Complications of Surgery for Posterior/Multidirectional Instability
James D. O’Holleran
Russel F. Warren
INTRODUCTION
Posterior instability of the shoulder has been described since the early 19th century. Historically considered a rare problem, traumatic posterior dislocation has been reported to comprise less than 4% of all shoulder dislocations (1, 2, 3). However, posterior instability is becoming increasingly recognized as an important clinical entity, alone or in combination with a multidirectional component. In 1980, Neer and Foster (4) solidified our understanding of multidirectional instability (MDI) by distinguishing it from other unidirectional instabilities, as well as by introducing the concept of the inferior capsular shift to globally tension the capsule to recreate multidirectional stability. In addition, instability manifested as subluxation, as opposed to frank dislocation, has been recognized as a separate and much more common clinical entity.
Although the treatment of multidirectional or nontraumatic posterior instability is diagnostically and therapeutically challenging, mostpatients canbe successfully managed nonoperatively, with individually tailored strengthening and balancing of rotator cuff muscles and the scapular stabilizers. When such conservative treatment fails, anatomic restoration of the injured or insufficient structures can reliably relieve pain and restore function. Avariety of treatment alternatives exists, depending on the pathologic process involved.
A thorough review of the underlying pathoanatomy of posterior instability and MDI, leading to the rationale for surgical decision-making, is beyond the scope of this chapter. However, some mention of the basis for surgical reconstruction is warranted. Posterior instability can be classified in a variety of ways, either by degree (subluxation, dislocation, or locked dislocation), direction (uni-, bi-, or multidi-rectional), chronicity (acute or chronic), volition (involuntary or voluntary), or mechanism (traumatic or atraumatic). A thoughtful assessment of the direction and the degree of instability combined with an appreciation of the anatomic abnormalities, which are reflected by a combination of the above factors, will lead the surgeon to choose the proper type of surgical reconstruction.
Open techniques have been the historical standard for stabilization. Open posterior capsular shift, with or without posterior labral repair, and with or without infraspinatus augmentation, remains the mainstay of open treatment for posterior instability (1, 2, 3,5). For true MDI, capsular shift remains the gold standard, with the direction of the capsulorrhaphy determined by the side of greatest instability (1,4,6,6a). If the instability had a primarily anterior component, then selective inferior capsular shift performed through an anterior deltopectoral approach is preferred. For MDI associated with a primarily posterior component, an inferior capsular shift is performed through a posterior approach. For posterior instability associated with excessive glenoid retroversion, an opening wedge glenoid osteotomy, performed through a posterior approach, is advocated (7). In advanced and multiple-revision cases, humeral rotational osteotomy and glenohumeral fusion are salvage options (8,9).
Currently, arthroscopic techniques are being advocated to address these forms of instability, whether a posterior labral repair in a patient with an acute, traumatic posterior labral tear (the so-called reverse Bankart), or a global arthroscopic capsular placation/shift with a rotator interval closure for the patient with MDI. These techniques and their resultant complications will be addressed in another chapter, as well as complications of the anterior approach for a capsular shift.
It has been stated that the only way to prevent surgical complications is to avoid performing surgery (10). Complications represent a diagnostic and technical challenge, as the reason for the event may be difficult to ascertain, and the revision procedure usually requires restoring normal anatomy in the face of scarred tissue planes, previously placed anchors, and possibly glenohumeral arthrosis. Surgical reconstruction may fail because of errors made during the preoperative, intraoperative, or postoperative period (11). Preoperative errors occur in the process of patient evaluation and surgical decision-making, and include diagnostic errors and the failure to address a patient’s expectations for surgery and the resulting outcome. Intraoperative errors include technical pitfalls encountered during the posterior approach to the shoulder and complications involving bony procedures (hardware problems and glenoid fracture). Complications encountered in the postoperative setting include loss of motion with or without resulting arthrosis, recurrent instability or new-onset anterior instability, coracoid impingement syndrome, and bony fixation problems (malunion, nonunion, loss of fixation, osteonecrosis of the glenoid). For each of these complications, we evaluate their nature and incidence, assess the anatomical or technical reasons for them, provide pearls on how to avoid them, and suggest treatment options in their management.
PREOPERATIVE ERRORS
The history, physical examination, and radiographic evaluation provide the foundation for accurate surgical decision-making. Although most surgeons are comfortable and familiar with anterior instability, especially of an acute traumatic nature, many are less familiar with atraumatic multidirectional instability and isolated posterior instability. Fastidious attention to detail in the preoperative period will dramatically reduce complications encountered in the operative and postoperative periods.
Incorrect Diagnosis
When evaluating any complaint in the shoulder, a thorough history and physical examination form the foundation for an accurate diagnosis. One of the most common sources of unrecognized referred pain to the shoulder is the cervical spine (12). In addition, other shoulder problems including rotator cuff or superior labral pathology may be responsible for painful symptoms (13). For the most part, however, improper assessment of the degree, direction, and mechanism of instability is the most common diagnostic error, leading to a failure to appreciate the true type of instability. Improper diagnosis in turn leads to vague or incorrect physical therapy orders, and ultimately to improper surgical procedures. The literature documenting the failure of posterior instability and MDI surgery is sparse compared to that assessing failed anterior surgery, but a common thread runs throughout: missed diagnosis of either unidirectional instability or MDI is responsible for failure of surgical stabilization, with rates ranging from 21% to 68% (14, 15, 16, 17).
To avoid missing the correct diagnosis, the clinician must be thoughtful in taking the history, performing specific provocative maneuvers in the physical exam, and obtaining all necessary imaging. As noted previously, posterior instability can be classified in a variety of ways: by degree (subluxation, dislocation, or locked dislocation), mechanism (traumatic or atraumatic), chronicity (acute or chronic), direction (uni-, bi-, or multidirectional), or volition (involuntary or voluntary). A focused history will elucidate these factors and their relative contribution to the overall diagnosis.
The degree, mechanism, and chronicity of instability can often help to differentiate unidirectional from multidirectional instability. Frank dislocations that occur from a discernible acute traumatic event and require medical assistance for reduction are often associated with labral pathology and are usually unidirectional in nature. On the other hand, subtle perceptions of atraumatic subluxation that occur chronically often suggest multidirectional instability. The patient describes the shoulder as “loose” or “popping in and out,” labral pathology is less common, and nonphysiologic capsular laxity is often present.
The direction of instability is usually suggested by the history. Anterior instability is perceived when the shoulder is in the abducted, externally rotated position, such as the driver of a car reaching into the backseat for an item. Posterior instability is perceived when the arm is forward flexed, as when reaching in front of the body for something. Even more sensitive is when a posteriorly directed force is applied along the arm when in this position, such as at the beginning or end of a repetition in a bench press. Inferior instability, corresponding to a sulcus sign, is perceived when an inferiorly directed force is applied to the adducted arm, such as lifting a heavy suitcase.
Lastly, voluntary subluxation is a particularly important subset of patients to recognize. Wall and Warren (11) separate volitional instability into positional and muscular types, with the former experiencing instability only in certain arm positions, and the latter being able to cause subluxation with simple muscle contraction (Fig. 2-1). Neer
(18) carefully distinguishes between the patient who can cause instability and the patient who receives secondary gain from such behavior. Although Fuchs and Gerber (19) reported satisfactory intermediate-term results with posterior-inferior capsular shift in voluntary subluxators, several reports in the literature caution the clinician to avoid surgery in the volitional instability patient who has documented psychiatric issues, exhibits muscular instability, or receives secondary gain (11,14, 15, 16, 17, 18,20).
(18) carefully distinguishes between the patient who can cause instability and the patient who receives secondary gain from such behavior. Although Fuchs and Gerber (19) reported satisfactory intermediate-term results with posterior-inferior capsular shift in voluntary subluxators, several reports in the literature caution the clinician to avoid surgery in the volitional instability patient who has documented psychiatric issues, exhibits muscular instability, or receives secondary gain (11,14, 15, 16, 17, 18,20).
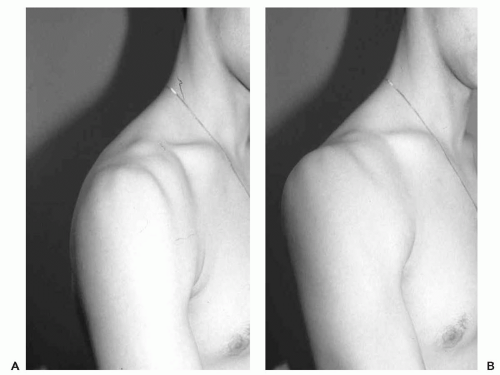 Figure 2-1 A patient at rest (A) and after muscle contraction (B), exhibiting voluntary muscular posterior subluxation. |
The physical exam should be thorough, including the cervical spine, the neurovascular assessment of the whole extremity, and the complete shoulder exam. Specific unidirectional instability signs include evocative tests of a patient’s subjective reaction to a maneuver, such as the apprehension and relocation signs, and clinician-derived objective measures of laxity, such as translation on load and shift testing. Positions similar to those mentioned in the history are recreated. Anterior instability is assessed with the arm in the abducted, externally rotated position. A subjective, uneasy feeling of instability or impending dislocation suggests a positive apprehension test. When a posteriorly directed force is applied to the humerus with the arm still in this position, the feeling of apprehension subsides, marking a positive relocation test. Anterior translation is documented by the load and shift test. The patient is placed supine to stabilize the scapula and the arm is positioned in abduction, neutral rotation, and forward flexion of approximately 30 degrees to match the plane of the scapula. An axial force is directed along the humerus and then the head is anteriorly translated.
Several variations on a grading scheme have been published; we use a 0 to 3+ grading system (21). Grade 0 indicates no increased translation over the opposite side; grade 1 indicates translation to the glenoid rim but not over; grade 2 indicates that the head can be dislocated over the glenoid rim but it spontaneously reduces; grade 3 indicates dislocation over the glenoid rim with no spontaneous reduction.
Posterior instability is assessed by placing the arm in the forward flexed position and applying a longitudinal force along the humerus, which effectively exerts a posteriorly directed force. A feeling of apprehension is again queried; however, it is far rarer to elicit the true apprehension of an impending dislocation as is seen anteriorly. Often the patient will experience pain, clicking, or vague discomfort. A posterior load and shift test is then performed to assess translation, with all factors similar to those described for anterior translation, but after axial loading, the humerus is shifted posteriorly. Grading is similar to the above.
Signs of MDI include generalized ligamentous laxity, pathologic translation anteriorly and/or posteriorly, and a positive sulcus sign (inferior translation). Although isolated anterior and posterior signs suggest unidirectional instability in that direction, the addition of a sulcus sign suggests more of a global problem. As will be discussed further, a positive sulcus sign indicates insufficiency in the rotator
interval. The sulcus sign is performed with the patient standing or seated and with the arm at the side. A longitudinal force is applied to the humerus by pulling on it such that the humerus is distracted from the acromion. The magnitude of the gap observed (and palpated), the so-called sulcus, is recorded. Grade 0 is minimal, grade 1 is less than 1 cm, grade 2 is 1 to 2 cm, and grade 3 is greater than 2 cm.
interval. The sulcus sign is performed with the patient standing or seated and with the arm at the side. A longitudinal force is applied to the humerus by pulling on it such that the humerus is distracted from the acromion. The magnitude of the gap observed (and palpated), the so-called sulcus, is recorded. Grade 0 is minimal, grade 1 is less than 1 cm, grade 2 is 1 to 2 cm, and grade 3 is greater than 2 cm.
A critical distinction to appreciate is that laxity does not equal instability. Laxity is a relative amount of humeral translation that it is asymptomatic and usually symmetrical when compared with the opposite side (Fig. 2-2). Instability is a symptomatic, subjective sense of unease, discomfort, or pain in the setting of excessive translation. The other shoulder should be used as a control, taking care to assess symptoms during provocative testing and to elucidate whether the day-to-day complaints are being recreated upon a specific maneuver. The patient history is very helpful at this point to aid in differentiating laxity from instability. Two seemingly identical patients may have a 2-cm sulcus sign, but if one patient perceives instability while lifting a suitcase with the adducted arm and the other patient does so without difficulty, then the former patient is more likely to suffer from instability, whereas the latter may simply have excessive laxity that is asymptomatic and therefore likely not pathologic.
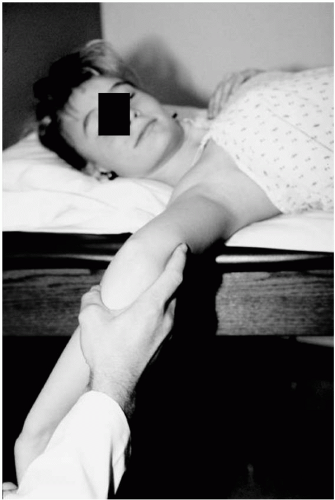 Figure 2-2 A patient exhibits excessive physiologic laxity, which is not symptomatic. Be cautious to differentiate laxity from instability. |
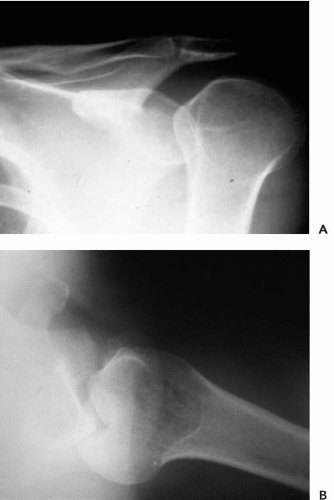
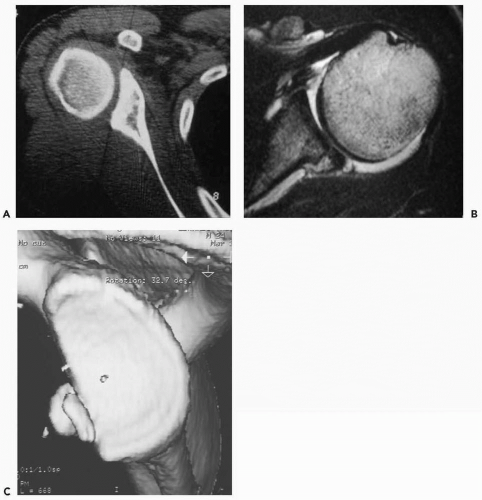
Lastly, proper imaging will aid in making an accurate diagnosis. All patients should be initially evaluated with appropriate radiographs (true AP, axillary lateral) (Fig. 2-3). Cross-sectional imaging usually involves magnetic resonance imaging (MRI), in which labral pathology, cartilage wear, and glenoid version can be assessed. Depending on the quality of the MRI, computed tomography (CT) is a very useful adjunct to accurately assess glenoid version and bone stock, bony avulsions of the capsulolabral complex, and Hill Sachs/reverse Hill Sachs defects (Fig. 2-4). It has been shown that glenoid version cannot be accurately assessed on plain axillary radiographs and that more advanced imaging is necessary (22).
Failure to appreciate glenoid retroversion, hypoplasia, or avulsions, as well as large Hill Sachs lesions, is a common cause of failed instability procedures (2,7,13,23). It is crucial to evaluate the bony anatomy preoperatively, using proper imaging as above, with an appreciation of the role
of the bony articulation in overall glenohumeral stability. Traditionally, focus has centered on addressing the static and dynamic contributors to stability by attempting to rehabilitate the rotator cuff and scapular stabilizers, and to restore normal capsulolabral architecture and tension. Much work has been done on the role of the anterior inferior glenoid in recurrent anterior instability, which is covered in another chapter. Likewise, purely soft tissue procedures in the presence of excessive glenoid retroversion, hypoplasia, or other posterior bony deficiencies are doomed to fail (1,2,7,11,13,22,23).
of the bony articulation in overall glenohumeral stability. Traditionally, focus has centered on addressing the static and dynamic contributors to stability by attempting to rehabilitate the rotator cuff and scapular stabilizers, and to restore normal capsulolabral architecture and tension. Much work has been done on the role of the anterior inferior glenoid in recurrent anterior instability, which is covered in another chapter. Likewise, purely soft tissue procedures in the presence of excessive glenoid retroversion, hypoplasia, or other posterior bony deficiencies are doomed to fail (1,2,7,11,13,22,23).
Pearls
Always rule out cervical spine pathology when evaluating the shoulder.
Seek to classify the instability by degree (subluxation, dislocation, or locked dislocation), mechanism (traumatic or atraumatic), chronicity (acute or chronic), direction (uni-, bi-, or multidirectional), or volition (involuntary or voluntary).
Tailor your history and physical examination to specifically differentiate unidirectional instability from multidirectional instability.
Remember that laxity does not equal instability.
Use advanced imaging such as CT and MRI to carefully assess glenoid version and bone stock as well as humeral Hill-Sachs lesions.
Patient Expectations
Healthcare has gradually shifted toward a market model, with consumer satisfaction a major driving force for
change. Consumers are increasingly determining how health care is delivered and administered, and traditional tools of measuring clinical outcomes are likewise evolving. Over the last decade, the outcomes assessment movement has evolved in response to these and other forces, becoming a major component of patient care. Outcomes instruments include generic measures of health quality-of-life such as the SF-36, condition-specific measures of disease such as the American Shoulder and Elbow Surgeons Score, and measures of patient satisfaction.
change. Consumers are increasingly determining how health care is delivered and administered, and traditional tools of measuring clinical outcomes are likewise evolving. Over the last decade, the outcomes assessment movement has evolved in response to these and other forces, becoming a major component of patient care. Outcomes instruments include generic measures of health quality-of-life such as the SF-36, condition-specific measures of disease such as the American Shoulder and Elbow Surgeons Score, and measures of patient satisfaction.
Commensurate with being responsive to patient outcome and satisfaction, clinicians are increasingly attuned to the need to assess a patient’s preoperative expectations of a successful outcome. Mancuso and colleagues developed a 17-item Hospital for Special Surgery Shoulder Surgery Expectations Survey, which can serve as a guide to understand the patient’s perspective and as a template to direct preoperative discussions and education (24). Questions assess the relative importance of such varied features as the relief of night pain, the regaining of motion, the return to employment, and the improvement of psychological well-being.
Specifically with regards to shoulder instability, patient expectations may be varied. For the professional football lineman with a history of traumatic posterior instability, the ability to return to the same level of play with stability is paramount. For the overhead athlete, regaining range of motion may even supersede stability as the primary surgical goal. Lastly, for the young female with generalized ligamentous laxity and multiple daily episodes of subtle instability, merely returning to a more normal quality of life may be the primary goal. For each patient, a careful assessment of his or her preoperative expectations will facilitate the development of shared, reasonable goals of treatment. It is important to understand and to communicate to patients that all expectations may not be attainable; the true error would be to fail to recognize and address this disparity with the patient before undertaking a surgical relationship.
Pearls
Outcome instruments include generic measures of health quality of life, condition-specific measures of disease, and measures of patient satisfaction.
Patient expectations regarding outcome after instability surgery, and especially after revision surgery, vary widely.
Each patient’s expectations must be addressed carefully in the initial stages to tailor a treatment strategy that is individualized and to educate him or her about reasonable expectations.
INTRAOPERATIVE ERRORS
Intraoperative complications are encountered in the surgical approach and through manipulation of the soft tissues and bony structures in the shoulder. Careful attention to patient positioning, a thorough knowledge of anatomy, familiarity with all instruments and hardware, and the use of intraoperative fluoroscopy will all serve to minimize surgical complications. Of course, a well-designed preoperative plan as discussed in the previous section will facilitate adequate preparation by assuring that all of these criteria are met.
Complications of the Posterior Approach to the Shoulder for Instability Repairs
The posterior approach to the shoulder has been well described (3,5,25,26). Several critical points warrant emphasis to avoid surgical complications.
