Complications Related to the Use of Thoracic Pedicle Screw Instrumentation
Louis G. Jenis
INTRODUCTION
The use of thoracic spinal instrumentation has evolved significantly over the last several decades with the advent of new technologies and better understanding of the anatomical and biomechanical characteristics of this unique segment of the spine. Harrington is often credited with initial development of instrumentation that was applied to the thoracic spine to treat deformity (1). The concept of nonsegmental fixation with Harrington rods or attachment and application of a force at opposite ends of a deformity without any additional fixation to intervening posterior elements was popularized and applied to the management of idiopathic scoliosis. Luque later contributed to the conceptual development of attachment of implants to several contiguous spinal levels, referred to as segmental fixation (2,3). Advantages of this technique over nonsegmental fixation included increased purchase of the posterior elements via multiple sublaminar wires fixed to Harrington longitudinal rods. This allowed for greater application of vector forces for deformity correction and stabilization, although the technique carried an increased risk of neurologic risk secondary to sublaminar passage of wires into the spinal canal (4). In order to limit the risk of canal intrusion, Cotrel et al. expanded upon the technology of segmental spinal fixation with the use of laminar or pedicle hooks attached to longitudinal rods (5). A biomechanical limitation of segmental fixation techniques applied to the spine with the aforementioned techniques is the application of forces to the posterior column of the spine only. In addition, insertion of hooks or sublaminar wires into the spinal canal carries an inherent risk of neurologic injury (4,6,7,8).
Transpedicular fixation in the lumbar and thoracic spine carries the biomechanical advantage of providing three-column fixation. Longitudinal pull-out strength has been shown to be significantly greater than pedicle or laminar hook fixation, lending credence to the applicability of these devices to deformity situations (9). Thoracic pedicle screw instrumentation has been popularized with development of devices specifically devised for the anatomical variations in this area, and it has been applied to coronal and sagittal plane deformities, and traumatic and pathologic conditions in adult, adolescent, and pediatric populations. However, insertion of fixation hardware into the pedicle is challenging, based on anatomy and surrounding vital structures in the nondeformed and deformed spine; to most surgeons, this can be an intimidating procedure, especially in the thoracic spine. Clinical success is related to appropriate use of pedicle screw instrumentation, and indications must be considered. The procedure of intrapedicular insertion of a screw is technically demanding and, although the reported complication rates are low, the consequences of malpositioning may be devastating.
Complications relating to the use of posterior thoracic instrumentation can be classified by the time of occurrence and etiology. Intraoperative complications can be considered to result from malpositioning or acute loss of fixation, early postoperative failure may be related to loss of correction, and delayed complications may relate to hardware fatigue or adjacent segment degeneration.
The purpose of this chapter will be to discuss the relevant anatomy related to posterior thoracic pedicle screw instrumentation and potential complications. Discussion will also include techniques for identification and management of complications.
PERTINENT ANATOMY
The anatomy of the thoracic should be considered in three distinct areas, including the upper thoracic (T1-T3), middle thoracic (T4-T9), and the lower thoracic (T10-T12). Each region is consistent in terms of basic spinal structure, although the main distinction lies within the anatomy of the pedicle. The pedicle arises from the posterior superior aspect of the vertebral body and tends to an anteromedial inclination (10). The most medial deviation is in the upper thoracic area and becomes more aligned in a true sagittal plane caudally and even may direct slightly laterally in some individuals (11) (Fig. 11.1). The lateral projection of pedicle is nearly 20 to 25 degrees from the vertebral body and remains similar throughout the upper and lower thoracic spine (12).
The morphology of the thoracic pedicle has been extensively studied in cadaveric and radiographic evaluations. The height of each thoracic pedicle is large and does not represent a limitation to intrapedicular instrumentation. The pedicle height is greatest in the lower thoracic spine (12.0 to 20.0 mm) and decreases cephalad (7.0 to 14.5 mm) (13,14). The transverse diameter or width serves as the dimension that is most critical for screw placement. Again, the largest transverse diameter is found in the lower thoracic region (6.3 to 7.8 mm) and is even greater than in the upper lumbar spine (12,14). The middle thoracic region represents the narrowest transverse diameter and gradually increases in the upper thoracic spine. The pedicle wall throughout the thoracic spine is thicker medially than laterally and may be one of the contributing anatomical variations of this region that leads to a high incidence of lateral pedicle perforation (15).
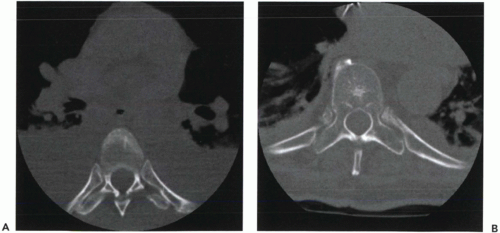 Figure 11.1 A. Axial CT of T4 vertebra. B. Axial CT of T11 vertebra. Note the pedicle width and angulation at each level. |
The anatomical relationship of the pedicle to surrounding structures is important to appreciate, given the potential consequences of a malpositioned pedicle screw. Vaccaro et al. evaluated in a human cadaveric study the placement of pedicle screws from T4 to T12 in the absence of radiographic assistance (16). Ninety pedicle screws were inserted, and 37 were noted to have perforated the pedicle wall (21 perforated medially and 16 laterally). Medial to the pedicle is the spinal canal, which in the thoracic spine is narrower than at other spinal levels. In the nondeformed spinal canal, there are 1 to 2 mm of epidural space between the neural elements and the pedicle wall (17). Medial protrusion places these structures at risk of injury. In close proximity to the anterior vertebral body lies the pleural cavity or retroperitoneal space, depending on the level of the spine considered. Major structures that are in close vicinity include the great vessels, azygos vein, pleura, and lungs, among others. Lateral to the pedicle and vertebral body lie the radicular paired vessels and pleural cavity.
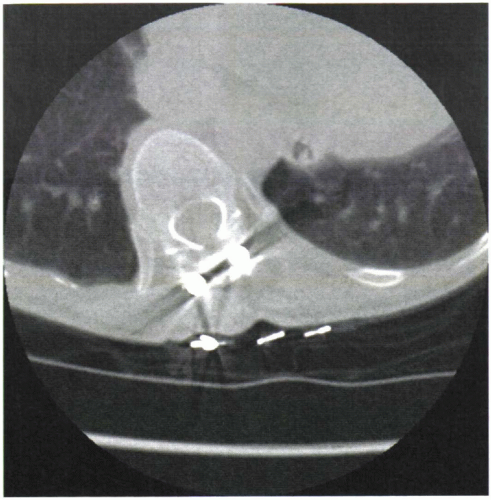
In scoliotic deformity, especially with significant apical vertebral body rotation, these relationships may be altered. The vertebral body translates anteriorly along the concavity of the curvature, while the convexity translates posteriorly. The pedicle axis along the convexity of the deformity will then orient along a more vertical trajectory, and any excess of medial angulation may place the spinal canal at risk (17). The pedicles along the concavity will require a more horizontal trajectory for safe placement and may place structures that were normally situated more anteriorly now at greater risk with malpositioning (Fig. 11.2).
COMPLICATIONS RELATED TO SCREW MALPOSITIONING
Superficial landmarks on the posterior elements may identify the entrance to pedicle; this knowledge becomes critical when attempting to insert intrapedicular devices in a safe and confident manner. Numerous clinical studies have reported on the complication rates related to the insertion of transpedicular fixation devices. Most data that have been reported in the literature surround the placement of pedicle screws within the lumbar spine. Jutte and Castelein retrospectively evaluated placement of screws in 105 consecutive patients and reported an overall 54% incidence of complications, with 6.5% related to screw malpositioning (18). In a large series of 875 patients with 4,790 screw placements, Lonstein et al. reported that 94.9% of the devices were placed within the pedicle and the 2.4% complication rate directly related to the hardware (19). They described a very low (1.0%) risk of nerve root irritation secondary to screw malpositioning; however, this study had very few procedures performed in the thoracic spine.
Belmont et al. compared thoracic screw placement accuracy in 407 patients and 399 screws with and without coronal plane deformity (20,21). Accurate positioning was confirmed in 98% and 99% of pedicles with and without associated deformity, respectively. Kulklo et al. performed a retrospective review of 20 patients with large-magnitude (greater than 90-degree) coronal plane deformity with postoperative computed tomography (22). They reported 96.3% accurate intrapedicular positioning from 354 screws and 0.57% of screws requiring removal for asymptomatic medial pedicle perforation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree