Complications of Thermal Capsulorrhaphy
Charles L. Getz
Matthew L. Ramsey
David Glaser
Gerald R. Williams Jr.
INTRODUCTION
Thermal energy has been used in the management of glenohumeral instability to modify the structure of collagen. Applying the energy with a small probe makes thermal capsulorrhaphy a relatively easy technique to add to a shoulder arthroscopist’s repertoire. In part, the ease of thermal capsulorrhaphy has resulted in its widespread use. However, application of heat in shoulder surgery has raised concerns about the potential complications that may occur. Risk to the axillary nerve, stiffness, capsular necrosis, and chondral injury have been reported as the major complications of thermal capsulorrhaphy. The following chapter will review the basic science of thermal modification of tissue, the indications and results for its use in shoulder surgery, and the major complications associated with thermal capsulorrhaphy.
BASIC SCIENCE
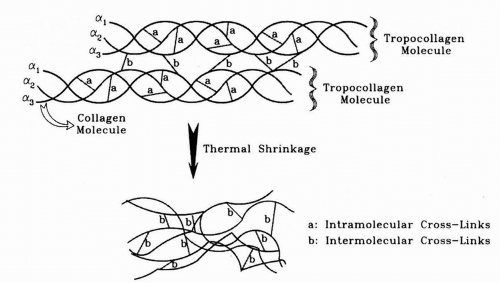
The most common structural protein contained within ligaments is type I collagen. Type I collagen is comprised of a triple-helix tropocollagen molecule composed of three polypeptide chains, each with unique repeating triple amino acid sequences (1,2). The individual polypeptide chains that combine to form the triple helix are bound together by crosslinking. Additional crosslinks between separate triple-helix tropocollagen molecules also occur. The crosslinking within and between the tropocollagen molecules is responsible for the tensile properties of collagen and maintains the highly organized structure.
When tissue containing type I collagen is heated to a temperatures above 65°C, the crosslinked bonds that stabilize the structures are dissolved (Fig.15-1) (1,2). The “melting” of collagen transforms the previously organized structure into a gel by both uncoiling the triple helices and disrupting the crosslinks between the tropocollagen molecules. As the tissue cools, the individual chains are free to form new crosslinks, resulting in a less organized, smaller protein. Over time, the tissue is remodeled to a more normal state.
The ability to shrink collagen fibers has allowed thermal energy to be used as a possible tool to decrease the overall length of the individual capsular regions and the overall volume of the glenohumeral joint. Luke et al. were able to show that thermal energy, when applied to cadeveric specimens, reduced capsular volume but not to the same extent that can be achieved by open shift techniques (3). In a series of articles, Tibone, Lee, and colleagues demonstrated reduced glenohumeral translation in cadaveric shoulders following thermal shrinkage (4, 5, 6, 7, 8, 9).
Thermal modification of type I collagen not only results in physical changes, but also in mechanical and biologic changes as well. The mechanical properties of strength and stiffness are both decreased as a result of thermal capsulorrhaphy.
The decreases in strength and stiffness are directly proportional to the length change that has occurred during heat application (10, 11, 12). Following the thermal injury, the treated tissue must then undergo protracted tissue remodeling, requiring up to 3 months (in a rabbit model) before normal mechanical characteristics return (13). The biologic impact of thermal injury is primarily related to the effect of heat on cells within the capsular tissue. Cell death has been reported to occur at temperatures of greater than 45°C (14,15). Therefore, in tissue that has been thermally modified (heated to at least 65°C), cell death has certainly occurred and probably extends to a zone of injury adjacent to but not directly under the heat probe.
The decreases in strength and stiffness are directly proportional to the length change that has occurred during heat application (10, 11, 12). Following the thermal injury, the treated tissue must then undergo protracted tissue remodeling, requiring up to 3 months (in a rabbit model) before normal mechanical characteristics return (13). The biologic impact of thermal injury is primarily related to the effect of heat on cells within the capsular tissue. Cell death has been reported to occur at temperatures of greater than 45°C (14,15). Therefore, in tissue that has been thermally modified (heated to at least 65°C), cell death has certainly occurred and probably extends to a zone of injury adjacent to but not directly under the heat probe.
INDICATIONS AND RESULTS
Traumatic Unidirectional
Instability can be defined as increased rotational or translational motion associated with pain and disability. A common type of glenohumeral instability is unidirectional anterior instability. This instability pattern often results following a frank anterior dislocation of the shoulder and is secondary to an avulsion of the anterior glenoid rim (bony Bankart lesion), labrum (classic Bankart lesion), or humeral insertion of the anterior-inferior glenohumeral ligament (HAGL). Intracapsular stretch injury also contributes to traumatic unidirectional instability in patients who have had multiple dislocations or who have sustained an anterior dislocation in the presence of pre-existing multidirectional laxity. Therefore, surgery to address unidirectional anterior instability is aimed at restoring the premorbid anatomy (i.e., reattaching the capsule or labrum and addressing any pathologic capsular laxity). Open repair of the injured anterior shoulder restraints has a long proven track record with recurrence rates of less then 10% (16, 17, 18, 19). Arthroscopic repair of the same structures has continued to improve and results are now approaching those obtained in open reconstruction, especially when capsular stretch and capsular avulsion have been addressed. Gartsman has reported excellent results (92% success rate) for 53 patients with anterior instability arthroscopically treated with thermal capsulorrhaphy added to arthroscopic labral repair if increased translation exists after the labrum is repaired (20).
Atraumatic and Microtraumatic Instability
Atraumatic and microtraumatic instability may develop with repetitive use of the arm over months to years, not in a single event. Various regions of the joint capsule become attenuated and allow increased motion of the glenohumeral joint. The labrum, glenoid, and ligamentous insertions are typically normal. Neer (21) described an inferior capsular shift procedure that reduced the over all volume of the shoulder in patients with multidirectional instability patterns; his results were greater then 90% successful. Arthroscopic plication of the capsule to address capsular redundancy has also been described (22). All of these surgical techniques aim to restore normal function to the shoulder by reducing the length of the ligaments of the shoulder and therefore reducing the overall capsular volume.
Arthroscopic thermal modification of the collagen-rich glenohumeral capsule has also been described as a method of shortening capsular ligaments and reducing capsular volume (3). The ability to watch the tissues as they shorten provides the surgeon tactile feedback to assess the overall amount of volume contraction that is taking place. The procedure has been applied to a wide range of instability patterns with varied success.
Anterior Atraumatic Instability
Jobe (23) described an open anterior capsular reconstruction for primarily overhead athletes with anterior, microtraumatic
instability in 1991. An open subcapularis sparing approach with plication of the anterior inferior glenohumeral ligament returned 17 of 25 overhand athletes to a high level of play (mainly professional baseball players) and resulted in 92% good or excellent results. In a similar group of patients, Levitz et al. (24) reported on the use of thermal capsulorrhaphy in 2001. Surgery was performed using arthroscopy with and without thermal capsulorrhaphy in this group of throwing athletes with presumed recurrent anterior microtraumatic subluxation. Patients with partial rotator cuff tears and/or superior labral tears were treated with arthroscopic debridement of the partial rotator cuff tear and debridement or repair of superior labral pathology. At an average of 30 months follow-up, a significant difference was noted between those patients who underwent thermal treatment and those who did not. In all, 90% of patients treated by thermal capsulorrhaphy were still throwing at follow-up as compared to 60% in the nonthermally treated group.
instability in 1991. An open subcapularis sparing approach with plication of the anterior inferior glenohumeral ligament returned 17 of 25 overhand athletes to a high level of play (mainly professional baseball players) and resulted in 92% good or excellent results. In a similar group of patients, Levitz et al. (24) reported on the use of thermal capsulorrhaphy in 2001. Surgery was performed using arthroscopy with and without thermal capsulorrhaphy in this group of throwing athletes with presumed recurrent anterior microtraumatic subluxation. Patients with partial rotator cuff tears and/or superior labral tears were treated with arthroscopic debridement of the partial rotator cuff tear and debridement or repair of superior labral pathology. At an average of 30 months follow-up, a significant difference was noted between those patients who underwent thermal treatment and those who did not. In all, 90% of patients treated by thermal capsulorrhaphy were still throwing at follow-up as compared to 60% in the nonthermally treated group.
Enad et al. (25,26) have recently reported less favorable results for overhand athletes treated with selective thermal shrinkage. In one series, only 10 of 20 patients returned to their previous level of play (25). In the second series, 17% of patients required an open stabilization procedure following thermal capsulorrhaphy for continued instability (26).
Multidirectional Instability
As previously noted, Neer (21) has reported considerable success with an open shift to address multidirectional instability. Other surgeons have also noted success with open capsular shift techniques (27,28). Success with thermal capsulorrhaphy in the management of multidirectional instability has been quite variable. Reports by Fanton, Thabit, and Savoie have been favorable (29, 30, 31). Gartsman combined thermal capsulorrhaphy with other techniques to successfully treat patients with bidirectional instability (32). However, the literature also has reports of less favorable results from Anderson, Fitzgerald, Levy, Frostick, Noonan, Miniaci, and D’Alessandro (33, 34, 35, 36, 37, 38, 39).
In an attempt to define patients that may be more likely to have early recurrent instability after undergoing thermal capsulorrhaphy, Anderson et al. (40) reviewed the results of 106 patients all with at least 6 months of follow-up. The study found a significantly higher failure rate among patients with a history of more than two dislocations or prior surgery. Other factors reviewed such as contact sports, multidirectional instability, and other procedures performed concurrent with the thermal capsulorrhaphy did not result in significantly higher rates of failure.
COMPLICATIONS
Axillary Nerve Injury
Several authors have reported injury to the axillary nerve after thermal shrinkage. Greis (41) reported a case series of four patients with axillary nerve injury. Two had pure sensory disturbances, whereas the others were mixed injuries. Miniaci (38) reported four patients with transient sensory disturbances in a series of 19 patients. One of the patients also had deltoid weakness. The neurologic symptoms were completely resolved by 9 months in all patients. D’allessandro (39) reported 12 patients (out of 84) who experienced temporary axillary nerve dysesthesias. Fortunately, all symptoms related to nerve irritation resolved by 3 months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree