Complications of Surgery to the Acromioclavicular and Sternoclavicular Joints
Jonathan P. Braman
Evan L. Flatow
The preponderance of shoulder pathology involves the glenohumeral joint and the subacromial articulation. However, the acromioclavicular (AC) and the sternoclavicular (SC) joints also provide sources of disability from degenerative and traumatic conditions. These conditions often coincide with pathology found in other regions of the shoulder, and consequently their treatment is often simultaneously performed with other shoulder procedures. Even so, there are complications associated with surgery of the joints on the ends of the clavicle in isolation of other concomitant shoulder pathology.
AC JOINT ANATOMY
The AC joint bridges the clavicle and the acromion of the scapula with a diarthrodial joint covered with fibrocartilage. A meniscoid intra-articular cartilage in the joint degenerates over time and its function is not well understood. The inclination of this joint varies from near vertical to an approximately 50-degree inclination downward medially (1,2).
Bony congruency is inadequate for intrinsic stability, so ligamentous and capsular structures provide support. The coracoclavicular ligaments (trapezoid laterally and conoid medially) prevent caudad migration of the shoulder in relation to the clavicle and deformation with axial compression. Acromioclavicular ligaments provide stability in the anteroposterior direction (2, 3, 4). Additional stability is added by the blending of the trapezial and deltoid fascia on the surface of the clavicle and joint capsule (5).
AC JOINT PATHOLOGY AND SURGICAL TREATMENT
AC joint disorders manifest as instability of the joint or pain in the location of the joint. Instability issues are usually related to traumatic insults, such as a direct load on the point of the shoulder. Painful conditions, on the other hand, can be the result of primary osteoarthritis, posttraumatic osteoarthritis, or distal clavicle osteolysis.
COMPLICATIONS OF AC JOINT STABILIZATION
Surgical indications for instability of the clavicle have been debated and many techniques of stabilization have been
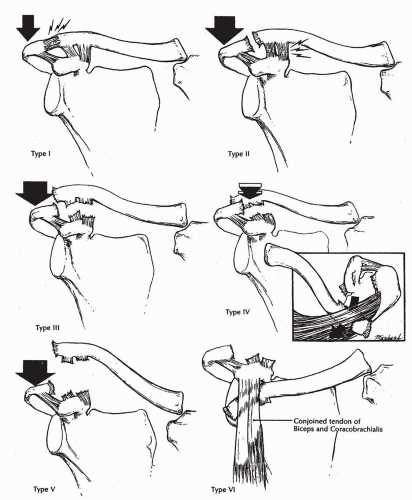
described (6, 7, 8, 9, 10, 11, 12, 13, 14). Rockwood’s six-type classification is by far the most widely used (Fig. 6-1) (15). A thorough review of the indications for surgery on the unstable acromioclavicular articulation is outside the scope of this chapter; however, symptomatic instability of the clavicle, especially those in the posterior direction (Type IV) or with severe displacement (Types V and VI) can require surgical stabilization (Fig. 6-2). Whichever surgery is performed on the AC joint to restore stability, several recognized complications can occur (16,17). These complications take many forms, but most common are loss of reduction, continued symptoms, new-onset arthritis, and migration of hardware.
described (6, 7, 8, 9, 10, 11, 12, 13, 14). Rockwood’s six-type classification is by far the most widely used (Fig. 6-1) (15). A thorough review of the indications for surgery on the unstable acromioclavicular articulation is outside the scope of this chapter; however, symptomatic instability of the clavicle, especially those in the posterior direction (Type IV) or with severe displacement (Types V and VI) can require surgical stabilization (Fig. 6-2). Whichever surgery is performed on the AC joint to restore stability, several recognized complications can occur (16,17). These complications take many forms, but most common are loss of reduction, continued symptoms, new-onset arthritis, and migration of hardware.
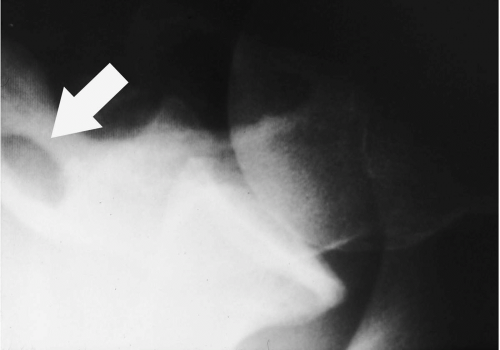
Loss of reduction has been reported to be as high as 44% following AC joint reconstruction (11). Reoccurrence can occur regardless of which technique is used (Fig. 6-3). Many different methods have been attempted to reduce this rate. Transarticular AC pinning has been shown to have high rates of loss of reduction and dangerous pin migration (Fig. 6-4) (8,18, 19, 20, 21, 22). Taft et al. (8) had 4 of 26 patients with loss of reduction and six patients with AC joint arthritis at an average follow-up of 9.5 years. Two of the six with arthritis required distal clavicle excision. In Larsen’s series (20), they noted 9 out of 39 patients had at least slight pain, two of whom required distal clavicle excision. Three patients had poor range of motion.
Bosworth screw fixation, first described by Bosworth in 1949 (23), is a method of screw fixation between the clavicle and the coracoid designed to reduce and hold the clavicle in anatomic position. A variation on this device was evaluated by Tsou (10) using a percutaneous cannulated
device to facilitate insertion. In Tsou’s series, 5 of 53 patients had postoperative AC joint pain, 15 of 53 patients had loss of reduction, and the technique required staged removal. He reported an overall 32% “technical complication” rate (17 of 53 patients). Taft et al. (8) reported 11 of 26 coracoclavicular screw patients with loss of reduction in his series.
device to facilitate insertion. In Tsou’s series, 5 of 53 patients had postoperative AC joint pain, 15 of 53 patients had loss of reduction, and the technique required staged removal. He reported an overall 32% “technical complication” rate (17 of 53 patients). Taft et al. (8) reported 11 of 26 coracoclavicular screw patients with loss of reduction in his series.
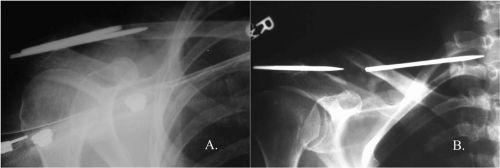
 Figure 6-2 Posterior (type IV) dislocations of the acromioclavicular joint can be symptomatic and require stabilization. |
 Figure 6-3 Recurrence of clinical deformity is a frequently seen complication after stabilization procedures regardless of which surgical technique is used. |
Ferris et al. (9) reported on the results of 20 coracoid transfers in their series. This is a dynamic transfer in which the coracoid with attached muscles is transferred to the clavicle to act as a clavicle depressor. A variation of this transfer was originally described by Vargas in 1942 (24). Ferris et al. (9) had 9 of 20 patients with residual pain, two superficial infections, two frozen shoulders requiring manipulation, and a 100% clinical “deformity” at the AC joint, which the authors attributed to a combination of “soft-tissue swelling and residual subluxation of the acromioclavicular joint.” Additionally, one patient reported subjective weakness. Lastly, their procedure required a second surgery to remove the AC staple approximately 6 weeks after the index procedure.
Increasing the strength of the stabilizing device also failed to reduce the rate of loss of fixation. Use of a hook plate as reported by Sim (13) failed to prevent subluxation (4 of 20 displaced) while necessitating a second operation with significant dissection to remove the plate and allow resumption of normal activities with the shoulder. They also reported a high infection rate.
By far the most common reconstructions for AC separations are variations of the Weaver-Dunn procedure. They originally described their technique for reconstruction of the coracoclavicular ligaments in 1972 (7). This procedure uses the coracoacromial ligament as a prosthetic to restore clavicular alignment. They noted 4 of 15 patients with at least partial recurrence of the deformity, one of which required reoperation. Attempts to reduce the recurrence rate by augmenting ligamentous reconstruction with fascial loops, nonbiodegradable suture, or tape have still failed to eliminate recurrence of the deformity completely. Modification of their technique by Stam and Dawson (11) using a Dacron ligament showed similar results with 9 of 20 nonanatomic reductions and 8/20 patients with at least occasional pain. Weinstein et al. (25) reported on a series using nonabsorbable suture and had 9 of 44 patients with loss of reduction. Morrison and Lemos (12) reported much better results at 2 years follow-up with slightly different tunnel placement in the clavicle and a different artificial graft. In their series, 2 of 14 patients had poor results acutely; one was a frozen shoulder that responded well to manipulation and the other was a patient with rupture of his graft who did well with revision surgery. Loss of reduction, osteolysis, coracoid fracture, and reaction to synthetic materials have also been reported (Fig. 6-5).
Paavolainen et al. (26) combined a direct repair of the acromioclavicular and coracoclavicular ligaments with a AC joint transfixion screw. Their results demonstrated subluxation or dislocation in 7 of 36 patients. Additionally, they had 12 of 36 patients who showed distal clavicular osteolysis in addition to four who showed AC arthosis. Consequently, some surgeons prefer routine resection of the distal clavicle at the time of repair of AC dislocations to avoid the complication of later AC pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree