Abstract
Objective
To analyse contraceptive methods and the extent of screening for breast and cervical cancer in women with neuromuscular disease, compare these results with data and guidelines for the general population and determine the environmental and attitudinal barriers encountered.
Patients and methods
A retrospective, descriptive study in a population of female neuromuscular disease patients (aged 20 to 74) monitored at a clinical reference centre.
Results
Complete datasets were available for 49 patients. Seventy percent used contraception (hormonal contraception in most cases). Sixty-eight percent had undergone screening for cervical cancer at some time in the previous 3 years and 100% of the patients over 50 had undergone a mammography. Architectural accessibility and practical problems were the most common barriers to care and were more frequently encountered by wheelchair-bound, ventilated patients.
Conclusions
In general, the patients had good access to contraceptive care and cervical and breast cancer screening. However, specific measures may be useful for the most severely disabled patients.
Résumé
Objectif
Évaluer les pratiques contraceptives et la réalisation de frottis cervicovaginaux et de mammographies de femmes présentant une maladie neuromusculaire et le comparer aux données de la population générale et aux recommandations. Déterminer les obstacles éventuels (accessibilité, représentations concernant le handicap).
Patients et méthodes
Étude descriptive et rétrospective, réalisée par questionnaire auprès des femmes de 20 à 74 ans suivies par le centre de référence d’Angers.
Résultats
Les données complètes sont disponibles pour 49 femmes. Soixante-dix pour cent des femmes en activité génitale ont une contraception, majoritairement la pilule, 68 % ont un frottis de moins de trois ans ; 100 % des femmes de plus de 50 ans ont eu un dépistage par mammographie. Les problèmes matériels et d’accessibilités sont les principales barrières rencontrées et sont plus importants dans le sous-groupe des patientes dépendantes d’un fauteuil et ventilées.
Discussion
Le suivi gynécologique de ces patientes est très satisfaisant. Pour les patientes les plus dépendantes, les obstacles nécessitent peut-être une prise en charge spécifique.
1
English version
1.1
Introduction
Several studies have shown that women with physical disabilities have worse access to preventive healthcare (including blood pressure check-ups and gynaecological cancer screening ) than women without disabilities . An American study published in 1995 showed that only 23% of the women with functional limitations had had a cervical smear, compared with 41% of the women without limitations . For the performance of a mammography, these percentages were 13 and 44%, respectively. However, there was no significant difference between the two populations in terms of vaccination against influenza. In France, data on preventive healthcare for patients with physical disabilities are scarce. A French study in 2002 attempted to determine how general practitioners (GP) dealt with disabled patients ; it showed that 27% of GP reported screening disabled women for breast cancer less often than for the general population and that 29.5% reported rarely prescribing contraception to disabled women. The main reasons stated were lack of information on the various medical and social care organizations, limited time during the appointment, lack of coordination between the various medical professionals and communication problems between patients and doctors.
Neuromuscular diseases are responsible for physical disabilities and can result in functional limitations. In general, patients do not present cognitive deficiencies and genital and sexual problems are non-specific (unlike spinal cord-injured patients). Hence, this population is a good model to use when seeking to analyze barriers to accessing preventive healthcare (due either to architectural accessibility or negative perceptions of persons with disabilities, for example). These obstacles are notably found in the field of sexuality, at a time when the French legislation asserts “equality of opportunity”. Neuromuscular disease care networks also have specific organisational features; these patients are increasingly managed by clinical reference centres and thus, GP may find it more difficult to fulfil their coordinating role and suggest health prevention measures and screening procedures.
The aim of the present study was to:
- •
analyse practice with respect to contraception and breast and cervical cancer screening in a population of women with neuromuscular diseases being monitored in a reference centre;
- •
compare these patients with the general population.
A qualitative analysis of patient interviews also addressed the obstacles and facilitators associated with functional limitations.
1.2
Patients and methods
In the present study, we included all women between the ages of 20 and 74 years being monitored by the local neuromuscular network for a neuromuscular disease and who were free of cognitive impairments.
In all, 49 out of 52 women were included; one person was lost to follow-up, one refused to participate and one had cognitive difficulties that were incompatible with participation in the study.
Part of the medical information on each patient was collected from the reference centre’s records: date of birth, nature of the neuromuscular disease, level of personal independence. For each patient, the degree of independence was rated as follows:
- •
walking unaided;
- •
dependency on a wheelchair for outdoors trips;
- •
fully wheelchair-dependant with a requirement for daytime ventilatory assistance.
A study information sheet and a consent form were emailed to all patients. The questionnaire was first sent by post (so that the interviewees could familiarize themselves with the contents) and was subsequently filled out during a telephone or face-to-face interview.
The following information was collected:
- •
lifestyle (family situation, number of children, occupation, etc.);
- •
contraceptive methods used (if any);
- •
cervical cancer screening (date of the last cervical smear and date of the next scheduled cervical smear);
- •
breast cancer screening (clinical breast examination and [for women over 50] the date of the last mammography).
The practitioner who had performed each procedure was specified (i.e. a GP or a gynaecologist).
An open question addressed the patients’ feelings concerning their care and questioned them specifically about obstacles to and facilitators of gynaecological follow-up.
All data were entered using Microsoft Excel 2003.
Data on the performance of cervical smears were analysed for under-65 patients having had sexual relations and not having undergone a complete hysterectomy, which corresponds to the population for which the screening is recommended in France.
Likewise, data on the performance of a mammography were analysed for the population of women over 50, which again corresponds to the population for which this type of screening is recommended in France.
Means and standard deviations were calculated for quantitative variables.
1.3
Results
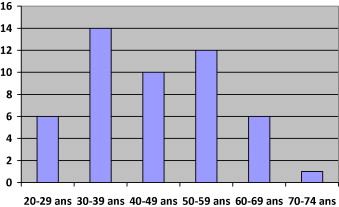
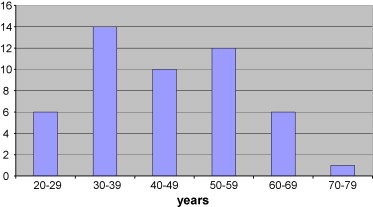
Forty-nine women were included. The mean age was 44.5 (SD: 13; minimum: 20; maximum: 74) and 30 women were under the age of 50 years old. Fig. 1 illustrates the age distribution. The population notably included nine subjects with proximal myopathy, ten with type 1 myotonic dystrophy (Steinert’s disease) and eight with childhood-onset spinal muscular atrophy.
Nineteen patients were able to walk unaided outdoors, 23 used a wheelchair and seven used a wheelchair full-time and also required daytime ventilation.
Thirty-four women lived with a partner and 23 had one or more children. One woman had adopted children because of her fear of transmitting her disease and another one had chosen not to have children for the same reason. Thirteen women were in employment.
1.3.1
Contraception
Thirteen women were menopaused, three were hoping to become pregnant, nine reported having never had sexual relations and five had undergone total or partial hysterectomy for fibroids. Nineteen women had a potential indication for contraception and 13 of these did actually use a contraceptive method (68%). The most frequently used method was the oestrogen-progesterone pill (53%), prescribed by a GP in four cases and by a gynaecologist in seven cases.
Two patients reported that their contraceptive method had been imposed on them. One patient stated that tubal ligation had been presented to her as the only means of contraception. Her refusal had prompted the administration of a contraceptive implant. One patient reported that contraception with leuprorelin injections was suggested to her after an intra-uterine device (IUD) was considered to be “inappropriate” for her disability.
Two patients relied on the use of male condoms as a contraceptive method. One patient had decided to have tubal implants, after a discussion with her gynaecologist. The remaining six patients (five of whom lived with a partner) did not use any contraceptive methods.
1.3.2
Cervical smears
A cervical smear (or Pap test) is indicated for women under the age of 65 having had sexual relations and not having undergone a total hysterectomy: this was the case for 35 patients. Three had never had a cervical smear and reported that it was a personal choice. The cervical smears had been performed in the previous 3 years for 24 of these 35 women (68%); 12 out of 14 ambulatory patients (86%), 11 out of 17 wheelchair-dependant patients (65%), and one of the four (25%) of the patients requiring daytime ventilation. The percentage differences between the subgroups were not statistically significant.
1.3.3
Clinical breast examination and mammography
Seventeen women had never had a clinical breast examination (35%), 11 had received this examination less than once a year (22%) and 21 had the examination annually (43%). Performance of an annual clinical breast examination was observed for eight of the 19 ambulatory women (42%), ten of the 23 wheelchair-dependant women (43%) and three of the seven women requiring ventilation (42%). The percentage differences between the subgroups were not statistically significant.
Eighteen women were aged 50 or over and all had had a mammography in the previous 2 years. Fifteen had undergone this mammography after receiving a national screening notification (83%). The remaining prescriptions were made by the gynaecologist (in one case) and the GP (in two cases). Thirteen of these 18 women were wheelchair-dependant.
1.3.4
The patient’s opinion of her gynaecological follow-up
Wheelchair-dependant women were more likely to report difficulties in obtaining regular gynaecological follow-up (14 out of 30) than ambulatory women (2 out of 19, p = 0.01). All mentioned practical problems (the lack of an appropriate examination table, in particular) and poor access to the doctor’s surgery. Three of these women also mentioned the requirement for a third person to help them undress and get onto the examination table. Five of the 16 women faced with these difficulties reported having abandoned their gynaecological follow-up as a result. Nine of these 16 women suggested that the inclusion of a gynaecological appointment in the reference centre’s multidisciplinary follow-up clinic would help.
Table 1 .
| Ambulatory | Wheelchair-dependant | Wheelchair- and ventilator-dependant | |
|---|---|---|---|
| Study population | 19 | 23 | 7 |
| Breast examination performed | 8 | 10 | 3 |
| Indication for cervical cancer screening | 14 | 17 | 4 |
| Cervical smear performed | 12 | 11 | 1 |
| Indication for breast cancer screening | 5 | 13 | 0 |
| Mammography performed | 5 | 13 | 0 |
| Reported difficulties in access to screening | 2 | 19 |
1.4
Discussion
General guidelines regarding contraception and breast and cervical cancer screening are relevant for this population of women with neuromuscular disease. As for any woman, sexual health and related matters should be discussed at least once with these disabled patients and contraception should be prescribed if the woman so wishes. This population is probably biased toward patients who are amenable to monitoring, since the latter were recruited at a multidisciplinary reference centre.
Our results concerning the prescription of contraceptive methods did not differ greatly from those for the general population. According to the “2005 Health Barometer” led by the French National Institute for Prevention and Health Education (INPES ), 71% of the women in France use a contraception method. Furthermore, the percentage of women not using contraception (despite living with a partner and not having expressed the wish to become pregnant) does not necessarily reflect specific problems.
Although our survey may have underestimated the use of male condoms as a means of contraception, the Pearl Index for this method is unsatisfactory anyway. As in the general population, the contraceptive pill remains the most frequent choice (57%) . None of our patients used IUD, despite the fact that the latter is the second most frequently used means of contraception in the general population in France; this agrees with North American data . Lastly, surgical methods are very infrequently used (7%), although this finding contrasts with the same American study in which surgical methods were reportedly more frequently used by disabled women . Our results appear to show that there is no great problem in gaining access to contraception. It is possible that the under-use of IUD is explained by practical difficulties in placing the patient in the usual gynaecological examination position. However, the prescription of “unusual” methods of contraception probably means that some negative stereotypes still persist within the medical profession.
In the population of women who should have undergone a regular cervical smear, 68% had indeed performed this procedure in the previous 3 years; this figure is similar to that found for general population in France’s “2005 Cancer Barometer” . Nevertheless, and even though the difference is not significant, there is a trend towards less screening as the level of disability increases. Again, this is probably due to poor access to doctors’ surgeries and healthcare management difficulties for disabled patients .
Regarding the clinical breast examination, there are very few literature data on the general population. A French study carried out in 2004 revealed that 10% of GP regularly examined their patients’ breasts . In our study, 34% of women had never had a clinical breast examination. There was no association between this percentage and the level of disability and so, this finding is probably due to the lack of systematic clinical breast examination in the general population.
For breast cancer screening, an evaluation of a mass screening programme organised in 2004 revealed a participation rate of 40,2%; this represents an increase over previous figures but is still below the 80% objective set by the fixed by France’s 2007 Cancer Plan. The coverage rates estimated in the INPES “2005 Cancer Barometer” are 70% for mass screening and 15 to 20% for individual screening , which is similar to our results. This very satisfactory result seems to confirm the hypothesis whereby these neuromuscular disease patients are, in general, very amenable to medical follow-up.
Our qualitative results for the patients’ opinion of their gynaecological follow-up consolidate the idea that (mainly practical) barriers persist and should help stimulate further debate on the problem of accessibility.
Our data are, on the whole, very similar to those of the French general population but differ from several French and North American studies on patients with a somewhat wider range of disabilities. The choice of a population affected by neuromuscular diseases and being monitored in a reference centre is a bias but leads to better results in the application of guidelines and can suggest interpretations and further research issues. The specific follow-up provided by a clinical reference centre does not reduce access to other care procedures (coordinated by the GP) and may even facilitate the patients’ overall compliance.
Specific measures should be offered to the most dependent patients; until such patients gain truly equal access to all health networks, these measures could include the provision of screening during multidisciplinary appointments. Lastly, it would be interesting to gather this type of data in populations of disabled women for whom systematic, multidisciplinary follow-up is not provided in France (in multiple sclerosis, for example) or those presenting associated cognitive impairments.
1.5
Conclusion
Architectural obstacles and (possibly) obstacles related to negative representations of disability persist but do not significantly impact access to contraception and gynaecological screening for women with neuromuscular diseases. These results have to be confirmed in a larger population and compared with other populations, in order to better define the patient groups which require specific measures in favour of equal opportunities.
2
Version française
Plusieurs études ont montré que des patientes atteintes d’un déficit moteur ont plus de difficulté à accéder à la médecine préventive qu’il s’agisse de la surveillance de la tension artérielle ou du dépistage des cancers gynécologiques . Celle réalisée en 1995 aux États-Unis montre que seulement 23 % des femmes ayant des limitations d’activité ont eu un frottis contre 41 % pour les femmes n’ayant pas de limitation. Ces chiffres sont respectivement de 13 et 44 % pour la réalisation d’une mammographie alors qu’on ne retrouve pas de différence significative entre les deux populations pour la vaccination contre la grippe. En France, les données sur l’accès à la médecine préventive de patients ayant un déficit moteur sont rares. Une étude réalisée en 2002 dans le sud de la France a essayé de déterminer la pratique des généralistes dans cette région vis-à-vis de patients en situation de handicap. Il en ressortait que sur le plan de la prévention 27 % des généralistes proposaient moins de dépistage de cancer du sein et 29,5 % proposaient rarement une contraception à une personne présentant un handicap. Les principales raisons évoquées dans ce manque de prise en charge sont le manque d’information sur les différents dispositifs médicosociaux, le manque de temps pour la consultation, le manque de coordination entre les différents intervenants et des problèmes de communication entre les patients et le médecin. Les maladies neuromusculaires sont parmi les pathologies responsables d’un déficit moteur pouvant être à l’origine de limitations importantes des activités. Elles ne sont généralement pas sources de déficiences cognitives et la prise en charge n’est pas déterminée par des problèmes génitosexuels spécifiques contrairement aux blessés médullaires. Elles constituent donc un bon modèle pour analyser les obstacles à la prévention liés au défaut d’accessibilité de l’architecture ou aux représentations négatives vis-à-vis des personnes handicapées, notamment dans le domaine de la sexualité, à l’heure où la loi affirme « l’égalité des chances ». Ces pathologies sont également spécifiques de par l’organisation de leur prise en charge multidisciplinaire. Celle-ci se fait de façon croissante autour de centres de référence et l’on peut se demander si cela crée des difficultés pour le médecin généraliste à trouver sa place en tant que coordonnateur du parcours de soins et à proposer les mesures préventives et le dépistage.
L’objectif de cette étude est donc d’analyser les pratiques de contraception et de dépistage des cancers du col utérin et du sein chez une population de femmes suivies pour une pathologie neuromusculaire dans un centre de référence et de les comparer à la population générale. Elle analysera aussi auprès des patientes les obstacles et les éléments facilitateurs à cette prise en charge, notamment en lien avec les limitations d’activité.
2.1
Patients et méthodes
L’étude concerne toutes les femmes âgées de 20 à 74 ans, ayant été suivies par le réseau neuromusculaire du CHU d’Angers depuis son ouverture en 2003, quelque soit la pathologie neuromusculaire, sans déficit cognitif majeur associé. Au total, 49 des 52 femmes suivies ont été inclues dans l’étude, une n’a pas pu être contactée, une n’a pas souhaité répondre et une présentait des troubles cognitifs incompatibles avec la passation du questionnaire.
Certaines données ont été recueillies à partir des dossiers standardisés du centre de référence.
Les données démographiques (date de naissance) et diagnostiques (nature de la maladie neuromusculaire) ont été recueillies dans le dossier. Le niveau d’autonomie des patients a été catégorisé en : marche autonome, utilisation d’un fauteuil roulant pour tous les déplacements extérieurs, utilisation d’un fauteuil roulant et ventilation assistée diurne.
Un courrier d’information et une demande de consentement ont été adressés à toutes les patientes. Un questionnaire a été adressé pour lecture préalable par la poste, puis rempli au cours d’un entretien téléphonique ou en face à face lors d’une consultation.
Les informations recueillies concernent :
- •
le mode de vie (situation familiale, nombre d’enfants, activité professionnelles) ;
- •
les pratiques contraceptives (mode de contraception utilisé) ;
- •
le dépistage du cancer du col utérin (date du dernier frottis, date prévue ou non du prochain) ;
- •
le dépistage du cancer du sein (palpation de seins et pour les femmes de plus de 50 ans date de la dernière mammographie).
Pour l’ensemble de ces examens, le praticien qui les a réalisé a été identifié (médecin traitant ou gynécologue).
Une question ouverte explore le ressenti des patientes concernant leur suivi et les interroge sur les obstacles, et les éléments facilitateurs de leur suivi gynécologique.
Traitement des données.
Toutes les données ont été saisies sous excel.
Pour la réalisation des frottis cervicovaginaux, les résultats ont été analysés pour la population des patientes de moins de 65 ans, ayant déjà eu des rapports sexuels et n’ayant pas subi d’hystérectomie complète qui correspond à la population pour laquelle cet acte de dépistage est recommandé.
Pour la réalisation de la mammographie, les résultats ont été analysés pour la population de femmes de 50 ans et plus qui correspond à la population pour laquelle cet acte de dépistage est recommandé.
Les moyennes et écarts-types ont été calculés pour les variables quantitatives.
2.2
Résultats
Il s’agit d’une population de 49 femmes d’âge moyen de 44,59 (écart-type : 13,17 ; extremes : 20–74) ; 30 femmes ont moins de 50 ans. La pyramide des âges est donnée sur la Fig. 1 . La population comprend neuf myopathies des ceintures, dix dystrophies musculaires de types 1 (myotonie de Steinert), huit amyotrophies spinales infantiles.