Complications of Reverse Total Shoulder Arthroplasty
Anders L. Ekelund
INTRODUCTION
The Grammont-type reverse shoulder arthroplasty (RSA) is being used with increasing frequency, and many different conditions resulting in rotator cuff deficiency can now be successfully treated with this technique.3,9,11,13,17,19,24,25,31,38,42,46,51,53,56,57,61,63,64,66 In some cases this technique is used together with tendon transfer to improve functional external rotation.6,27 There are more than 20 different RSAs currently on the market based on the principles of Professor Grammont.3,8,29,30
There has been a concern regarding the incidence of complications after this procedure and the long-term survival of the RSA. The early series reported promising clinical results, but complication rates of 15% to 50% and revision surgery in up to 40% of the patients occurred.3,9,24,29,51,52,54,56,61,63,64 and 65 However, it should be noted that the high incidence of complications in these series could be the result of patient selection and how complications were defined. Since these early series were published, the implant designs have been changed and surgical technique has improved.
In a recent systematic review, an overall complication rate of 25% was found and the most common reported complications were instability (4.7%) and infection (4%).68 Complications were seen more frequently after revision surgery compared with patients undergoing primary RSAs. Furthermore, the deltopectoral approach was associated with more complications compared with the superolateral approach (23.5% compared to 18.7%) and resulted in more revision surgeries (9.5% compared to 5.8%). Comparison is, however, complicated since more complex cases are performed through the deltopectoral approach and the superolateral approach is commonly used in the more straightforward primary cases.
The number of RSAs is rapidly increasing and the technique is used by surgeons who perform only a limited number of these procedures each year. It is therefore important to have knowledge about potential problems and complications, and how to manage them. Consequently, this chapter is a review of reported postoperative complications following RSA. The guidelines regarding the treatment are given based on the literature and the author’s experience of over 800 RSAs over more than 15 years.
COMPLICATIONS AFTER REVERSE SHOULDER ARTHROPLASTY
Instability
Incidence
In a French multicenter study of 457 RSAs in 430 patients, the incidence of dislocation was 4.8% (Fig. 23-1).61 However, all dislocations (22 patients) occurred after the use of the deltopectoral approach, giving an incidence of 6% in that group. Dislocation was more common after revision of failed anatomical arthroplasties (11%) and in post-trauma cases (9%) compared with cuff tear arthropathy (4%). Of the 22 patients suffering from a dislocation, 16 occurred within the first 3 months. In a more recent review of 284 RSAs, Trappey et al. reported a 5% incidence of instability in the primary group compared with 8% in the revision group (P = 0.388).59
Subscapularis insufficiency resulted in an increased risk of instability, and repair of the tendon was recommended, if possible.18,59
Subscapularis insufficiency resulted in an increased risk of instability, and repair of the tendon was recommended, if possible.18,59
In the author’s series (AE) of the first 236 Delta RSAs (1995 to 2002), 16 patients went on to suffer dislocation, giving an incidence of 6.7%. Twelve of these dislocations were seen after revision of failed arthroplasty and three were seen in patients with fracture sequelae. Only one dislocation occurred in the cuff tear arthropathy group. Since 2006, we have used the Delta Xtend RSA (DePuy) and three dislocations occurred in 457 consecutive RSAs (0.7%). Thus, with modern implant design and careful surgical technique, the incidence of instability of RSAs can be very low.
The most important stabilizing factor in an RSA is compressive forces in the joint (deltoid tensioning), followed by socket depth.33 The size of the glenosphere was found to have less importance. Favre et al. studied the effect of version of the components and reported that the stability was improved if the humeral component was put in neutral or slightly in anteversion.22 Retroversion of the humeral component decreased the stability.
Another situation that could cause instability is when the humerus is levered out, after the humeral bone comes into contact with the scapula at different positions. Performing releases, removing scar tissue around the glenoid—particularly inferior—and excising bony fragments around the glenoid are important steps to avoid instability. Furthermore, by using a larger diameter glenosphere at a low position, the risk is further reduced since bony impingement is minimized.
Diagnosis
Instability can occur as episodes of subluxation or a complete dislocation. Subluxations are easily recognized by the patient and diagnosis is therefore straightforward. The characteristics of the other group of patients are different. Complete dislocation occurs at some point postoperatively and it is our experience that these are often pain-free. This means that the patient is not always aware of the fact that the RSA is dislocated. Indeed, several cases that we have identified were detected on routine radiographs taken at the first standard postoperative follow-up at 3 months.
If the patient notices a sudden drop in active range of motion during postoperative rehabilitation, a dislocation should be suspected. The complete instability is usually diagnosed within the first 3 months. Two cases of late instability have been seen in the author’s series after 5 to 7 years. The cause was wear of the polyethylene insert, and both were revised with new polyethylene inserts, with good outcomes. The position of the dislocated humeral component relative to the glenosphere on radiographs varies in the same patient and can be posterior, inferior, or anterior. Most often, the humeral component is anterior to the glenosphere.
Management
The results after the treatment of RSA instability have been variable. In the French multicenter study, 22 patients with instability were identified.61 Seven cases were treated with closed reduction and immobilization, and physiotherapy was postponed until 4 to 6 weeks later. Nine cases underwent revision (open reduction, two cases; polyethylene liner change to a more constrained design, two cases; humeral spacer inserted, five cases). The remaining six patients had no further treatment. Seven of these 22 patients presented with a dislocation more than 1 month after surgery. None of these patients underwent revision and all remained unstable at last follow-up.
Gallo et al. reported on nine cases of instability in a series of 57 patients.26 Only three had a stable functioning RSA at follow-up. Edwards et al. treated seven patients with instability. 18 Closed reduction was performed in two patients and open reduction with deltoid tensioning was performed in five cases. All were stable at follow-up.
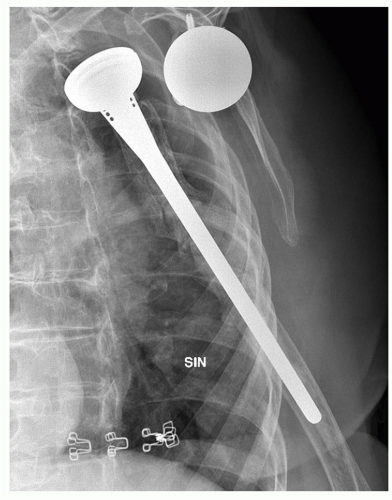
Since 1995, we have followed a strict protocol for treating instability of an RSA, and surgical factors to avoid instability have been defined. Deltoid tensioning is regarded as the key factor. In addition, all the humeral components are placed in neutral or a few degrees of anteversion to avoid instability. A dislocation occurring within 48 hours of surgery is treated with closed reduction and immobilization for 3 weeks. We believe that such a dislocation may be due to poor control of the deltoid muscle during the early postoperative period and not a reflection of poor tensioning. Dislocations occurring after 2 days are treated with open reduction, scar tissue removal and lengthening of the humeral component, either with a higher insert or a humeral lengthener (Figs. 23-1 and 23-2). Following this algorithm, all the patients were stable at last follow-up. Deeper, more constrained polyethylene inserts should be avoided since these result in increased polyethylene wear and complications. Stability can usually be restored without the need for these deeper constrained devices, which are regarded as salvage components.
Recently, some RSA designs in the market have introduced shallower inserts compared with the standard depth. These designs allow for better range of motion before impingement occurs, but significantly reduce the stability. It should be noted that when potential range of motion is increased, the stability is reduced. Therefore, it is important for the surgeon to be aware of the design features of the specific implant being used.
If there is a malpositioning of the implants, they have to be corrected (Fig. 23-3A, B). A retroverted humeral component may have to be put in neutral or in slight anteversion. From the author’s experience, this is rarely needed. If the glenoid component is placed too high and bone is protruding below the glenosphere, a levering-out effect can be seen, which needs to be corrected during revision. Another option is changing from a small to a larger diameter glenosphere. In all cases of instability, it is important to rule out the infection, since infection can result in instability.26
Surgical Technique
When the diagnosis of a chronically dislocated RSA is made in our group, the patient is scheduled for surgery within 1 to 2 weeks. We prefer the beach-chair position, and the incision from the previous procedure is used. Antibiotic prophylaxis is given for 3 days because the procedure is a revision. On exposure, the polyethylene insert is usually found to be worn, and it is removed. The glenosphere is inspected and if there are scratches on the surface, which are very common in our experience, it should also be replaced. Then, a release all around the
glenoid is performed and the scar tissue, particularly inferiorly, is removed. Six to eight biopsies are taken for microbiology. In order to increase deltoid tensioning, the humeral component is lengthened by inserting a metal lengthener or a higher insert. Usually, a 6 to 9 mm lengthening is necessary. A trial reduction is now performed.
glenoid is performed and the scar tissue, particularly inferiorly, is removed. Six to eight biopsies are taken for microbiology. In order to increase deltoid tensioning, the humeral component is lengthened by inserting a metal lengthener or a higher insert. Usually, a 6 to 9 mm lengthening is necessary. A trial reduction is now performed.
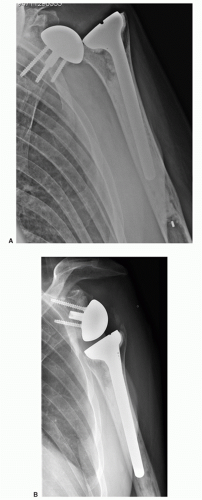 FIGURE 23-3. (A) Superior tilt of the glenoid component causing dislocation. (B) Revision of the glenoid component with bone graft resulted in a stable RSA. |
During trial reduction, the arm is placed in adduction and only a small gap between the components (1 to 2 mm) should be seen. Next, a longitudinal pull on the arm is performed and no separation between the glenosphere and the insert should be apparent (anesthesia without muscle relaxation is used to allow deltoid tensioning). Finally, the arm is put in extension and external rotation. In this position, the shoulder should be stable, but a small opening between the components of 2 to 3 mm anteriorly can be seen. If the stability is not satisfactory, the first step is to further increase the tension by lengthening the humeral component.
Lengthening of the humeral component may not be enough to create stability and the next step is to increase the size of the glenosphere or to put in an eccentric glenosphere, if available, to create more tensioning. Range of motion is then checked to see that enough room has been created, allowing the humeral component to glide over the glenosphere. Compared with an anatomical arthroplasty, more room is necessary posteriorly, anteriorly, and inferiorly.
Postoperatively, the patient wears a sling for comfort 1 to 2 weeks, but active range of motion rehabilitation is started the day after surgery. The patient is not allowed to push up from sitting to standing with the operated arm in the first 6 weeks after surgery.
Infection
Incidence
The mean rate of infection in 14 studies was 3.8%.68 More infections were seen after revision procedures (5.8%) compared to primary RSAs (2.9%).
Low-virulence organisms, such as Propionibacterium acnes, are a common cause of deep infection after RSA.68
In our series, we observed a high rate of infections (4,7%) in the first series of 277 RSA’s between 1995 to 2005. However, since 2006 only 7 infections (1%) have been diagnosed in 695 consecutive RSAs (Delta Xtend, DePuy, Warsaw, IN, USA). Thus, anatomical arthroplasty and RSA are associated with similar rates of infection.
Diagnosis
Diagnosis can be easy in some cases, but can also be very difficult and challenging. Radiographs, temperature, and blood tests can all be normal, and aspiration of joint fluid for microbiology analysis can be negative despite a deep infection. Topolski stated that there are no good preoperative or intraoperative investigations to detect who will have a positive intraoperative culture at the time of revision shoulder arthroplasty.58
Diagnostic clues from the patient history include pain at rest, which should be regarded as an infection until proven otherwise. The color of the skin should be examined since Propionibacterium infection can result in a very typical redbluish rash over the shoulder (Fig. 23-4). Fistulas may develop around the shoulder.
Regarding the analysis of blood samples, a recent systematic review by Berbari et al. concluded that interleukin-6 (which is rarely used) and C-reactive protein (CRP) are better diagnostic tools than sedimentation rate (ESR) and white blood-cell count.5 Thirty studies of hip and knee revision arthroplasties were assessed, and the diagnostic accuracy of CRP and ESR were analyzed. The sensitivity for CRP was 88% and specificity was 74%, compared with 75% and 70% for ESR. Piper et al. looked at shoulder implant infections and found poorer specificity (73%) and sensitivity (63%) for both CRP and ESR in diagnosing an infection compared with that seen in infected hip and knee arthroplasties.49
Aspiration of joint fluid, and tissue biopsies (open or arthroscopic) for culturing could be valuable to diagnose a periprosthetic infection. Biopsies have been found to be superior to aspiration and the author uses open biopsies (10 to 15 pieces) in complex cases.23 The biopsies are taken from various parts of the joint and around the implant. They are sent for culturing and it is important to keep the cultures for 3 weeks since Propionibacterium acnes grow slowly and need 2 to 3 weeks for incubation.2,34
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree