adjunctive treatment in Western medical practice. Furlan and colleagues examined the role of acupuncture in the treatment of acute and chronic lower back pain in a Cochrane review. This study showed no evidence for acupuncture in acute low back pain but some evidence suggesting that it may be better than no treatment or sham treatment of chronic low back pain. Per this meta-analysis, there was not sufficient evidence to conclude that acupuncture is more effective than other conventional treatments.
Similarly, multiple meta-analyses have concluded that true acupuncture is no more effective than sham acupuncture, but that both were significantly more effective than no treatment, thus highlighting the effect of the acupuncture experience as a whole, including the psychosocial context and the therapeutic milieu. Benefits of acupuncture were also shown in the GERAC (German Acupuncture) trial compared with conventional treatments.
Manual medicine: osteopathic and chiropractic manipulation
Manual medicine is often used as adjunctive therapy with medical or interventional management and may have a role in improving back-specific functioning and patient satisfaction with therapy. It is difficult to study because of different techniques and the effects of clinician touch, and therefore, sham treatments as well as a study group and a nontreatment group are required. Studies are conflicting in terms of the efficacy of manual therapy for chronic back pain sufferers. A study showed comparative outcomes with osteopathic manipulation and standard medical treatments (analgesics, antiinflammatory medication, active physical therapy, or therapies such as ultrasonography, diathermy, hot or cold packs [or both], use of a corset, or transcutaneous electrical nerve stimulation) in treating subacute lower back pain. A study by Zylbergold and Piper showed no statistical difference comparing outcomes with manual therapy with flexion exercise or home care. However, an extension program rather than flexion program would have been more appropriate. A review of the literature found good evidence for moderate benefit in chronic low back pain sufferers, as well as CBT, exercise, and multidisciplinary rehabilitation.
Self-management strategies
Yoga and tai chi
- •
Several randomized controlled studies have shown that yoga can help motivated individuals reduce back pain and improve back function. Yoga shows more effectiveness in the short-term than in the long-term. There are some data that it is superior to other self-help strategies, including books, but unclear if it is superior in the long-term over a therapeutic exercise program.
- •
Tai chi incorporates exercise and meditation and attempts to create a mindfulness of the body. Some data suggest that tai chi may be moderately effective in coping with lower back pain, but the studies are of low quality.
Meditation
- •
There are inconclusive data that meditation is helpful for improving outcomes with chronic lower back pain. Mind-body strategies have shown benefit compared with patient education.
Interventional options
Because of the chronic and often debilitating nature of the condition, as well as the mixed data/patient responses as noted earlier, interventional options are considered in the treatment of IDD. These treatments include administration of corticosteroids either epidurally or into the disk itself, intradiskal procedures targeted at the annular tears, and surgery. There is little consensus and mixed data on these procedures. The risks and benefits must be weighed when considering any procedure, especially if the condition is not life threatening.
Lumbar Epidural Steroid Injections
- •
The logic behind the use of epidural steroid injection in the treatment of IDD is to deliver antiinflammatory corticosteroid to the outer annulus. As noted, studies have shown the presence of inflammatory mediators in the disrupted disk. Studies have shown usefulness in the administration of epidural steroids via the caudal, interlaminar, or transforaminal route in the treatment of chronic lower back pain. However, these studies are not specific to discogenic lower back pain.
- •
Intradiskal steroid injections have not shown convincing benefit and are not a routinely performed procedure for lower back pain. One study showed a weak benefit of the administration of corticosteroids during diskography if degenerative endplate changes were also present. Another study showed some short-term benefit of intradiskal steroid in patients with Modic endplate changes.
Thermal Intradiskal Procedures
Various types of intradiskal procedures have been performed in the attempt to seal annular tears or coagulate the innervation to the disk. It is beyond the scope of this article to go into detail on each of these techniques, but some of the more common procedures are discussed.
- •
Intradiskal thermal annuloplasty (IDET) is a procedure in which a wire with contact points is placed through an introducer needle into the lumbar disk. This wire is then heated for 16 minutes to 90°C. The mechanism of action is unknown, but the theory is that heating denervates the nocioceptors in the annulus and also increases collagen fiber stability in annulus fibers by modifying their shape. Complications include catheter breakage, nerve injury, post-IDET disk herniation, diskitis, and epidural abscess. Although the primary studies were promising, recent studies have not provided sufficient evidence for using IDET for discogenic back pain. Further randomized clinical trials are needed to evaluate the efficacy of IDET in discogenic back pain treatment.
- •
Biacuplasty uses a radiofrequency current between 2 probes and creates heat in the posterior annulus. The temperature increases gradually to 50°C while the patient is awake and alert for communication. Biacuplasty has some advantages over IDET, including minimal damage to the tissue and easier targeting of the posterior annulus. Even although there were some promising results from pilot studies, further randomized clinical trials are required.
Introduction
Nature of the Problem
Chronic low back pain is a common and challenging problem presenting to a variety of practitioners. It is estimated that up to 90% of people experience significant lower back pain in their lifetime. Although low back pain was traditionally believed to be self-limited in most cases, data have emerged showing that many low back pain sufferers have recurrences or go on to a more chronic course.
The economic burden of lower back pain is staggering. It is estimated that the annual cost in the United States for the treatment of lower back pain is between 20 and 50 billion dollars. The pain can be debilitating in many cases and is a major reason for absence from work.
In most cases of acute lower back pain, a definite pain generator cannot be defined. For chronic low back pain sufferers, an estimated 39% of cases can be attributed to the intervertebral disk. This situation is complicated because not all degenerated or herniated disks are painful. Disk degeneration is a natural part of the aging process and normally begins about the third decade of life. In the right clinical setting, the disk can become a primary source of pain. The following sections address the challenging problem of pain emanating from the damaged and sensitized lumbar intervertebral disk.
Anatomy
The human intervertebral disk consists of a firm, collagenous exterior annulus fibrosis and a gelatinous interior nucleus pulposus. It is often compared with a jelly donut. This structure offers shock absorption and allows for the dispersion of axial and torsional forces at each level through the spine. The annulus is thicker anteriorly than superiorly, therefore herniations and tears are more common posteriorly. The nerve supply to the human intervertebral disk consists of contributions from the sinuvertebral nerves and gray rami communicantes. These nerves are segmental and from the dorsal ramus, but recent studies have shown some contributions from the sympathetic chain in a nonsegmental distribution.
Pathophysiology
Pain from lumbar disks can occur from 3 main causes, as described extensively by Bogduk. These causes include disk infection, torsion injury, and internal disk disruption (IDD). This review focuses on torsion injury and IDD.
Torsion injury is believed to result from forcible rotation of the intervertebral joint. Rotational forces around an impacted zygapophysial joint produce a lateral shear force on the disk, which can lead to circumferential tears. This cause of disk pain is difficult to prove with objective testing. It is a clinical diagnosis related to patient history, often related to a rotational strain injury.
IDD results from lumbar disk degradation, its nuclear components, and development of radial fissures that extend from the nucleus into the annulus. IDD is believed to be the most common type of discogenic pain. Disk disruption is not to be confused with degenerative changes, which are a normal part of aging. Studies have suggested IDD to be independent of degenerative changes that are seen with aging. Furthermore, it is well known that degenerative disk changes related to aging do not correlate with pain.
The development of radial fissures is believed to be related to repetitive shear, axial loads, and compression of the disk. This process leads to vertebral endplate fractures, in which the fissures can develop followed by disk degradation over time as nuclear material leaks out of the disk or desiccates.
Radial fissures may correlate with pain. A process of sensitization and neural ingrowth are proposed mechanisms of the development of IDD. Pain-associated proinflammatory mediators including calcitonin gene-related peptide, tumor necrosis factor α, interleukin 1, interleukin 6, and substance P have been isolated from disks with this morphology.
The modified Dallas diskogram scale is a descriptive way to categorize the severity of IDD after diskography ( Fig. 1 ). Using this scale, grade 1 and 2 fissures often produce no pain, whereas grade 3 and 4 fissures frequently produce pain.