Patient positioning is important and is often determined by the possible need for other procedures. In general, we favor the use of an arm holder, either the hydraulic arm holder (Spider Limb Positioner, Tenet Medical Engineering, Calgary, Canada) or the McConnell arm holder (McConnell Orthopaedic Manufacturing Company, Greenville, TX). These devices allow the arm to be rigidly positioned in space without the need for an additional surgical assistant for this purpose. If a combined open anterior and posterior approach is used, then either the beach chair or the lateral decubitus position on a bean bag can be used. We prefer the beach chair position, with the hemithorax clear for adequate exposure. This facilitates multiple simultaneous approaches to the shoulder, including arthroscopy. The lateral decubitus position could also be employed with an initial arthroscopic evaluation, depending on the surgeon’s preferences.
The posterior skin incision should be made vertically in Langer’s lines for cosmesis, centered over the glenohumeral joint. This is especially important in the female instability population, who often have generalized ligamentous laxity and surgical scars that stretch widely while healing. The deltoid should be split between its posterior and middle thirds in line with its fibers, which run obliquely in relation to the skin incision. Neurovascular injury can be avoided with a sound understanding of the anatomy of the suprascapular nerve, circumflex scapular artery, axillary nerve, and posterior circumflex humeral artery. Ball et al. (27) described the anatomy of the posterior branch of the axillary nerve as it relates to open and arthroscopic procedures of the posterior shoulder. The deltoid may be split up to 4 cm distal to the edge of the acromion, as the axillary nerve branches that supply the deltoid lie approximately 5 cm distal to the lateral edge of the acromion. These branches largely come from the anterior branch, but there is a variable (and redundant) contribution from the posterior branch. The two other contributions from the posterior branch of the axillary nerve are the branches to the teres minor and the superior-lateral brachial cutaneous nerve.
This cutaneous branch passes around the medial aspect of the deltoid, on average 8.7 cm distal to the posterolateral corner of the acromion; as it becomes a terminal branch, it is not endangered during routine surgical dissection. However, the more proximal posterior branch itself and its immediate branches lie directly adjacent to the capsule at the inferior aspect of the glenoid rim. The nerve is at particular risk during both open and arthroscopic procedures involving the posterior inferior capsule. A clinical pearl offered by Ball et al. (27) suggests that postoperative sensory changes in the distribution of the superior-lateral brachial cutaneous nerve might be a harbinger of coexistent injury to the nerve supply to the teres minor.
This cutaneous branch passes around the medial aspect of the deltoid, on average 8.7 cm distal to the posterolateral corner of the acromion; as it becomes a terminal branch, it is not endangered during routine surgical dissection. However, the more proximal posterior branch itself and its immediate branches lie directly adjacent to the capsule at the inferior aspect of the glenoid rim. The nerve is at particular risk during both open and arthroscopic procedures involving the posterior inferior capsule. A clinical pearl offered by Ball et al. (27) suggests that postoperative sensory changes in the distribution of the superior-lateral brachial cutaneous nerve might be a harbinger of coexistent injury to the nerve supply to the teres minor.
The internervous plane deep to the deltoid, as classically described, lies between the infraspinatus (suprascapular nerve) and the teres minor (axillary nerve), for the axillary nerve and the posterior circumflex humeral artery run in the quadrilateral space just inferior to the teres minor. Thus emphasis has been made to keep the plane of dissection superior to the teres minor. However, developing this plane between the infraspinatus and the teres minor is often difficult, as the muscle fibers coalesce medially, as do the tendonous insertions laterally on the greater tuberosity. Therefore, the surgeon may choose to split the bipennate infraspinatus between its two heads, a technique described by Jobe et al. (28). A fat stripe is usually present as a landmark for this plane (Fig. 2-5). A benefit to the infraspinatus split is that the plane of dissection, carried laterally, brings one to the equator of the glenohumeral joint as opposed to the inferior aspect of the glenoid, which is advantageous for posterior labral work. The plane between the infraspinatus and teres minor brings one inferior to the glenoid equator, which is ideal to dissect the inferior posterior capsule for a large shift. This is our preferred approach when performing such a shift.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree