Abstract
Background and purpose
The ability to rise from a chair to reach a standing position is impaired after stroke. This paper aims to review for the first time the factors that impact the ability to rise from a chair and identify recommendations for post-stroke rehabilitation.
Methods
In order to analyse relevant scientific publications (French and English), the search terms “stroke”, “rehabilitation” and “sit-to-stand” (STS and its variations) were used. The initial literature search identified 122 titles and abstracts for full review and 46 were retained because both the junior and senior researchers agreed that they were aligned with the objectives of this review.
Results and conclusion
During STS, most individuals with hemiparesis able to stand independently presented several changes such as lateral deviation of the trunk towards the unaffected side (ipsilesional side), asymmetrical weight bearing (WB) and asymmetry of knee moment forces. Interestingly, the WB asymmetry was observed even before seat-off, when subjects with hemiparesis still had their thighs in contact with the chair suggesting a planned strategy. Among other interesting results, the time to execute the STS was longer than in controls and influenced by the sensorimotor deficits. A greater risk of falling was observed with a need for more time to stabilize the body during STS and especially during the extension phase. Some rehabilitation interventions may be effective in improving STS duration, WB symmetry and the ability to stand independently with repeated practice (mentally or physically) of STS tasks. However, more research is essential to further investigate effects of specific training protocols and pursue better understanding of this complex and demanding task, particularly for stroke patients who need assistance during this transfer.
1
Introduction
Stroke is the third cause of mortality in the world . As one of the most common causes of long-term disability, stroke imposes an enormous economic burden in several countries and caring for stroke survivors put social, emotional, health and financial burdens and strains on the informal caregivers . After stroke, patients usually present sensorimotor impairments contralateral to the cerebral lesion that contribute to limiting their ability to perform functional activities such as walking , standing and sit-to-stand (STS) . STS, which is considered a fundamental prerequisite for daily activities, is commonly compromised and individuals post-stroke do not easily recover this ability to rise safely from a chair . Therefore, it is important to have a better understanding of how STS is accomplished and to know the important factors to consider in order to improve the patients’ performance.
The most important determinants to consider during a STS task were already reviewed for healthy subjects but not for hemiparetic individuals. Some of these determinants have been studied extensively in hemiparetic individuals and are commonly accepted, while others still need further research. The objective of this topical review is to present advances in research and clinical topics relevant to factors that may affect the ability to execute STS after stroke and to identify recommendations for post-stroke rehabilitation.
2
Methods
A literature review was conducted to identify relevant scientific publications concerning STS execution by people affected by stroke. The literature search was carried out in Medline. The search terms “stroke”, “rehabilitation” and “sit-to-stand” (and its variations) were used. There was a restriction for French and English language but no restrictions for publication date or study design. From the initial literature search, 122 titles and abstracts were appraised to identify papers for full review. Among these articles, only 29 were retained because they were consistent with the objectives of this review. The reference section from each initially selected article was searched manually and 17 other relevant publications were added. Finally, the study results from 46 articles were extracted and a narrative synthesis was compiled. The content of these 46 articles was validated by a senior researcher expert with STS literature.
2.1
STS description
Roebroeck et al. described STS as a movement of the body’s center of mass (CoM) upward from a sitting position to a standing position without losing balance. Similarly, Vander Linden et al. added that it is a transitional movement to the upright posture requiring movement of CoM from a stable position to a less stable position over extended lower extremities. For Galli et al. (2008) , STS requires skills, such as coordination between trunk and lower limb movements, muscle strength, control of equilibrium and stability.
To simplify its analysis, authors divided STS into phases that depend on kinematic variables, ground forces and CoM movement. Schenkman et al. distinguished four phases. The seat-off, which refers to the moment when only the feet are in contact with the ground and no force is applied on the seat, is often used to identify STS phases. The first phase is the flexion momentum phase, which begins with the initiation of movement and ends just before the thighs lift off from the chair. The second phase, the momentum-transfer phase, begins with seat-off and continues with the anterior and upward CoM displacement. The anterior displacement of the CoM brings it close to the center of pressure (CoP) to reach a quasi-static stability position. The third phase is designated as the extension phase. It is initiated just after maximal ankle dorsiflexion is reached and continues until hips ceases to extend. The stabilization phase is the last phase of STS. It begins just after hip extension velocity reaches 0°/s and continues until all motion associated with stabilization from rising is achieved.
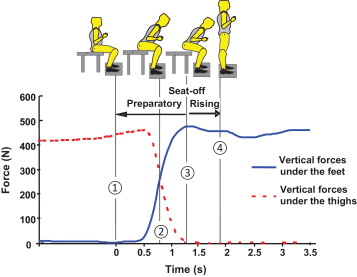
Other authors simplified STS by referring to only two phases: STS begins with the preparatory phase defined as onset of an anterior-posterior force beneath the thighs and lasts until seat-off. The second phase is the rising or extension phase, which lasts from seat-off until CoM vertical velocity decreases to zero ( Fig. 1 ). As it is the most recent description, we will distinguish only two phases in our review of STS determinants in the next sections. However, specific events of STS namely onset, the transition phase, the seat-off and the end of the task will also be used. These events corresponded respectively to the first perceptible changes of the vertical force on feet or thighs, almost similar forces under both feet and thighs, the point where the subject is just leaving the seat and the beginning of a stable extension of the hips in the standing position .
2.2
STS determinants in healthy individuals
STS determinants in healthy individuals have been described in a review by Janssen et al. . In this section, we voluntarily limited the review to concepts that are important for the analysis in individuals post stroke.
2.3
Angular displacements of lower limbs and trunk
In order to rise from a chair, Nuzik et al. reported that hips bent during the first 40% of the STS cycle, and then, continued with extension for the last 60%. Knees moved in extension during the whole cycle. The dorsal flexion of ankles occurred at 20% of cycle and then a plantar flexion movement was observed. When healthy subjects rose from a chair with feet placed in spontaneous (no instructions given on the initial foot position) and symmetrical (both feet placed at 15° of dorsiflexion) positions, the trunk was near the neutral position on the frontal plan during STS . However, when the feet were placed asymmetrically, healthy subjects rose with the trunk deviated towards the foot placed behind . On the sagittal plan, the trunk initially moved forward during the first 53.3% of the STS movement cycle with a mean distance of 489.6 mm, then upright for 49.8% of the cycle and finally backward to attain stable standing .
2.4
Muscular activation pattern of lower limbs
A bilateral specific muscular activation sequence in a concentric mode, is required to reach the standing posture from the seated position. Tibialis anterior muscles were activated first in order to stabilize the feet before beginning the forward body movement . Tibialis anterior activation was followed by knee and hip extensor muscles, which reached their peak of activity at seat-off . First, iliopsoas initiated hip flexion then quadriceps, as a biarticular muscle, continued hip flexion, stabilized the knees and allowed their extension . After seat-off, hamstrings decelerated the initial hip flexion and therefore promoted hip extension in order to initiate the extension phase of STS . In order to balance the forward movement, the tibialis anterior provided dorsiflexion torques at the ankles to maintain the CoP in a posterior position under the feet . At the end of STS, the activation of the gastrocnemius and soleus muscles enhanced control of the body’s forward transition .
2.5
CoM behaviour
To rise from a chair, an individual needs to bring his CoM from a relatively large and stable base of support in sitting to a considerably smaller base of support in standing . To achieve this transition, CoM must first move forward then reach its maximal velocity at the preparatory phase . At seat-off, CoM switches into vertical movement and its velocity continues to accelerate until it reaches a maximum at the middle of the extension phase. Subsequently, the CoM velocity decelerates progressively until reaching zero, when the standing position is achieved .
2.6
Weight bearing distribution
Hirschfeld et al. examined weight bearing (WB) distribution between feet and thighs during STS. They concluded that before seat-off, healthy individuals distributed about 85% of their weight under their thighs and 15% under their feet. During the extension phase, force under the feet rose from 52% of corporal weight to total corporal weight at the end of STS. Lecours et al. studied the effect of change in foot position on WB distribution between lower limbs. They found that with the feet placed in spontaneous and symmetrical positions, healthy subjects presented almost equal loading on both lower limbs during seat-off. However, when the non-dominant foot was moved forward, healthy persons increased their loading on the posterior foot (dominant) and an asymmetrical WB distribution was induced . Along the same line, Brunt et al. demonstrated that when the dominant foot was placed in extended (dominant foot was positioned such that the knee angle equaled 75°of flexion) or elevated positions (foot placed on dense foam where thickness was adjusted to 25% of the chair height), the ground reaction forces under this foot in the vertical and anteroposterior directions decreased relative to the non-dominant foot. Therefore, the posterior position of one foot seems to advantageously increase WB in comparison to an extended or elevated foot position.
2
Methods
A literature review was conducted to identify relevant scientific publications concerning STS execution by people affected by stroke. The literature search was carried out in Medline. The search terms “stroke”, “rehabilitation” and “sit-to-stand” (and its variations) were used. There was a restriction for French and English language but no restrictions for publication date or study design. From the initial literature search, 122 titles and abstracts were appraised to identify papers for full review. Among these articles, only 29 were retained because they were consistent with the objectives of this review. The reference section from each initially selected article was searched manually and 17 other relevant publications were added. Finally, the study results from 46 articles were extracted and a narrative synthesis was compiled. The content of these 46 articles was validated by a senior researcher expert with STS literature.
2.1
STS description
Roebroeck et al. described STS as a movement of the body’s center of mass (CoM) upward from a sitting position to a standing position without losing balance. Similarly, Vander Linden et al. added that it is a transitional movement to the upright posture requiring movement of CoM from a stable position to a less stable position over extended lower extremities. For Galli et al. (2008) , STS requires skills, such as coordination between trunk and lower limb movements, muscle strength, control of equilibrium and stability.
To simplify its analysis, authors divided STS into phases that depend on kinematic variables, ground forces and CoM movement. Schenkman et al. distinguished four phases. The seat-off, which refers to the moment when only the feet are in contact with the ground and no force is applied on the seat, is often used to identify STS phases. The first phase is the flexion momentum phase, which begins with the initiation of movement and ends just before the thighs lift off from the chair. The second phase, the momentum-transfer phase, begins with seat-off and continues with the anterior and upward CoM displacement. The anterior displacement of the CoM brings it close to the center of pressure (CoP) to reach a quasi-static stability position. The third phase is designated as the extension phase. It is initiated just after maximal ankle dorsiflexion is reached and continues until hips ceases to extend. The stabilization phase is the last phase of STS. It begins just after hip extension velocity reaches 0°/s and continues until all motion associated with stabilization from rising is achieved.
Other authors simplified STS by referring to only two phases: STS begins with the preparatory phase defined as onset of an anterior-posterior force beneath the thighs and lasts until seat-off. The second phase is the rising or extension phase, which lasts from seat-off until CoM vertical velocity decreases to zero ( Fig. 1 ). As it is the most recent description, we will distinguish only two phases in our review of STS determinants in the next sections. However, specific events of STS namely onset, the transition phase, the seat-off and the end of the task will also be used. These events corresponded respectively to the first perceptible changes of the vertical force on feet or thighs, almost similar forces under both feet and thighs, the point where the subject is just leaving the seat and the beginning of a stable extension of the hips in the standing position .

2.2
STS determinants in healthy individuals
STS determinants in healthy individuals have been described in a review by Janssen et al. . In this section, we voluntarily limited the review to concepts that are important for the analysis in individuals post stroke.
2.3
Angular displacements of lower limbs and trunk
In order to rise from a chair, Nuzik et al. reported that hips bent during the first 40% of the STS cycle, and then, continued with extension for the last 60%. Knees moved in extension during the whole cycle. The dorsal flexion of ankles occurred at 20% of cycle and then a plantar flexion movement was observed. When healthy subjects rose from a chair with feet placed in spontaneous (no instructions given on the initial foot position) and symmetrical (both feet placed at 15° of dorsiflexion) positions, the trunk was near the neutral position on the frontal plan during STS . However, when the feet were placed asymmetrically, healthy subjects rose with the trunk deviated towards the foot placed behind . On the sagittal plan, the trunk initially moved forward during the first 53.3% of the STS movement cycle with a mean distance of 489.6 mm, then upright for 49.8% of the cycle and finally backward to attain stable standing .
2.4
Muscular activation pattern of lower limbs
A bilateral specific muscular activation sequence in a concentric mode, is required to reach the standing posture from the seated position. Tibialis anterior muscles were activated first in order to stabilize the feet before beginning the forward body movement . Tibialis anterior activation was followed by knee and hip extensor muscles, which reached their peak of activity at seat-off . First, iliopsoas initiated hip flexion then quadriceps, as a biarticular muscle, continued hip flexion, stabilized the knees and allowed their extension . After seat-off, hamstrings decelerated the initial hip flexion and therefore promoted hip extension in order to initiate the extension phase of STS . In order to balance the forward movement, the tibialis anterior provided dorsiflexion torques at the ankles to maintain the CoP in a posterior position under the feet . At the end of STS, the activation of the gastrocnemius and soleus muscles enhanced control of the body’s forward transition .
2.5
CoM behaviour
To rise from a chair, an individual needs to bring his CoM from a relatively large and stable base of support in sitting to a considerably smaller base of support in standing . To achieve this transition, CoM must first move forward then reach its maximal velocity at the preparatory phase . At seat-off, CoM switches into vertical movement and its velocity continues to accelerate until it reaches a maximum at the middle of the extension phase. Subsequently, the CoM velocity decelerates progressively until reaching zero, when the standing position is achieved .
2.6
Weight bearing distribution
Hirschfeld et al. examined weight bearing (WB) distribution between feet and thighs during STS. They concluded that before seat-off, healthy individuals distributed about 85% of their weight under their thighs and 15% under their feet. During the extension phase, force under the feet rose from 52% of corporal weight to total corporal weight at the end of STS. Lecours et al. studied the effect of change in foot position on WB distribution between lower limbs. They found that with the feet placed in spontaneous and symmetrical positions, healthy subjects presented almost equal loading on both lower limbs during seat-off. However, when the non-dominant foot was moved forward, healthy persons increased their loading on the posterior foot (dominant) and an asymmetrical WB distribution was induced . Along the same line, Brunt et al. demonstrated that when the dominant foot was placed in extended (dominant foot was positioned such that the knee angle equaled 75°of flexion) or elevated positions (foot placed on dense foam where thickness was adjusted to 25% of the chair height), the ground reaction forces under this foot in the vertical and anteroposterior directions decreased relative to the non-dominant foot. Therefore, the posterior position of one foot seems to advantageously increase WB in comparison to an extended or elevated foot position.
3
STS determinants for hemiparetic patients in the reviewed studies
The differences related to the factors that differ between hemiparetic and healthy subjects will be discussed in the next section.
3.1
Angular displacements of lower limbs and trunk
In order to stand up, individuals with post-stroke hemiparesis often showed a lack of coordination between hip and knee displacements and hence, completed knee extension at the end of STS while their hips were still extending . Unlike healthy subjects, who presented an almost neutral trunk position in the frontal plane, individual post-stroke showed trunk tilt towards the less affected side during STS when they rose from a chair using spontaneous or symmetrical foot positions . This trunk displacement was observed, even before seat-off and was estimated at 12.1° ± 6.1 compared to 2.4° in healthy individuals . Nevertheless, placing the affected foot behind the other, corrected the asymmetrical tilt of trunk . When asked to do an anterior trunk flexion while sitting, individuals post-stroke had less CoP displacement compared to healthy subjects, despite similar trunk movement amplitude . To explain these results, authors suggested that the anterior trunk flexion was executed more by flexing the upper trunk while a small anterior tilt of pelvis occurred .
3.2
Muscular activation changes after stroke
During the chronic phase of stroke, an impairment of lower limb muscle activity was observed in the paretic lower limb when compared with the less affected side especially for tibialis anterior, soleus and quadriceps . However, when the less affected foot was placed in an extended position, the activity was improved by 29% for tibialis anterior and by 34% for the quadriceps. The same improvement was observed when the less affected foot was placed in an elevated position, with 51% and 41% for tibialis anterior and quadriceps respectively . These two-foot positions therefore seem to be more advantageous in normalizing muscle activation on the paretic limb.
Chronic post-stroke hemiparetic subjects were also unable to recruit their paretic lower limb muscles at the proper time to achieve STS . Thus, the moment when tibialis anterior became active was delayed as demontrted by a mean onset time of this muscle activity at 12.5% of the total STS duration for post-stroke subjects while it was at 5.8% for healthy subjects. An almost simultaneous activation of quadriceps, hamstrings and soleus muscles was also observed . In contrast with healthy subjects, the soleus muscle was activated before seat-off, which could be related to the spasticity and weakness of this muscle .
In the less affected limb, change in muscular activation was also observed with higher EMG activity of tibialis anterior, quadriceps and soleus muscles on one hand, and earlier hamstring activation on the other hand . These changes occurred to possibly compensate for the weakness of the paretic lower limb and might be related to the increased WB on the less affected side.
3.3
Postural control
After stroke, CoM movement deviated laterally towards the less affected side by 78% more before seat-off and 50% more after seat-off than in healthy subjects . This was explained by greater trunk movements in the mediolateral direction in comparison to healthy subjects . Duclos et al. corroborated this explanation by showing an improvement in trunk deviation, as well as CoP displacement, when the affected foot was placed behind. To evaluate postural control of post-stroke subjects, Duclos et al. calculated the CoP time-to-contact (TtC) in the mediolateral plan, which represents the maximal time before CoP reaches the limit of the base of support. This index was shorter for hemiparetic subjects in comparison to healthy ones, indicating poor dynamic stability during STS, and was mainly related to motor impairment of the paretic lower limb (evaluated by the Chedoke score) and to a lesser extent to strength of trunk muscles (assessed with a Biodex dynamometer) and level of spasticity . Along the same line, hemiparetic subjects who had experienced one or more falls had significantly increased CoP sway in both mediolateral and anteroposterior directions when compared to those who had never fallen . To avoid this risk of falling, they have therefore adopted compensatory strategy such as exaggerating (3 cm more than healthy subjects) the anterior projection of CoM before rising . This strategy allowed closer position of CoM to CoP and might thus induce less anterior movement during the rising phase and better postural stability.
3.4
Weight bearing distribution
Eng and Chu examined the test-retest reliability of the weight-bearing (WB) measures in individuals who have had stroke. They showed that WB measures are reliable over separate days for both the paretic and non-paretic limbs and for different postures and directions. Spontaneously, post-stroke hemiparetic individuals put less weight on the affected limb during STS . The mean loading on the paretic limb was 37% of body weight according to Engardt . A similar value was observed by Brunt et al. , with 16% excess on the less affected limb. However, they were able to perform more symmetrically with the use of auditory or visual feedback or by modifying the foot positions . It is not understood why they spontaneously adopt this asymmetrical pattern but it was suggested that this could represent the best compromise in terms of decreasing the level of muscle effort, ensuring safety and being effective in performing STS . Interestingly, this asymmetric tendency was observed even before seat-off, when subjects with hemiparesis still had their thighs in contact with the chair . With regard to foot positions, WB under the paretic foot decreased when the less affected one was placed backward . In contrast, when the paretic foot was placed behind, subjects with hemiparesis were forced to improve their WB by 14% . Brunt et al. reported similar values, 8% and 10% under extended and elevated less affected foot conditions respectively, which suggest that these conditions place the paretic limb in a better position to generate greater vertical force or to bear more weight on the paretic side.
The degree of awareness about WB asymmetry of hemiparetic subjects is still an unresolved issue. Engardt and Olsson reported that association between post-stroke hemiparetic subjects’ estimation of WB distribution on a visual analogue scale and their actual WB distribution was low. Similarly, Brière et al. concluded that subjects with chronic hemiparesis were less accurate in their perception of WB than healthy individuals and they overestimated the weight under the paretic foot. As a plausible explanation, authors suggested that these individuals rated their perceived effort distribution instead of their WB. In a recent study, Brière et al. demonstrated similar bilateral efforts in a hemiparetic group with severe knee strength impairment, while their WB distribution was clearly asymmetrical. For those who had mild and moderate knee strength impairment, knee efforts and WB were similar revealing that the strategy adopted by the participants depended on the level of strength deficit. However, the same authors demonstrated that the intraclass correlation coefficient (ICC) between real distribution and perception scores was greater for WB than for level of effort, 0.358 and 0.061 respectively revealing that participants post-stroke were not able to judge their perception of effort at the knees.
Post-stroke individuals also have impaired perceptions of verticality, namely the visual vertical, the haptic (tactile) vertical and the postural vertical. These modality-related perceptions of verticality influence the WB in standing and might also be important in STS tasks mainly if the lesion involved the right hemisphere . Future studies will need to determine the influence of alterations of verticality perception on STS performance and execution.
Lastly, Lee et al. noted a correlation between asymmetric WB in STS and functional capacities of the post-stroke subjects. Those who bore less weight on their paretic limb obtained a poor score of mobility in the independence functional measure scale. This finding was supported by Cheng et al. , who considered the asymmetric WB distribution in STS as a fall mediator. In fact, the average loading on paretic limb was smaller in stroke fallers than non-fallers, 24% and 29% of body weight respectively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




