INTRODUCTION
Shoulder arthroplasty has steadily increased in popularity since Neer and colleagues introduced their prosthesis for complex three- and four-part proximal humerus fractures in 1953 (
1). Since that time, the indications for shoulder replacement have expanded to include various primary and secondary degenerative shoulder conditions such as osteoarthritis, rheumatoid arthritis, cuff tear arthropathy, and the late sequelae of trauma. According to the National Center for Health Statistics, approximately 13,000 shoulder replacements were performed in 1999 (
2). Although shoulder replacement is generally successful in relieving pain and improving shoulder function, as the number of shoulder arthroplasties has increased, so has the number of unsuccessful arthroplasties requiring reoperation. In the latest edition of their text, Matsen and colleagues (
3) reported that in 22 series of shoulder replacement, the average reoperation rate was 7%.
Despite the growing number of shoulder replacements, very little has been written about complications, causes of failure and techniques, and results of revision. In 1982 Neer and Kirby (
4) were the first to report on the causes of failure and discussed techniques of revision in a series of 40 failed shoulder arthroplasties. In the same year, Neer and associates
(
5) reported the outcome of 26 of those shoulders as part of a larger series of shoulder replacements. Since that time, Cofield and Edgerton (
6) and Wirth and Rockwood (
7,
8) have written specifically on complications of shoulder arthroplasty, discussing causes of failure and methods of revision. Subsequently, a number of authors have published series focusing on specific complications of shoulder arthroplasty, and numerous authors have included a few complications or revisions in large series of shoulder arthroplasties. In 2002 Hasan and colleagues (
9) expanded our understanding of complications by noting that some shoulder arthroplasties may have an unsatisfactory result even if there is no traditional “complication,” whereas others may suffer a typical complication, such as an intraoperative fracture, yet have a very satisfactory result.
This chapter summarizes the current literature concerning complications of shoulder arthroplasty and their treatment, beginning with a discussion of the common types of complications, their incidence, and attempts at classification. The chapter concludes by discussing the evaluation of the unsatisfactory shoulder arthroplasty, the natural history of individual complications, indications for operative and nonoperative treatment, and techniques of revision.
DEFINITIONS/CLASSIFICATIONS/HISTORICAL REVIEW
In 1982 Neer and Kirby published the first report on the revision of failed hemi- and total shoulder arthroplasties (
4). They treated 40 failed shoulders in 36 patients, converting almost all of them to total shoulder arthroplasty (TSA). Patients averaged two prior surgeries and approximately 2 years from the prior operation to revision. Twenty-seven of the 40 were initially performed for acute trauma (8 patients) or its sequelae (19 patients). Their focus was on the causes of failure, which they divided into preoperative, surgical, and postoperative considerations. Preoperative considerations included psychological and neuromuscular issues, adjacent joint problems, and infection. Surgical considerations were divided into soft-tissue, bone, and prosthesis problems, and glenohumeral instability and the function of remaining muscles were classified as postoperative concerns. The most common complications were deltoid scarring and detachment, a tight subscapularis, adhesion and impingement of the rotator cuff, prominence or retraction of the tuberosities, loss of humeral length, uneven glenoid wear or centralization, and lack of a supervised rehabilitation program. More than one cause of failure was present in nearly every case.
With Watson and Stanton, Neer reported the results of 26 of these revisions in 23 patients as part of a larger series on the results of TSA in 273 shoulders (
5). Ten shoulders were excellent according to Neer, achieving normal use of the shoulder, full strength and no significant pain, active elevation to within 35 degrees, and rotation to within 90 percent of the normal side. Eleven were satisfactory according to limited goals criteria, with good use for daily activities to the top of the head, 30% of normal strength, only occasional pain, elevation of 90 to 135 degrees, and rotation to 50% of the normal side. According to these criteria, five patients had unsatisfactory results, which were attributed to poor motion stemming from deltoid or rotator cuff weakness rather than pain.
The next authors to deal with the failure of shoulder arthroplasty on a large scale were Cofield and Edgerton (
6). In 1990 they reviewed 29 studies of shoulder arthroplasty with sufficient data to analyze complications. Among nine large series of unconstrained shoulder replacement, the average rate of revision surgery was 6.6%. Although they did not propose a classification, they did list major complications in order of decreasing frequency, with glenoid loosening being the most common, followed by instability and rotator cuff tearing. Humeral loosening, infection, and nerve injury followed. Reviewing the 79 complications leading to revision surgery that was performed at their institution, they found that glenoid loosening and displacement of polyethylene from metal backed glenoids were the most common complications of TSA and that glenoid arthritis was the most common complication in hemiarthroplasty (HA). Instability and rotator cuff tearing were the next most common, closely followed by humeral loosening and infection. These authors also emphasized that multiple causes of failure may coexist and that all must be recognized and corrected for a successful revision. Because of the great variability among these patients, they did not report results of revision.
Wirth and Rockwood (
7,
8) reviewed the literature on complications of shoulder replacement and found that reported complications, in order of decreasing frequency, were as follows: loosening of glenoid components, instability, rotator cuff tear, periprosthetic fracture, infection, failure of the implant (e.g., dissociation of a modular prosthesis), and deltoid dysfunction. They reviewed data concerning 38 failed unconstrained shoulder arthroplasties they revised and found that acute trauma was the most common reason for the index arthroplasty. As in other series, reason for failure was typically multifactorial. The most common complication leading to revision was instability, with other causes of failure, in order of decreasing frequency, being deltoid detachment, glenoid loosening (after TSA), glenoid erosion (after HA), humeral loosening, greater tuberosity detachment or malunion, osseous or fibrous ankylosis, infection, and modular component dissociation. Although results were not reported in their review, Wirth does cite American Academy of Orthopaedic Surgeons presentations by Caldwell and colleagues (
10) and Wirth and associates (
11) with 67% and 75% satisfactory results among shoulders revised to another arthroplasty. In a similar series, Connor and colleagues (
12) reviewed 50 revision shoulder arthroplasties and found excellent and satisfactory outcomes in 62%.
More recently, Hasan and colleagues (
9) have defined failure as patient dissatisfaction with the procedure and
reported on the characteristics of 141 unsatisfactory shoulder arthroplasties presenting to the Shoulder Service at the University of Washington. They found that the rate of revision underestimated the rate of failure, with 23% of the unsatisfactory arthroplasties not coming to revision. Pain and weakness were common but were considered expressions of failure, not causes. They considered numerous possible characteristics of the failed shoulders and noted an average of 2.5 characteristics of failure in each. The most common characteristic of the unsatisfactory arthroplasties was stiffness, which was present in 74%. The next most common cause of failure was glenoid loosening (59%) among failed TSA and glenoid erosion (42%) among HA. Instability, component malposition, rotator cuff tears, and humeral loosening were also noted, and tuberosity nonunion occurred in 43% of failed HA performed for proximal humerus fracture. Function, as measured by the simple shoulder test, and general health, as measured by the Short-Form-36 (SF-36), were significantly compromised.
We reviewed and presented our experience with revision shoulder arthroplasty at the University of Texas Health Science Center at San Antonio (UTHSCSA), analyzing causes of failure in 94 arthroplasties and the outcomes of revision in 65 of these (
13). Operations that did not include revision of at least one component were not considered in this series. Preoperative and postoperative conditions were not considered as separate categories in the review. The vast majority of patients (75%) had more than one cause of failure of their arthroplasty. Causes of failure were categorized as being soft-tissue problems, humeral component problems, or glenoid problems. Tuberosity malunion or nonunion after arthroplasty for proximal humerus fracture were considered to represent a failure of reattachment of the rotator cuff and were therefore classified with the soft-tissue problems. The most common soft-tissue complication was instability, followed by stiffness, tuberosity malunion/nonunion (after fracture), and subscapularis rupture. The rotator cuff rarely was implicated as a cause of failure in the series. The most common complication related to the humeral component was incorrect version, which was twice as common as problems with head size, stem height, and humeral loosening. The native glenoid required resurfacing or smoothing in 36 of 55 failed Has, and the prosthetic glenoid was loose or worn in 31 of 39 failed TSAs.
Cofield and colleagues have also provided a compilation of complications seen at the Mayo Clinic over a twodecade span (
14). They identified 157 surgical complications in 90 of the 419 patients who had undergone TSA and 49 complications among the 83 patients who had undergone HA for proximal humerus fractures and their sequelae. In contrast to the two reviews mentioned previously, stiffness was rarely, if ever, considered a cause of failure in this series. A summary of the more common complications of TSA and HA found in these three series follows. (See also
Tables 16-1 and
16-2.)
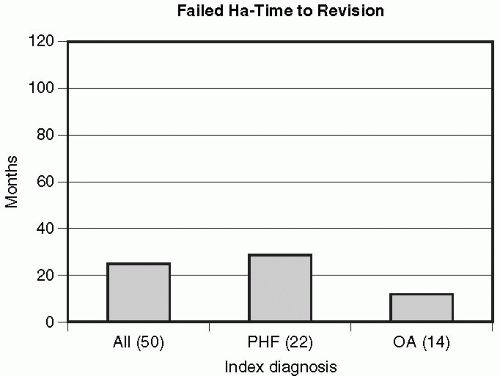
Although the timing of failure is rarely discussed, the analysis of our revisions revealed interesting trends. Of the
55 failed HAs, five were initially successful, lasting an average of 13 years before revision, whereas 50 (91%) were never considered successful by the patient and were revised at an average of only 23 months. The vast majority of causes of failure in this group could be termed avoidable errors. The subset of failed HA for proximal humerus fracture was slowest to revision, at an average of 28 months, and the subset of failed HA for osteoarthritis was fastest, at an average of 12 months (
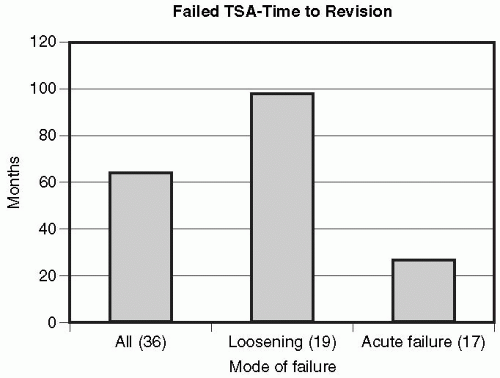
Fig. 16-1). In contrast, the timing of failure of TSA was bimodal. Approximately half failed early, in association with instability, and were revised at an average of 19 months. The other half failed late as a result of aseptic loosening and were revised at an average of 99 months (
Fig. 16-2).
Because the causes of failure are so disparate, classification is difficult. For purposes of this chapter, we use a modification of the University of Texas Health Science Center at San Antonio’s (UTHSCSA) system of soft-tissue, humeral, and glenoid problems as the broad categories of postoperative complication. To improve understanding of the causes of failure, they are often discussed in the context of the index diagnosis. For purposes of simplicity, some complications, such as nerve injury and heterotopic ossification, are grouped with the soft tissues. Additional complications not specific to shoulder arthroplasty (e.g., pulmonary embolus and infection) are also included.
EVALUATION OF THE FAILED SHOULDER ARTHROPLASTY
Evaluation of the failed shoulder arthroplasty begins with a careful history and physical examination, followed by appropriate diagnostic studies. As much as is possible, the preoperative evaluation should determine the causes of failure and whether a fixable problem exists. Finally, the needs of the patients and their ability to undergo a revision arthroplasty must be considered.
The history is critical in helping to determine the causes of failure of the arthroplasty. The index diagnosis, details of prior surgical procedures, and the timing of failure of the primary arthroplasty all provide critical information. In the patient who fails to improve following an elective arthroplasty, possible problems include instability, often resulting from a ruptured subscapularis repair, an unaddressed lax posterior capsule, or an error of component positioning. Failure of an arthroplasty to relieve pain may also result from failure to resurface an arthritic glenoid or from the development of postoperative stiffness. Patients with unsuccessful arthroplasty for fracture may have problems with tuberosity position or healing or with the position of the humeral component. Infection may occur either early or late and should always be included in the differential for any unsuccessful arthroplasty. Late failure after a period of satisfactory function most typically is the result of glenoid loosening, dissociation after TSA, or the development of glenoid arthrosis following HA. Humeral loosening is less common but may also occur, typically in the setting of TSA, when glenoid wear debris may induce osteolysis around the humeral stem (
15).
Physical examination begins with inspection of the shoulder for evidence of rotator cuff dysfunction and atrophy or detachment of the deltoid. Active and passive range of motion is recorded, as are the strength of the deltoid, external rotators and subscapularis, and the function of the peripheral nerves. The stability of the shoulder in all directions—anterior, posterior, inferior and superior—also is evaluated. In addition, a standard shoulder examination should be carried out because more chronic problems such as impingement and acromioclavicular arthritis can also compromise the results of shoulder replacement.
For preoperative imaging, standard radiographs usually will suffice. At a minimum, a “true” anteroposterior (or posterior oblique view) in internal and external rotation, a scapular “Y” view, and an axillary view should be obtained. Whenever they are available, serial x-rays should be reviewed for evidence of progressive radiolucent lines, osteolysis, or change in implant position. If fluoroscopy is available, it may occasionally be used to obtain tangential views of the glenoid to enhance the detection of radiolucent lines about the glenoid or the humeral stem to determine humeral version.
Sperling and colleagues (
16) have reviewed the radiographs of primary ingrowth TSAs and determined a number of “at risk” criteria for clinical component loosening. A glenoid component was “at risk” when a complete lucent line was present, some part of it being 1.5 mm or greater in width, or when two or more independent observers identified migration or tilt of the component. A humeral component was “at risk” when a lucent line 2 mm or greater in width was present in three or more of eight zones or when at least two observers identified tilt or subsidence of the component.
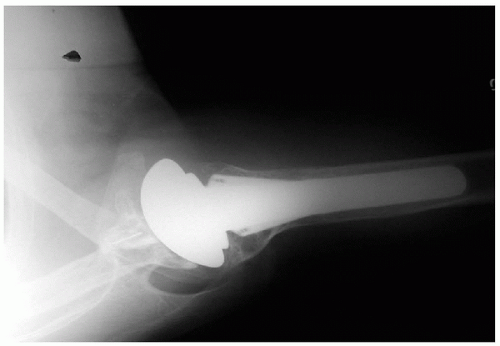
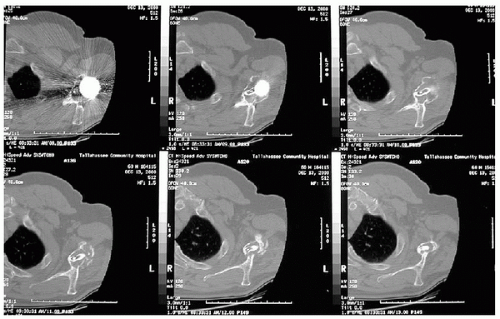
If questions regarding the status of the osseous or soft-tissue structures remain (
Figs. 16-3 and
16-4) magnetic resonance image (MRI) may be added.
Computed tomography (CT) scans can be helpful in special circumstances, although the quality of the images may be lessened by artifact from the metallic stem. They are particularly useful for determining the position and healing of the tuberosities, for assessing the shape and version of the glenoid, and for evaluating glenoid loosening when the plain films are not conclusive (
Fig. 16-5).
For the painful arthroplasty that presents a diagnostic dilemma, MRI can also be used to evaluate the rotator cuff and the glenoid cartilage. Sperling and colleagues (
17) correlated the MRIs of 22 painful shoulder arthroplasties with operative findings at subsequent revision surgery. At the time of revision surgery, there were full-thickness rotator cuff tears in 11 of 21 shoulders; MRI had correctly predicted 10 of these 11 full-thickness rotator cuff tears, which involved the subscapularis in 8 of 11 shoulders. MRI also correctly predicted glenoid cartilage wear in 8 of 9 shoulders.
When the history, physical examination, and radiographic tests do not provide a clear diagnosis, shoulder arthroscopy can provide additional diagnostic information and also presents options for treatment. Bonutti and colleagues (
18) reviewed nine patients who underwent
arthroscopy followed by open surgery to confirm arthroscopic findings. They found that arthroscopy accurately evaluated glenoid component loosening in all patients with this problem. O’Driscoll and colleagues (
19) reported on three cases in which the loose glenoid was removed arthroscopically following the diagnosis. Hersch and Dines (
20) reported on 13 arthroscopies performed for poor results following shoulder arthroplasty. The arthroscopic diagnoses ranged from rotator cuff tears in five shoulders, fibrosis and scarring of the long head of the biceps in five shoulders, impingement and biceps tendinitis in one shoulder, and capsular contracture in one shoulder. They repaired or debrided the lesions at the time of arthroscopy, with few complications and excellent patient satisfaction.
Tytherleigh-Strong and colleagues (
21) reported on 29 patients who underwent arthroscopy for excessive pain or limitation of motion after a shoulder arthroplasty. Although the procedures were often hindered by limited access and reflection from the prosthesis, preoperative diagnoses were confirmed in 14, including impingement syndrome in 10 patients (treated by arthroscopic subacromial decompression). Of the 15 patients without a preoperative diagnosis, 7 had postarthroplasty capsular fibrosis, with 6 undergoing arthroscopic capsular release.
A final complication that must be ruled out for any failed, painful arthroplasty is infection. Although infection after shoulder replacement is rare, and there is a paucity of literature regarding the preoperative evaluation of a potentially infected shoulder arthroplasty, there are significant lessons that can be drawn from the literature on infected hip arthroplasty. Spangehl and associates (
22) reviewed preoperative and intraoperative data on 202 revision hip replacements and found that 35 (17%) were infected on the basis of clinical findings and positive laboratory results. All patients who had a periprosthetic infection had an elevated erythrocyte sedimentation rate or level of C-reactive protein but not always both. In other words, in this series, if a patient had a combination of a normal erythrocyte sedimentation rate and a normal C-reactive protein level, the probability of infection was zero.
Plain radiographs may show bone resorption around the components, endosteal scalloping, or periosteal new bone formation. Indium-labeled white cell scan also may be used occasionally. Aspiration and culture are useful when prior studies do not clearly indicate the status of the shoulder. Gram stain is unreliable. Examination of intraoperative frozen sections is useful in equivocal cases or when hematologic markers could be falsely elevated because of an inflammatory or other condition.
SOFT-TISSUE COMPLICATIONS
Instability
Overall, the most common complication after shoulder replacement is instability. According to his recent Instructional Course Lecture, Brems (
23) noted that instability following all surgeries on the shoulder comprises up to 38% of complications and may occur in up to 22% of shoulder arthroplasties. In our series, instability was one of the characteristics of failure in 26 (28%) of 94 revisions. In reviews on postoperative instability, Norris and Lipson (
24), Hennigan and Iannotti (
25), and Warren and colleagues (
26) have all noted that the instability may occur in any direction—anterior, posterior, superior, or inferior—based on the position of the components and the condition of the soft tissues.
In a Mayo Clinic review of 419 total shoulder arthroplasties, subluxation was identified in 11%, developing early in one-third, occurring late in two-thirds, and requiring reoperation in 72% (
27). In a separate report on 50 arthroplasties undergoing revision for instability, component problems were a primary cause of the instability in 18 of the 50 shoulders, with the remainder being soft-tissue abnormalities. When revision consisted only of soft-tissue repair, only 24% had an excellent or satisfactory result. When change of the prosthetic position was included at the time of the revision surgery, the rate of excellent or satisfactory result went up to 48%, but at best, the likelihood of improving this situation with revision surgery was only moderate.
As with all complications, the best treatment is prevention, with careful attention to soft-tissue technique and component position being the crucial elements in avoiding instability. When instability does occur, it is important to recognize and correct all factors contributing to the problem as early as possible because continued instability may result in component wear or loosening. Although more detailed descriptions of glenoid and humeral revision are presented later in this chapter and in the chapter on revision arthroplasty, this section does address aspects of revision as they particularly apply to instability.
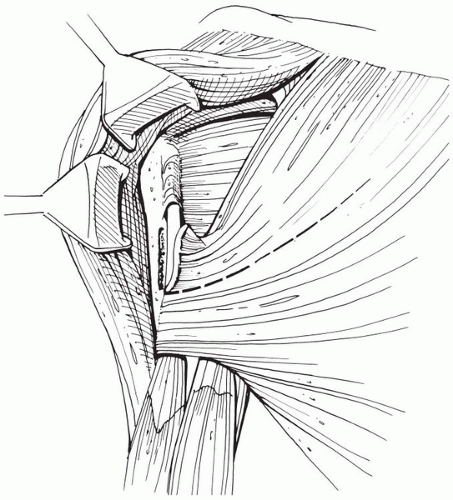
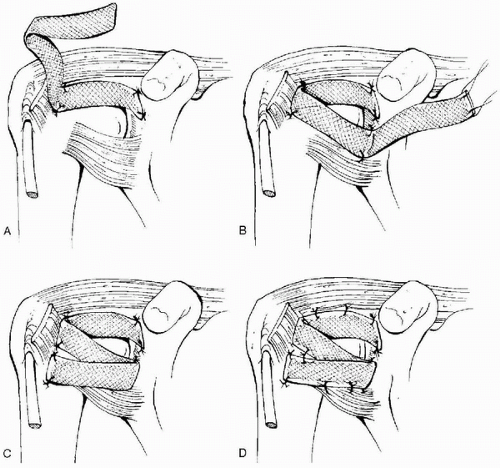
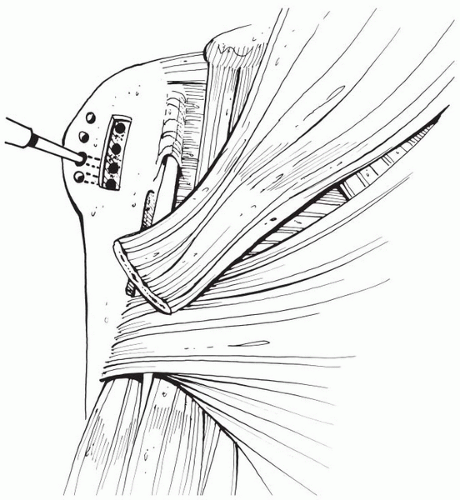
In most series, anterior instability occurs acutely and is typically the result of rupture of the subscapularis tendon or excessive humeral anteversion. Overstuffing the joint with an excessively large humeral head can also cause problems with the subscapularis repair. At the time of revision, a careful search for the subscapularis is an important part of the surgical approach. If it is present and can be mobilized sufficiently, it may be re-repaired, but there may be times when it is irretrievable. In this circumstance, transfer of the pectoralis major may be necessary to restore anterior stability. A number of techniques, including transfer of the sternal head (
28)and partial (
29) or complete (
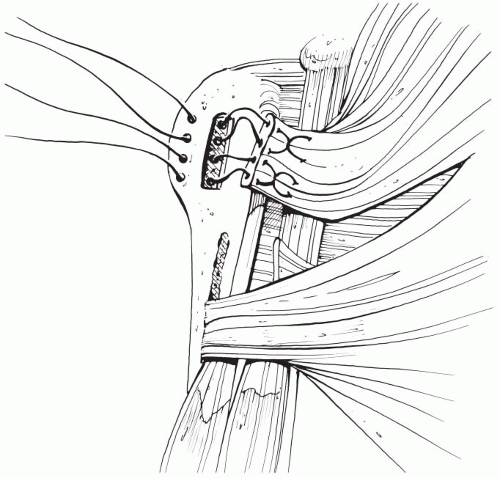
30) subcoracoid transfer have been described. Our preference is to transfer the upper half of the entire tendon over the conjoined tendon and attach it to the greater tuberosity (
Figs. 16-6,
16-7, and
16-8) (
31). Once a dynamic anterior muscle tendon unit has either been mobilized for rerepair or prepared for transfer, attention is directed to the capsule. In cases where anterior instability is severe, it may be necessary to reestablish a capsular restraint as well. Moeckel and colleagues (
32) identified seven patients with
anterior instability caused by a rupture of the repaired subscapularis tendon after shoulder arthroplasty. Treatment consisted of mobilization and repair of the tendon, but three of the seven patients continued to have instability. A static stabilizer, consisting of an allograft of Achilles tendon, was inserted in these three patients. In 2002 Iannotti and colleagues (
33) described a method of iliotibial band reconstruction for irreparable capsular deficiency that could also be considered in this situation (
Fig. 16-9). In the UTHSCSA review, of 94 failed arthroplasties, 12 had subscapularis rupture with associated early anterior instability. In addition to repair of the detached subscapularis or transfer of the pectoralis major, revision consisted of correction of any errors of humeral component position. In many cases, excessive anteversion of the stem is a contributing factor to anterior instability. Although it may occasionally be possible to compensate for errors in stem position by changing the position of an eccentric head, in general, an improperly place humeral component should be revised to the appropriate height, size, and version.
Finally, the glenoid must be inspected. In many cases in our series, the unstable humeral head had eroded, loosened, or dissociated a prosthetic glenoid or eroded the anterior rim of the native glenoid. If instability has caused a prosthetic glenoid to fail, it should be removed and a new glenoid should be inserted or cancellous bone graft should be impacted into the empty vault. In some circumstances, we have encountered so much anterior erosion that it has been necessary to either insert a prosthetic glenoid to improve stability or increase the humeral retroversion to match an anterior-facing glenoid.
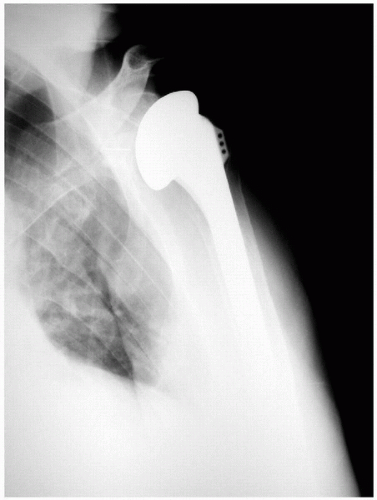
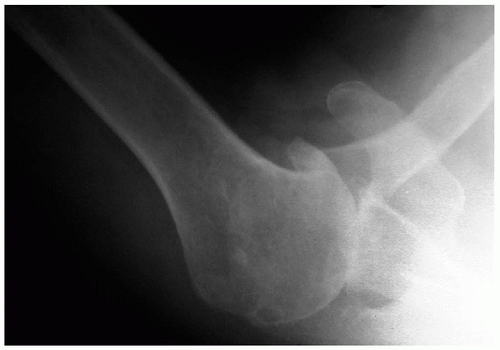
In contrast to anterior instability, posterior instability may either occur early or develop late and is usually attributable to combined excessive retroversion of the humeral and glenoid components. This is particularly problematic in patients with an index diagnosis of osteoarthritis, with its characteristic combination of posterior glenoid wear,
excessive glenoid retroversion, and a lax posterior capsule. Failure to address this pathology at the index surgery can lead to either immediate posterior instability or continued stretching of an already patulous posterior capsule, with the instability developing later (
Figs. 16-10,
16-11,
16-12).
Although some have addressed posterior instability from the back of the joint, our preference has been to correct it from the front. After opening the deltopectoral interval, one is usually able to find the subscapularis. Lack of external rotation can also contribute to posterior instability, and if the subscapularis is tight it should be lengthened, either by medializing its insertion or by a zlengthening of the tendon and capsule.
Revision is facilitated by modular humeral designs. If the stem is appropriately placed, it is possible to access the glenoid and posterior capsule merely by removing the humeral head. However, if the stem itself is inappropriately located, it should be removed and revised to the appropriate size, height, and version.
With the humeral head removed, a bone hook pulling laterally on the shaft gives access to the posterior capsule. If it is patulous we either plicate or cut and oversew the posterior capsule to decrease posterior translation. Appropriate posterior capsular tension is achieved when, with the arm in neutral rotation, gentle posteriorly-directed pressure on the humeral head allows it to translate approximately 50% of the anterior to posterior dimension of the glenoid. If desired, additional posterior stability can be obtained at the end of the procedure by securely closing the rotator interval, although one must be cautious about an excessively tight closure limiting external rotation.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access