Complications of Instability Surgery
Robert J. Gillespie
Mark D. Lazarus
INTRODUCTION
There are three broad categories of recurrent instability: anterior, posterior, and multidirectional (MDI). Anterior instability remains the most commonly diagnosed and treated form of recurrent instability. Recurrent anterior glenohumeral instability occurs most often following a significant traumatic incident and is often referred to as recurrent traumatic instability. This traumatic event usually takes place with the arm in an abducted, extended, and externally rotated position. Glenohumeral dislocation reproduced in the laboratory demonstrates a severe and explosive event, supporting the destructive pathology noted in the shoulders of these patients. As many as 84% to 97% of these patients will have avulsions of the anteroinferior capsulolabral complex from the glenoid rim (the so-called Bankart or Perthes lesion).11,164,223,256 A wide array of factors can be responsible for failure of this repair (Table 6-1).
Posterior shoulder instability represents approximately 5% of all instability cases.216 It represents a continuum of problems that remains poorly understood.280 No single lesion is thought to be responsible for the development of posterior instability. Most researchers distinguish between acute traumatic dislocations and chronic atraumatic posterior instability. The former is typically caused by a single traumatic event, while the latter develops insidious laxity and instability over time. Rehabilitation of the rotator cuff, especially the infraspinatus, remains the first line treatment for posterior instability. If rehabilitation fails and symptoms persist, operative intervention may be indicated. Open surgical procedures for posterior instability can be divided into osseous, soft-tissue, or combination. Bony procedures include glenoid osteotomy, posterior bone block(reverse Eden-Hybbinette), and proximal humeral rotation osteotomy. Soft-tissue procedures include posterior capsular shift, reverse Bankart repair, and reverse Putti-Platt procedures. Combination procedures incorporate elements of both categories.
MDI was originally defined by Neer and Foster in 1980.185 Their study group demonstrated instability anteriorly, posteriorly,
and inferiorly. Capsular redundancy was demonstrated intraoperatively and was eliminated with an open humeral-based capsular shift. Caspari first reported on arthroscopic techniques for MDI.39,172 His technique utilized multiple sutures to shift the posterior and anterior bands of the inferior glenohumeral ligament (IGHL) and anterior glenohumeral ligaments superiorly, thereby reducing capsular volume. Excessive capsular laxity is considered the primary pathogenesis of MDI. It can be congenital or acquired. Despite a general agreement that capsular laxity is the “essential lesion” of MDI, increased laxity alone cannot explain MDI which often occurs in the midrange of motion when capsular ligaments are loose. Other contributing factors may include concavity-compression (muscle forces of the rotator cuff) and geometric conformity of the glenohumeral joint provided by labrum and articular cartilage.39,172 Kim identified labral pathology in all of his patients with either MDI or posterior-inferior instability.127,129 Additionally, there is evidence that the amount of translation in symptomatic shoulders with MDI is not significantly different from the laxity found in painless shoulders with MDI.148,149 This implies that pathology other than capsular volume may contribute to painful MDI.148,150,170
and inferiorly. Capsular redundancy was demonstrated intraoperatively and was eliminated with an open humeral-based capsular shift. Caspari first reported on arthroscopic techniques for MDI.39,172 His technique utilized multiple sutures to shift the posterior and anterior bands of the inferior glenohumeral ligament (IGHL) and anterior glenohumeral ligaments superiorly, thereby reducing capsular volume. Excessive capsular laxity is considered the primary pathogenesis of MDI. It can be congenital or acquired. Despite a general agreement that capsular laxity is the “essential lesion” of MDI, increased laxity alone cannot explain MDI which often occurs in the midrange of motion when capsular ligaments are loose. Other contributing factors may include concavity-compression (muscle forces of the rotator cuff) and geometric conformity of the glenohumeral joint provided by labrum and articular cartilage.39,172 Kim identified labral pathology in all of his patients with either MDI or posterior-inferior instability.127,129 Additionally, there is evidence that the amount of translation in symptomatic shoulders with MDI is not significantly different from the laxity found in painless shoulders with MDI.148,149 This implies that pathology other than capsular volume may contribute to painful MDI.148,150,170
TABLE 6.1 Causes of Failure of Open Anterior Instability Repairs | ||||||
|---|---|---|---|---|---|---|
|
Rarely do we as surgeons proceed as confidently as when we operate for recurrent instability. For traumatic anterior or posterior instability, a surgeon can confidently inform his patient that his or her chances of returning to near normal function are greater than 90%.30,256 When instability surgery fails, however, that surgical confidence can deflate as fast as it had risen. Faced with the patient who has suffered multiple failures of instability surgery, we as surgeons can become thoroughly humbled. This chapter will explore the common complications after instability surgery, how to avoid these failures, and the techniques for recovery.
RECURRENCE OF INSTABILITY
Incidence and Background
The most common complication reported after surgical treatment for glenohumeral instability is recurrence of instability.30,37,96,121,161,202,223,238,253,292 The exact rate of instability recurrence depends on the specific surgical correction employed at the time of the index procedure as well as the direction of the instability, but ranges from 0% to almost 90%.15,30,33,78,118,164,202,203
Anterior
The most common complication reported after surgical repair for anterior instability is recurrence of instability.33,96,104,121,145,223,292 The exact rate of instability recurrence depends on the specific surgical correction employed at the time of the index procedure, but ranges from 0% to almost 90%.15,40,78,157,265 Others have cited other predisposing factors such as age, gender, and time from dislocation to surgery, as causes for the recurrence after surgery, regardless of open or arthroscopic techniques.202 The literature continues to evolve when evaluating anterior instability as techniques for treatment continue to change and improve. This has led to high variability in rates of recurrence in the literature after open or arthroscopic repair. Much of the variability probably relates to the wide array of different arthroscopic and open repair techniques, differences in surgeons’ experience, and short followup. Arthroscopic techniques for shoulder instability can be divided into several categories with some of the techniques used infrequently given the recent advancement of techniques and technology in the current state of shoulder instability surgery: metal fixation such as screws or staples, absorbable devices, suture-based repairs, and thermal treatment. Each technique offers unique advantages but each can also result in unique complications and causes for instability recurrence. Shaffer and Tibone reviewed recurrence of instability after arthroscopic surgery and found rates of 16% to 33% for staple capsulorrhaphy, 0% to 60% for transglenoid suturing, 0% to 37% for tack stabilization, and 0% to 30% for suture anchor repair.235 Few of these techniques except for suture anchor repair are used currently, but this rate of recurrence of instability is consistent in the more recent literature and is comparable to open repairs.6,7,18,30,84,86,94,126,139,141,145,181
Initial arthroscopic Bankart repairs were performed by staple capsulorrhaphy. Johnson’s staple repair technique, which formed the basis for many other subsequent approaches, had an initial failure rate of 21%.17,116 Other authors continued to report high recurrence rates after arthroscopic staple capsulorrhaphy.47,88,94,140,165,239,240,279 As a response to the problems of staple capsulorrhaphy, other investigators developed arthroscopic suture techniques,6,18,39,51,73,84,139,181,187,198,266 based on the transglenoid open Bankart repair procedures of Reider and Inglis.208 Manta’s review of 38 shoulders, stabilized with the arthroscopic transglenoid suture technique, demonstrated a 10% failure rate at 2 years and a 40% failure rate at a minimum 5 years of follow-up.163 This technique is infrequently done today and is not currently recommended. Another method developed for arthroscopic Bankart repair utilizes absorbable tacks for labral attachment. Even in experienced hands, the overall rate of instability recurrence is approximately 12% to 21%.233,246 As a result of high complication rates and the development of newer technology with suture anchors, the above described techniques are infrequently performed today and are not recommended.
The most common method currently for arthroscopic labral repair involves the use of suture anchors, either absorbable or permanent.30,40,197,245,246,264,272,273 Arthroscopic Bankart repair with suture anchors have been utilized with success ranging from 70% to 95%.12,30,33,113 Ide utilized absorbable anchors for acute Bankart repair in 55 athletes with no glenoid bone loss followed for 42 months with 93% success.113 Mazzocca studied collision athletes and found an 11% redislocation rate after a 37-month follow-up.167 Burkhart and DeBeer noted that the overall rate of recurrence for this technique for athletic patients with anterior glenoid defects was 89%. Without significant bone loss the recurrence rate dropped to 6.5%, similar to Ide’s study.33 Similarly, Bacilla
reported 91% return to athletic competition without redislocation in 32 patients12 and Kim reported only 4% recurrent instability in a group of 167 patients (53% contact athletes) followed for 44 months.124 Koss, however, reported 30% redislocation in 27 patients followed for 40 months with failure associated with more than five preoperative dislocations.136 Guanche reported 33% resubluxation or dislocation in 15 patients followed for 17 to 42 months.89 Recently, longer follow-up has been reported with Castagna and colleagues reporting a 23% recurrence rate after arthroscopic suture anchor repair. Interestingly, three of the seven occurred more than 6 years after their index procedure.40 Jones and colleagues showed an overall recurrence rate of approximately 15% in a pediatric population.118 Clearly, the trend in orthopedic surgery for anterior instability is toward arthroscopic stabilization but three recent meta-analyses bring this trend into question: Brophy and Marx performed a literature review examining recurrence after open and arthroscopic techniques and found that the overall rate was low for both, at 8% and 6%, respectively.30 Lenters and colleagues showed a significantly increased relative risk of recurrent instability, dislocation, and re-operation using arthroscopic techniques versus traditional open methods. A possible reason for the difference between the current conventional wisdom and this study is the fact that the search only included studies between 1966 and 2004, ending at the very beginning of the learning curve of arthroscopic stabilization.145 However, it could also be that for a small percentage of patients, arthroscopic techniques do not address all of the pathology, leading to recurrence in this select population. Hobby and colleagues performed a similar analysis, looking at all studies in the literature from 1985 to 2006 and after eliminating techniques such as transglenoid suturing and staples found that open and arthroscopic techniques yielded similar rates of recurrence at 2 years.104
reported 91% return to athletic competition without redislocation in 32 patients12 and Kim reported only 4% recurrent instability in a group of 167 patients (53% contact athletes) followed for 44 months.124 Koss, however, reported 30% redislocation in 27 patients followed for 40 months with failure associated with more than five preoperative dislocations.136 Guanche reported 33% resubluxation or dislocation in 15 patients followed for 17 to 42 months.89 Recently, longer follow-up has been reported with Castagna and colleagues reporting a 23% recurrence rate after arthroscopic suture anchor repair. Interestingly, three of the seven occurred more than 6 years after their index procedure.40 Jones and colleagues showed an overall recurrence rate of approximately 15% in a pediatric population.118 Clearly, the trend in orthopedic surgery for anterior instability is toward arthroscopic stabilization but three recent meta-analyses bring this trend into question: Brophy and Marx performed a literature review examining recurrence after open and arthroscopic techniques and found that the overall rate was low for both, at 8% and 6%, respectively.30 Lenters and colleagues showed a significantly increased relative risk of recurrent instability, dislocation, and re-operation using arthroscopic techniques versus traditional open methods. A possible reason for the difference between the current conventional wisdom and this study is the fact that the search only included studies between 1966 and 2004, ending at the very beginning of the learning curve of arthroscopic stabilization.145 However, it could also be that for a small percentage of patients, arthroscopic techniques do not address all of the pathology, leading to recurrence in this select population. Hobby and colleagues performed a similar analysis, looking at all studies in the literature from 1985 to 2006 and after eliminating techniques such as transglenoid suturing and staples found that open and arthroscopic techniques yielded similar rates of recurrence at 2 years.104
Recently, open coracoid transfer, specifically the Latarjet procedure, has been used as a primary instability surgery when there is significant bone loss along the anteroinferior glenoid. Allain and colleagues had at least a 10-year follow-up on all of their patients and had only one patient with occasional subluxations.2 Burkhart and colleagues had a 4.9% recurrence rate, whereas Walch and Boileau had a recurrence rate of 1%.34,265 Some authors have begun to perform this procedure through an all-arthroscopic technique reporting similar low recurrence rates.26,138 Mahirogullari and colleagues highlighted the major problem with these procedures, that is, the increased risk of complications not related to recurrence when compared with arthroscopic repair.161
Despite the increased risk of other complications, the low rates of recurrence in anterior stabilization procedures highlights the need to accurately diagnose the source of instability, regardless of the direction as one of the most common causes of recurrence after instability surgery of any type is incorrect procedure or diagnosis.
Posterior
Most authors cite posterior capsular redundancy as the most common intraoperative pathology in posterior instability cases, although varying degrees of labral pathology have been described.92,127 The wide recurrence range likely also depends on the sample group. The results of treatment are not often reported on one well-defined subgroup. Besides patients with unidirectional posterior instability, many patients with MDI have painful posterior subluxations, making this their primary direction. There is no general agreement regarding classification of posterior instability. Multiple variables, such as trauma, MDI, and voluntary or involuntary components are difficult to integrate into a reproducible accepted classification system. Are an offensive lineman with a posterior labral avulsion and mild posteroinferior redundancy and a gymnast with posterior labral fraying and a large posteroinferior capsular recess suffering from the same problem even if they both have a primary instability direction of posterior?
Nevertheless, posterior instability has been broadly classified into acute or chronic. Chronic can be further subdivided into “locked” (missed) and recurrent voluntary or recurrent involuntary. Structural abnormalities, including labral injury or rotator interval injury, may exist. Structural abnormalities may also include bony defects such as increased glenoid retroversion or posterior glenoid erosion.
The actual incidence of recurrent instability after open or arthroscopic posterior repair has been extremely variable and is dependent on the index procedure. Rates as high as 30% to 50% have been reported after an open procedure.258 There may be several reasons to explain the high recurrence rate. Unlike anterior instability, there appears to be no “essential lesion” of posterior instability. Recurrent posterior instability is thought to be a pathologic process incompletely understood with several etiologies making treatment more difficult. As would then be expected, the results of surgery for repair of unidirectional posterior instability are variable and often much less gratifying than those for anterior instability.
Boyd and Sisk reported their results of posterior capsular imbrications, with and without posterior transfer of the long head of the biceps tendon, and found no recurrences at longer than 2 years postoperative.28 Hurley and colleagues, on the other hand, reported a recurrence of instability rate of 72% after soft-tissue reconstruction for posterior instability.110 When Hawkins et al. reviewed their cases of posterior capsular and infraspinatus imbrications, they found a recurrence rate of 83%.98 Regardless of the technique used, the overall recurrence rate in that study was 50%. Tibone and Ting reported recurrence of instability in 6 of 20 patients who underwent staple posterior capsulorrhaphy.257 Bigliani and colleagues reported the results of posteroinferior capsular shift in 35 patients with posterior instability.21 At a mean follow-up of 5 years, only 4 patients suffered from recurrence. More recently, Wolf and colleagues reported on their open results citing a 19% recurrence rate with poor outcomes in those patients who had a chondral injury at the time of surgery.284
Recurrence of posterior instability after arthroscopic repair techniques is extremely variable and is likely linked to the learning curve that was initially associated with this procedure as well as the difficulty addressing all the potential sources of posterior instability. Rates of 0% to 50% have been reported.83,127,280 It is our belief that this procedure is now technically easier to perform through an arthroscopic technique versus an open technique and the recent literature on recurrence rate supports this: Kim and colleagues reported a 3% recurrence rate with high patient satisfaction after an average of over 3 years follow-up. They also noted the multiple pathologic lesions in these patients and that failure to address all of these may lead to recurrence.127 Englesma and Willems
recently reported on their arthroscopic results and found a 21% recurrence rate. Interestingly, their failures were all in patients who either had thermal capsulorrhaphy or had atraumatic ligamentous laxity.56 Savoie and colleagues reported a 3% recurrence rate in their patients with long-term followup after certain surgical techniques had been eliminated.229 In general, these studies support the decreased recurrence found in an arthroscopic versus an open procedure for posterior instability. When recurrence does occur after arthroscopic shoulder repair, it is usually secondary to incorrect diagnosis/patient selection, surgical errors, or inadequate rehabilitation, which will all be discussed in later sections.
recently reported on their arthroscopic results and found a 21% recurrence rate. Interestingly, their failures were all in patients who either had thermal capsulorrhaphy or had atraumatic ligamentous laxity.56 Savoie and colleagues reported a 3% recurrence rate in their patients with long-term followup after certain surgical techniques had been eliminated.229 In general, these studies support the decreased recurrence found in an arthroscopic versus an open procedure for posterior instability. When recurrence does occur after arthroscopic shoulder repair, it is usually secondary to incorrect diagnosis/patient selection, surgical errors, or inadequate rehabilitation, which will all be discussed in later sections.
Multidirectional instability
Overall, the rate of instability recurrence after open capsular shift for an appropriate diagnosis of multidirectional instability is low. In 1980, Neer and Foster reported 40 patients who had undergone capsular shift for multidirectional instability, with only 1 patient suffering a recurrence.185 Altchek et al. described recurrent instability (posterior) in 1 patient of 40 who underwent T-plasty Bankart repair for multidirectional instability (anterior and inferior).4 Cooper and Brems reported recurrence in 4 of 39 patients after capsular shift.45 More recently, Pollock treated 49 shoulders with open inferior capsular shift for MDI. There was a 4% recurrence after a 61-month average follow-up. Excellent or good results were found in 94% of their study group.201 Reports on recurrent instability after arthroscopic treatment of MDI are similar. Gartsman reported on 47 patients treated with multiple suture anchors for MDI with just 1 of 47 experiencing recurrent instability.72 McIntyre reported a 5% recurrence rate using multiple sutures.172 Baker and colleagues also reported on an athletic population that underwent arthroscopic treatment for MDI and found 91% satisfaction in 43 shoulders.14 Alpert reported on their results in patients with MDI with a labral tear and they found a 15% rate of recurrence.3
The challenge for us, as orthopedic surgeons, is to determine why recurrence occurs after surgery for instability and to identify this prior to any intervention. This challenge will serve as the basis for the remaining portion of this section which focuses on the causes of recurrent shoulder instability after operative treatment.
Etiology
Numerous causes may be responsible for recurrence of instability after previous surgical repair (Table 6-2). Although discussed individually, several of these situations may coexist in the same patient. In the patient with instability recurrence, the revision surgeon must consciously rule out each of these causes before choosing a course of action.
Incorrect Diagnosis
In an ideal world, every patient with recurrent traumatic anterior instability would present to the surgeon with a radiograph demonstrating the dislocation. In the absence of a radiograph, the patient would give a clear history of instability events directly related to positioning the arm in abduction, extension, and external rotation. Unfortunately, as is usually true in medicine, patients rarely read the textbook before giving their history. Deciding on the direction of instability, or differentiating unidirectional traumatic from multidirectional instability, can sometimes be a confusing task, and the diagnosis should be made by thorough history, examination, and radiographic analysis.
TABLE 6.2 Etiology of Recurrent Instability after Anterior Repair | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Accurate determination of the direction of instability is crucial for obtaining satisfactory results after instability surgery. Even Hippocrates recognized the importance of performing the corrective procedure at the precise location of instability and the worsening that might result from misdiagnosis1:
For many physicians have burned the shoulders subject to dislocation, at the top of the shoulder, at the anterior part where the head of the humerus protrudes, and a little behind the top of the shoulder; these burnings, if the dislocation of the arm were upward, or forward, or backward, would have been properly performed; but now, when the dislocation is downward, they rather promote than prevent dislocations.
If a patient with recurrent anterior instability is incorrectly diagnosed as having posterior instability, a posterior repair would result in continued or worsened anterior instability.15,37,104,143,164,253,292 Subsequent appropriate anterior repair would result in an excessively tight shoulder. Similarly, if an anterior repair is performed, but the true diagnosis is multidirectional or posterior instability, posterior displacement may be worsened (Fig. 6-1).
Hawkins and Hawkins reviewed cases of recurrent instability after surgical repair and attempted to retrospectively assign a cause to the repair failure.96 In 12 of 31 patients, the authors believed that the primary cause of surgical failure was in the diagnosis, usually a confusion of direction of instability or type of instability. McAuliffe et al., in an analysis of 36 patients with failed instability repairs, found that 15 of those patients had recurrence secondary to misdiagnosis.168 Norris and Bigliani determined that 9 of 42 patients with recurrent instability were incorrectly diagnosed, including 4 who underwent surgery on the incorrect side of the shoulder.190 Rockwood and Gerber thought that the cause of recurrent, postoperative instability in 68% of 57 reported patients was failure to recognize multidirectional instability.217 Burkhead and Richie analyzed 23 patients with postoperative instability and determined that, for 5 of 23, the diagnosis of multidirectional instability had been missed.36 Wolf studied open posterior capsular shift and labral repair in 44 shoulders from 2 to 22 years follow-up for posterior instability.287 His study
group consisted primarily of traumatic posterior subluxors or dislocators. Recurrence of instability was found in 19% of patients. All patients were examined under anesthesia and it was documented that 11 cases had MDI. In those cases with MDI, recurrence was 40% versus 10% for those patients with posterior inferior instability. The authors emphasized the need to document MDI at the time of surgery.
group consisted primarily of traumatic posterior subluxors or dislocators. Recurrence of instability was found in 19% of patients. All patients were examined under anesthesia and it was documented that 11 cases had MDI. In those cases with MDI, recurrence was 40% versus 10% for those patients with posterior inferior instability. The authors emphasized the need to document MDI at the time of surgery.
Failure to recognize MDI instead of unidirectional posterior instability may also lead to surgical failure. Patients with posterior instability typically complain of mild shoulder pain, mechanical symptoms (catching, clicking, and clunking), and laxity in positions of flexion, adduction, and internal rotation. Trauma with the arm in this position is usually described. They usually present in their teens or twenties. They may or may not have pain. Hawkins reported that 40% of patients with posterior subluxation had no complaints of pain.98 This was true even in the face of ongoing subluxation. Activity-related pain or discomfort is common and range from dislocation to repeated subluxations. Physical examination should confirm unidirectional posterior instability.
Failure to recognize glenoid hypoplasia or excessive retroversion is another cause for recurrence if one utilizes a softtissue only procedure. Standard radiographs, including AP, lateral, and axillary views should be obtained to rule out a retroverted, posteriorly eroded, or dysplastic glenoid. In the setting of failed arthroscopic repair for posterior instability, a computed tomography (CT) scan should be considered to assess glenoid version and posterior glenoid erosion. If greater than 20 degrees of retroversion is present a soft-tissue only procedure may lead to high recurrence.128 Magnetic resonance imaging (MRI) with gadolinium enhancement is useful to evaluate the posterior inferior caspsulolabral complex. Kim identified four types of posterior labral pathology identified on MR arthrogram.
They also found that retroversion of the chondrolabral glenoid was present in posterior instability (5 to 8 degrees) when compared with controls (1.7 to 2.9 degrees). Failure to recognize labral pathology and/or chondrolabral retroversion may lead to increased recurrence.128,130
Once MDI and anterior instability have been ruled out, the examiner must first attempt to answer two questions. First, what is causing the symptoms? Is it true posterior instability or is there another potential cause for his symptoms? Second, what is the pathology that accounts for the symptoms? These are best assessed using clinical examination and history.
Clinically, recurrent subluxation typically presents as achy activity-related pain exacerbated by overuse. A history of trauma and volitional instability should be sought. Other potential causes for posterior shoulder pain include suprascapular nerve compression, Bennet lesion (posterior glenoid spur), quadrilateral space syndrome, osteoarthrosis, tumor, scapular winging, or cervical radiculopathy.
Physical examination attempts to reproduce symptomatic posterior translation. The signs, however, may be nonspecific. Athletes may have non-pathologic posterior humeral head translation of 50% and little discomfort. If the patient has painful posterior translation, the position of the arm and scapula should be noted. Patients with true posterior instability typically demonstrate subluxation with the arm in 80 to 90 degrees of forward flexion. Any inferior component to the instability is noted as it implies either rotator interval laxity or a redundant inferior capsule. Regardless of the test performed, it is critical to demonstrate reproducible symptomatic posterior instability in the clinic setting and to confirm the direction of instability in the operating room with examination under anesthesia.
For MDI, the reasons for instability recurrence after arthroscopic repair are similar to those after open repair. As stated previously, failure to identify the patient with MDI will lead to higher percentage failures. In the surgical suite, Oliashirazi found 83% sensitivity and 100% specificity to identify unilateral anterior instability using EUA with the affected arm tested in neutral, 40 and 80 degrees of external rotation and 20 degrees abduction. They also added the directions anterior inferior and posterior inferior in 70 to 80 degrees abduction to the more standard anterior, posterior, and inferior tests.195 Speer and colleagues have commented that their high rate of recurrence (21%), when compared with open procedures for instability, was related to an underestimation of the degree of overall capsular laxity at the time of initial arthroscopic treatment in those patients with atraumatic instability.244,246
Surgery for glenohumeral instability will also result in failure if the underlying diagnosis is not instability.190 Through recent teachings, we have correctly become more alert to the potential of instability as a cause of shoulder pain in the young population. However, not all shoulder pain in the young patient indicates occult instability. Unless the diagnosis of glenohumeral instability is truly indicated by history and
physical examination and is demonstrated by an examination under anesthesia, instability surgery should not be performed. Volitional dislocators should be identified and those with psychiatric problems must be identified. Connective tissue disorders such as Marfan’s or Ehlers-Danlos syndrome must be elicited. True scapular winging or dyskinesis must be diagnosed, if present.123,262 As stated previously, other diagnoses such as cervical radiculopathy, osteoarthrosis, nerve entrapment, and rotator cuff disease should always be ruled out before any type of instability surgery.
physical examination and is demonstrated by an examination under anesthesia, instability surgery should not be performed. Volitional dislocators should be identified and those with psychiatric problems must be identified. Connective tissue disorders such as Marfan’s or Ehlers-Danlos syndrome must be elicited. True scapular winging or dyskinesis must be diagnosed, if present.123,262 As stated previously, other diagnoses such as cervical radiculopathy, osteoarthrosis, nerve entrapment, and rotator cuff disease should always be ruled out before any type of instability surgery.
Incorrect Surgical Procedure
In many ways, an incorrect surgical procedure is directly related to an incorrect diagnosis: it is very difficult to perform the correct procedure without knowing the correct diagnosis. In general, there are two types of incorrect procedures in instability surgery: the first is a procedure that has been shown to be effective but is done for the wrong diagnosis. The second is a procedure that is done that has been shown to be less successful than others for the diagnosis it was designed to treat. In the following section, various procedures and the correct indications will be discussed for all types of instability.
ANTERIOR
In most patients with recurrent anterior instability, the pathologic defect is a tear of the anteroinferior glenoid labrum and origin of the IGHL, necessitating a repair of this defect to provide stability.33,78,145,164,220,256 In the literature, however, more than 150 different operative procedures have been described in the treatment of recurrent traumatic anterior instability. The “anatomic” surgical correction restores the labrum to its pre-injury anatomic position. Despite advances in arthroscopic treatment of instability, open treatment remains a reliable method with low recurrence.30,104,145,161 It may indeed be the preferred treatment for pathology not adequately treated by arthroscopic means, including soft tissue or bony deficiency. Other surgical techniques to correct instability are “nonanatomic” and can also be done in an open or arthroscopic fashion.26,138,180,265 These procedures attempt to compensate for labral or capsular pathology or bony deficiencies by using osseous blocks or soft-tissue tightening or advancements. No attempts are made to correct labral pathology. Examples include the Putti-Platt, which shortens the subscapularis, the Bristow or Latarjet, which osteotomize and transfer the coracoid to the glenoid rim and block translation, or the Magnuson-Stack which advances the subscapularis. The Latarjet procedure is the most commonly used today with the other techniques falling out of favor due to their higher risk of recurrence and long-term complications.27,34,138,265 Patients who have severe bony deficiencies or a deficient soft-tissue envelope may be incorrectly treated with an anatomic repair and may be better treated with a Latarjet, Bristow, or other grafting procedure.
For most patients who have recurrent anterior instability after a nonanatomic repair, the literature suggests that simply performing a Bankart repair has a high rate of success. Rowe et al. reviewed the results of surgical correction after a prior failure of instability surgery.223 In 84% of their patients, they found residual, unrepaired Bankart lesions at the time of revision surgery. With revision surgery, usually a Bankart repair, they were able to restore stability in 92% of patients. Hawkins and Hawkins found residual anteroinferior labral detachments in most of their patients who underwent surgery for recurrence of instability.96 Our experience with revision of instability surgery is that all of the pathology causing the instability was usually not corrected with the index procedure, thus an incorrect procedure as a result of a missed diagnosis was sometimes performed. An algorithm for revision instability was followed and will be presented later in the chapter.
Historically, coracoid transfer procedures often had similar to even higher recurrence rates compared with anatomic procedures, perhaps because of the increase in severity of the diagnosis leading to the nonanatomic procedure being performed. Several new studies, however, have shown improved results. Hovelius reviewed 118 cases over 15 years and found a 3.4% recurrent rate with high patient satisfaction.106 Allain and colleagues also reviewed 95 Latarjet procedures over 14 years.2 There were no redislocations and an 88% satisfaction rate. Similar results have been found in other European and North American studies with Burkhart reporting a 4.9% recurrence rate,34 Walch a 1% recurrence,265 Boileau and LaFosse having no recurrences, with Lafosse performing his all arthroscopically.26,138,289 Clearly, doing a “nonanatomic” procedure when it is not indicated, is difficult and if not done for the correct diagnosis (i.e., the wrong procedure), can be fraught with complications. In addition, revising nonanatomic procedures can be even more technically difficult and unrewarding: Young and Rockwood described in detail the surgical difficulties encountered in revising a failed Bristow procedure.290 Because of the loss of normal anatomic landmarks, associated problems of scar formation, hardware problems, subscapularis deficiency, and articular degeneration, the overall success rate at revision surgery was only 50%. Matsen has coined the phrase “lighthouse of the shoulder” to describe the coracoid process, meaning that the coracoid can guide a surgeon between the “safe” lateral side of the conjoined tendon and the “suicide” medial side.164 Revision surgery without this lighthouse, as in after coracoid transfer procedures, is technically demanding and dangerous. Lunn and colleagues reported on their results of failed Latarjet procedures utilizing the modified Eden-Hybinette procedure and reported 79% good to excellent results, further highlighting the difficulty in revising a “nonanatomic” procedure.157 Therefore, “nonanatomic” techniques should be not be used as a routine first line intervention for recurrent shoulder instability unless there is significant bone loss or a severe irreparable capsulolabral deficiency.
POSTERIOR
The most common surgical error for posterior instability is exactly the same as it is for anterior instability: a failure to address all pathology causing the instability.21,56,216,229 Procedures for posterior instability typically involve fixation of labral tears, posterior capsular shift, and in some instances, posterior glenoplasty to correct retroversion. The treatment, whether open or arthroscopic, should address all lesions.
Capsular laxity, at present, is felt to be the primary cause for recurrent atraumatic posterior instability. A redundant capsule is the most common finding at surgery. Cadaveric and biomechanical studies have reinforced the importance of the IGHL and rotator interval when evaluating posterior instability. Warren demonstrated in cadaveric sections damage to the anterior-superior capsule with posterior dislocation.275
He coined this injury the “circle” concept, emphasizing that capsular injury on both sides of the capsule is needed for dislocation to occur. Blaiser demonstrated that the coracohumeral ligament (CHL) contributed to posterior stability with the arm forward flexed to 90 degrees in neutral rotation. He also demonstrated that the IGHL contributed to posterior instability with the arm in internal rotation.24
He coined this injury the “circle” concept, emphasizing that capsular injury on both sides of the capsule is needed for dislocation to occur. Blaiser demonstrated that the coracohumeral ligament (CHL) contributed to posterior stability with the arm forward flexed to 90 degrees in neutral rotation. He also demonstrated that the IGHL contributed to posterior instability with the arm in internal rotation.24
Lesions of the labrum have been primarily implicated as contributing to traumatic posterior instability. Lippitt reported that loss of the posterior labrum reduced resistance to posterior inferior glenohumeral translation by 20%.150 Lesions of the superior labrum also contribute to instability. Cadaveric studies by Pagnani demonstrated increased anterior—posterior translation in cadavers with SLAP tears.196 Wolf and colleagues studied open posterior capsular shift and labral repair in 44 shoulders from 2 to 22 years follow-up. Their study group consisted primarily of traumatic posterior subluxors or dislocators. Reverse Bankart lesions were found in 18 shoulders and were the most common findings at surgery. Recurrence of instability was found in 19% of patients.284
More recently, Misamore reported on 14 athletes with unidirectional posterior instability treated with open posterior capsular shift and repair of labral defects.177 Of 14 patients, 13 had no instability or apprehension on follow-up. Fuchs found recurrence of 23% in 26 patients treated with posterior capsular shift with labral repair but 3 of 6 recurrences were in patients having previously undergone instability procedures.68 Kim presented their results after treating both the posterior capsule and the labrum arthroscopically and found only one of their patients had recurrent subluxations.127 They emphasized the need to use a surgical procedure that addressed all of the pathology of the shoulder. Savoie and colleagues also presented their results with arthroscopic stabilization and had a 3% recurrence rate at an average of 28 months.229 Incorrect/obsolete procedures such as suture tacks and thermal capsulorrhaphy were removed from the analysis yielding an improved outcome clearly showing that incorrect procedures can lead to poor results in shoulder instability surgery. Englesma and Willems also reported on recurrence rate after arthroscopic repair, with a rate of 21%. However, unlike Savoie, they did not remove the patients who had a procedure that was unsuccessful from their analysis, as three of the four patients who failed had a thermal capsulorrhaphy. They recommended abandoning this technique for the indication of posterior instability.56 Despite the variability in recurrence, posterior capsular shift with labral repair, if necessary, is the mainstay of surgical treatment of traumatic posterior shoulder instability if glenoid version is within normal limits. Good or excellent results can be obtained over short and intermediate terms if the correct surgical procedure is performed.
It is unclear how much of a role increased glenoid retroversion accounts for recurrent posterior subluxation.29,68,75,110,207 If a patient suffers recurrence of instability after a soft tissue procedure, osseous abnormality should be investigated. Fuchs identified posterior IGHL complex redundancy in 68% and lesions of the posterior labrum in 50% of 26 patients treated with open posterior capsular shift and labral repair.68 Glenoid retroversion was 12 degrees in recurrent subluxors versus 6 degrees in stable shoulders. Some studies have confirmed increased glenoid retroversion in patients with posterior subluxation while others have discounted it.29,68,75,207 The most common osseous procedure performed is posterior glenoid osteotomy. Preoperatively, a CT scan is indicated to accurately evaluate glenoid version. If greater than 20 degrees of retroversion is found, a posterior opening wedge osteotomy is indicated as part of the revision procedure (Fig. 6-2). Scott reported the use of posterior glenoid osteotomy to treat recurrent posterior instability.232 In his initial report on three patients, one of the three suffered from anterior instability postoperatively. After using a posterior glenoid osteotomy, Norwood and Terry had no recurrences in patients who had a traumatic etiology.192 Hawkins used CT scan to analyze shoulders after posterior glenoid osteotomy.95 He noted several potential complications, including undercorrection of version, intraarticular fracture, graft extrusion, and osteoarthritis. The rate of instability recurrence was 17%. Osseous procedures alone often leave a
redundant inferior capsular pouch or labral pathology, which may account for their high rates of recurrence. Wellmann and colleagues recently examined the biomechanics of bone block procedures and found that the posterior bone block repaircapsulorrhaphy overcorrects posterior translation and does not effectively restore inferior stability, whereas the arthroscopic posterior Bankart repair restores posterior and inferior laxity of the intact joint. They recommended an arthroscopic posterior capsulolabral repair as it more precisely restores posterior and inferior glenohumeral joint laxity.278 As such, bony block procedures and osteotomies have slightly fallen out of favor secondary to the high success rate of arthroscopic procedures for posterior instability.
redundant inferior capsular pouch or labral pathology, which may account for their high rates of recurrence. Wellmann and colleagues recently examined the biomechanics of bone block procedures and found that the posterior bone block repaircapsulorrhaphy overcorrects posterior translation and does not effectively restore inferior stability, whereas the arthroscopic posterior Bankart repair restores posterior and inferior laxity of the intact joint. They recommended an arthroscopic posterior capsulolabral repair as it more precisely restores posterior and inferior glenohumeral joint laxity.278 As such, bony block procedures and osteotomies have slightly fallen out of favor secondary to the high success rate of arthroscopic procedures for posterior instability.
Some investigators have reported better results and lower recurrence rates with posterior instability repairs while others have not. Fronek et al. reported 11 patients who underwent posterior capsulorrhaphy with or without posterior bone block and found recurrence of instability in only 1 of those patients.66 In 1984, Hawkins et al. reported a recurrence of instability rate of 41% after posterior glenoid osteotomy, posterior capsular plication, and infraspinatus imbrication.98 As stated previously in this section, recent work examining arthroscopic techniques have shown results similar to anterior instability repair for posterior instability.56,177,203,205,229
Careful attention to all the supporting structures of the shoulder, including the rotator interval, the anterior-superior labrum, and its attached superior glenohumeral ligament (SGHL), the CHL, the IGHL complex, and the infraspinatus, the glenoid, in addition to the posterior labrum and capsule, should allow excellent outcomes to be achieved. Failure to address or incorrectly treat all pathologies with the index procedure will often result in a higher recurrence rate and a more difficult revision in the future.
MULTIDIRECTIONAL INSTABILITY
The pathology of MDI that can be addressed arthroscopically includes increased capsular volume, labral deficiencies, and a deficient rotator interval. Failure to address these variables may result in a technical failure. Suture “pinch-tuck” imbrication and pinch tuck plication of the capsule to the labrum combined with rotator interval closure is an effective method for achieving these surgical goals. Kim reported good or excellent outcomes in 30 of 31 patients studied over 51 months using this technique.129 Gartsman was 94% successful with 47 patients studied over 35 months utilizing these techniques.72 Treacie and Savoie reported on 25 patients with MDI after arthroscopic stabilization followed for 5 years with 88% satisfaction and 12% resubluxation but no dislocation.260
Surgical intervention begins with an examination under anesthesia. Cordasco studied patients with isolated posterior or inferior labral tears but no clinical instability.46 On EUA all had posterior instability. MDI, if present, should be confirmed and the direction of maximal translation recorded and correlated to the patients’ symptoms. Failure to identify MDI may lead to recurrence. Arthroscopically, attention is paid to defects in glenoid concavity or other bony pathology. The posterior inferior labrum is thoroughly assessed. Lesions in this location may vary from labral tears to more subtle deep lesion on the chondrolabral junction (Kim’s lesion).128 Kim’s lesion may be evident after liberating the superficial chondrolabral surface and thus exposing the loose underlying labrum. Failure to rectify all potential pathology may lead to recurrence.
Suture anchor capsulorrhaphy restores the posterior inferior labral height and capsular tension. In the revision situation, the repair may be performed arthroscopically or open. The repair may be augmented with suture capsulorrhaphy. Kim recommends augmenting the repair with a posterior capsular shift, anterior capsular shift, and RI closure if anterior translation and/or inferior translation coexist. He studied 31 patients over 51 months. Thirty of thirty-one had good or excellent results by the Rowe grading system with 3% recurrent instability.128,130 Williams studied 27 shoulders over 5 years treated with posterior suture anchor capsulorrhaphy and found 8% recurrence of instability.280 Mair studied nine patients treated in like fashion with no recurrence at minimum 2-year followup.162 Goubier treated 11 patients for posterior instability with suture anchor capsulorrhaphy and had no recurrence of instability at 34 months.83
Although there are several techniques available for arthroscopic suture capsulorrhaphy, either with or in the absence of a labral lesion, we prefer a “pinch tuck” technique. Anchors are placed percutaneously via a posteroinferior (“seven o’clock) or posterosuperior (“Port of Wilmington”) portal. The anchors are placed at the chondral-labral junction. Through the posterior portal a curved suture passing device is introduced and pierces the capsule approximately 1 cm lateral and inferior to the labrum. The hook then re-enters the capsulolabral junction and the sutures are tied arthroscopically. Care is taken to incorporate the posterior IGHL and to achieve a shift of the capsule superiorly. Wolf reported on 14 patients treated with either suture anchor capsulorrhaphy or suture capsulorrhaphy with recurrence in 1 patient over 33 months.284 Posterior capsular redundancy was found in all patients and labral pathology was present in 86%. Provencher reported on 35 patients treated likewise with a follow-up of 25 months and found good or excellent results in 31 of 35. There were five recurrences.203
Recurrence of instability after capsular shift can also occur in the anterior or posterior directions. If the patient indeed has recurrent multidirectional instability, consideration may be given to combined anterior and posterior approaches at the time of revision. Neer and Foster suggested this strategy in their initial description of the inferior capsular shift procedure for multidirectional instability.185 Specifically, they recommended Bankart repair, if necessary, through an anterior approach, with a concomitant posterior approach for capsular shift. The technique is also useful, however, in the absence of a Bankart lesion. Through the posterior approach, complete access is gained to the posterior and posteroinferior capsule. From anteriorly, the anteroinferior, anterior, and rotator interval capsular regions can be addressed. Finally, instability recurrence in multiple directions may be a good indication for arthroscopic revision, as the anterior, inferior, and posterior aspects of the joint can be equally accessed in a non-destructive manner.
Postoperatively, these patients are placed in a neutral position brace with the arm positioned in neutral external rotation, but with the entire humerus and shoulder girdle superiorly displaced. This brace is maintained for 6 weeks, with the patient performing abduction and external rotation isometrics in the cast. At 6 weeks postoperative, the brace is removed and a
sling is placed. The patient is permitted to remove the sling for activities of daily living, but are encouraged to wear the sling for activities during which the arm may be expected to hang to gravity. At 10 weeks postoperative, the patient is begun on a gentle, supine, active-assisted motion program, rotator cuff strengthening against resistance, and a scapular stabilization and balancing program. Contact athletics and heavy lifting are restricted for 1 year.
sling is placed. The patient is permitted to remove the sling for activities of daily living, but are encouraged to wear the sling for activities during which the arm may be expected to hang to gravity. At 10 weeks postoperative, the patient is begun on a gentle, supine, active-assisted motion program, rotator cuff strengthening against resistance, and a scapular stabilization and balancing program. Contact athletics and heavy lifting are restricted for 1 year.
Technical Error
As much as we all wish to perform the perfect surgery in each and every case, there are times when the procedure does not proceed exactly as anticipated. The goal of the Bankart procedure is repair of the anterior glenoid labrum and IGHL to the glenoid rim. Although the surgeon may set out to perform a Bankart repair, difficulty with the exposure or unfamiliarity with the anatomy may result in the surgical goals being left unaccomplished.
It may be difficult to initially determine the cause for recurrence of instability in these cases. The index operative note may describe a Bankart-type repair as intended. If the integrity of the anteroinferior glenoid labrum and IGHL is not restored, a Bankart repair was not accomplished and instability recurrence is predictable. Bartl and colleagues demonstrated a low 11% recurrence rate after revising failed index instability cases using only arthroscopic techniques.16 Given this high level of success, it is likely that a large number of these index procedures had a recurrence due to technical error.
Technical errors leading to instability recurrence also plague non-Bankart repairs. For the Latarjet or Bristow procedure, correct placement of the transferred coracoid is essential for success.106,108 If the coracoid tip is secured too medial or superior on the glenoid neck, recurrent instability would be expected. If the procedure is to be successful, the transferred coracoid process must be placed at the anteroinferior quadrant to act as a bone block against anteroinferior humeral translation. A surgeon cannot rely on the “sling” of conjoined tendon to prevent humeral subluxation. In this section, we will briefly outline the major technical errors that occur in instability surgery, regardless of the diagnosis (anterior, posterior, MDI).230
FAILURE TO RESTORE GLENOID CONCAVITY
The shoulder is often described as inherently unstable owing to the shallow glenoid fossa. Relative to the acetabulum, the glenoid fossa is shallow. However, just as a golf ball on a tee, the humeral head gains a great degree of stability from its position within a concave glenoid fossa, and should actually be considered inherently stable. Howell and Galinat determined the depth of the glenoid fossa to be 9 mm in the superior to inferior direction and 5 mm in the anteroposterior direction.109 Half of the depth was attributed to the effect of the glenoid labrum, with the other half coming from the combined effect of the bony glenoid structure and the peripherally thickened chondral surface. This depth confers a great deal of stability to the glenohumeral articulation.
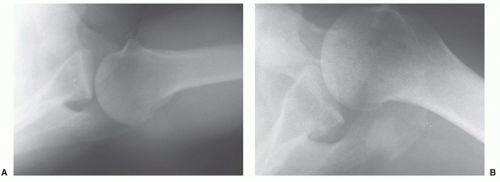
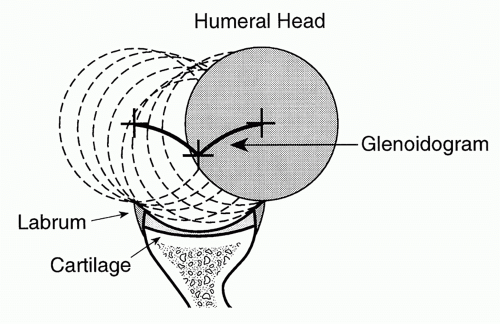
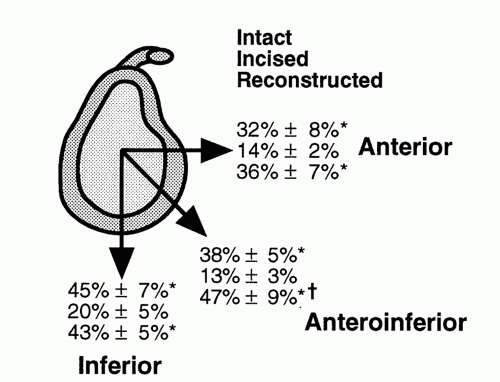
Even without ligamentous support, glenoid concavity plays a surprisingly effective role in providing glenohumeral stability. Lippitt et al. defined the concavity—compression mechanism of glenohumeral stability as the combined stabilizing effect of a spherical humeral head contained in a deep glenoid fossa, held there by muscular compressive action.149 These investigators used a graphic representation, referred to as the glenoidogram, to define glenoid depth. The glenoidogram demonstrates that lateral displacement of the humeral head is first necessary before anterior translation can occur (Fig. 6-3). They also used the stability ratio, a factor defined by Fukuda et al. as the humeral translating force required to cause a glenohumeral dislocation divided by the humeral compressive load maintaining stability, multiplied by 100, to analyze the effectiveness of glenoid concavity in promoting stability.69 Normal glenoids were noted to have significant concavity, equating with an ability to provide a tremendous stabilizing effect (stability ratios as high as 63%). Excising the glenoid labrum caused a reduction in the stability ratio of approximately 20%.
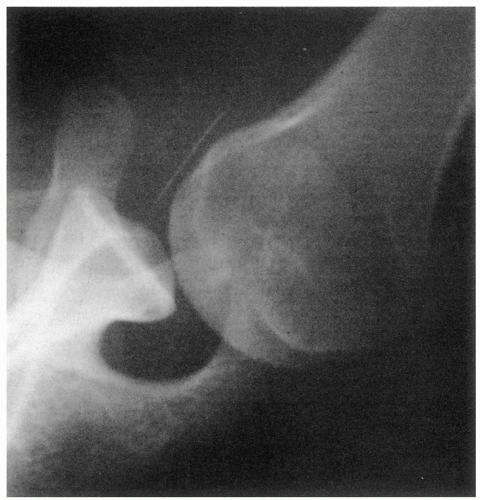
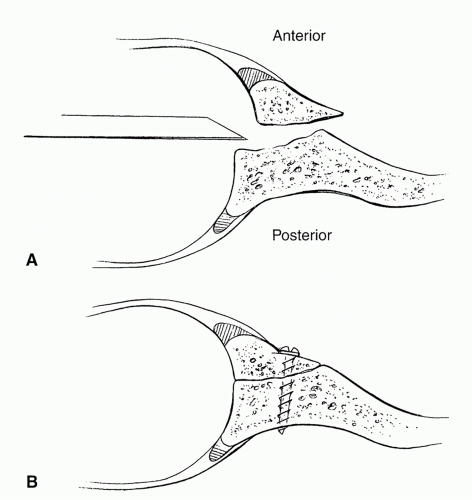
To relate the concept of concavity-compression more directly to the diagnosis of recurrent traumatic anterior instability, Lazarus et al. measured glenoid concavity and stability ratios before and after the creation of an anteroinferior glenoid chondral-labral defect.143 This defect was designed to be similar to that which might be found after numerous
anterior glenohumeral dislocations (Fig. 6-4). This investigation demonstrated significant reduction in the effectiveness of concavity-compression after creation of the instability defect. Glenoid concavity and stability ratios could be normalized with a simulated surgical reconstruction of the glenoid concavity (Fig. 6-5). Halder confirmed previous studies that suggested that the stability ratio and effective depth of the glenoid socket were linearly correlated.91 As compressive loads increased, the stability ratio decreased. Finally, Itoi performed a cadaveric study in which osteotomy of the anterior-inferior glenoid was performed and then the Bankart lesion repaired. Stability to anterior translation was decreased significantly after the repair if the osseous lesion exceeded 21% of glenoid width.115
anterior glenohumeral dislocations (Fig. 6-4). This investigation demonstrated significant reduction in the effectiveness of concavity-compression after creation of the instability defect. Glenoid concavity and stability ratios could be normalized with a simulated surgical reconstruction of the glenoid concavity (Fig. 6-5). Halder confirmed previous studies that suggested that the stability ratio and effective depth of the glenoid socket were linearly correlated.91 As compressive loads increased, the stability ratio decreased. Finally, Itoi performed a cadaveric study in which osteotomy of the anterior-inferior glenoid was performed and then the Bankart lesion repaired. Stability to anterior translation was decreased significantly after the repair if the osseous lesion exceeded 21% of glenoid width.115
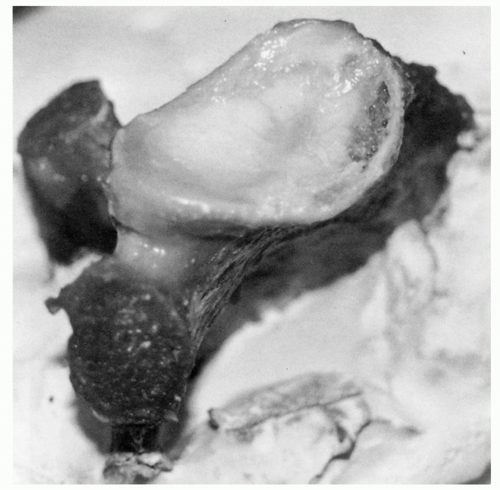 FIGURE 6-4. Surgically created anteroinferior glenoid labral and chondral defect to simulate the findings of glenoid concavity loss in recurrent, traumatic anterior instability. |
Larger concavity defects occur with fracture of the glenoid rim. It has been well reported that glenoid rim fractures are associated with recurrent anterior instability.15,137,141,158,164 Treatment options in the face of a glenoid rim fracture or deficiency include excision of the fragment and capsulolabral repair to the remaining glenoid rim (Fig. 6-5) , mobilization and direct internal fixation of the anterior glenoid fragment, coracoid transfer, or bone grafting of the anterior glenoid. Most authors recommend some type of osseous reconstruction if the deficiency constitutes more than 25% of the glenoid width.15,77,180,204,292
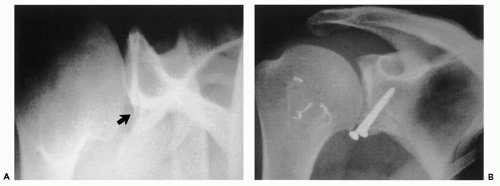
The accurate preoperative evaluation of a potential clinically significant osseous glenoid lesion is critical. Special radiographic studies, including a Garth view and a West Point axillary view, should be obtained. Even with good quality images, however, only large or distinct osseous fragments may be visible. A CT scan may be needed to adequately visualize and size a glenoid rim defect. Sugaya et al. used CT to evaluate 100 shoulders with recurrent unilateral glenohumeral instability and found that 90 had pathologic lesions. Fifty had osseous defects and forty had blunting of the normal glenoid contour suggesting compression or erosion at the glenoid rim.250 Glenoid rim deficiency of less than 20% of the articular width can possibly be effectively treated by simple repair of the capsulolabral complex into the defect. If the defect involves more than 20% to 25% of the glenoid articular width, however, it must be repaired or reconstructed for successful revision surgery. Failure to account for and reconstruct an anterior glenoid rim fracture can be a cause for instability recurrence after surgery15,77,141,158,202,204,250,253 (Fig. 6-6A).
Gerber has reported work on the effect of loss of the anteroinferior glenoid rim on stability.74 Instead of measuring the percent loss of the glenoid rim, he recommends measuring the shortest distance from the glenoid rim just superior to the defect to the intact rim at the inferior aspect of the defect. In his study, if this distance was greater that 15 mm, the stability to translational force was decreased by over 60%. More importantly, the stability could not be corrected by ignoring the osseous lesion and repairing the capsule and labrum into the defect. Burkhart studied glenoid bone loss and found that 25% to 45% of the glenoid must be missing to create an “inverted pear” glenoid.33,34 and 35 He showed that arthroscopic Bankart repair resulted in a redislocation rate of 4% without bony defects and that the rate of redislocation increased to 61% if an inverted pear was present. Bone defects in contact athletes resulted in an 89% redislocation rate versus 6.5% redislocation if no glenoid defect existed. Burkhart further showed that the degree of bone loss can be determined arthroscopically by measuring the distance from the bare spot of the glenoid to the posterior rim. This distance is almost identical to the distance from the bare spot to the anterior rim. The percentage of bone loss can therefore be determined. If greater than 25% bone loss exists, the authors recommend consideration of glenoid osseous reconstruction or coracoid bone block procedure.35
If, during revision surgery, the residual bone fragment appears viable, direct internal fixation of the fragment should be performed (Fig. 6-6B). Depending on the condition and size of the fragment, as well as its ability to be osteotomized
and mobilized, it can be repaired arthroscopically or open. For arthroscopic repair, 4.0 mm cannulated screw or suture fixation is possible, our preference being screw fixation. The fragment is mobilized while viewing via the anterosuperior portal. A quarter inch osteotome can be placed through the anteroinferior portal. Screws are usually placed percutaneously and extra-long guide wires are used (Fig. 6-7). For suture anchor fixation, smaller bone lesions are easily fixed by anchors placed inferior and superior to the fragment, indirectly reducing it. For larger fractures, this technique cannot be used as it will posteriorly tilt the fragment relative to the glenoid articular surface. If suture fixation is desired, anchors are placed in the fracture bed and the sutures are passed around both the osseous fragment and the labrum. It is helpful to pass all sutures first, prior to tying, as this permits access to the medial aspect of the osseous piece.
and mobilized, it can be repaired arthroscopically or open. For arthroscopic repair, 4.0 mm cannulated screw or suture fixation is possible, our preference being screw fixation. The fragment is mobilized while viewing via the anterosuperior portal. A quarter inch osteotome can be placed through the anteroinferior portal. Screws are usually placed percutaneously and extra-long guide wires are used (Fig. 6-7). For suture anchor fixation, smaller bone lesions are easily fixed by anchors placed inferior and superior to the fragment, indirectly reducing it. For larger fractures, this technique cannot be used as it will posteriorly tilt the fragment relative to the glenoid articular surface. If suture fixation is desired, anchors are placed in the fracture bed and the sutures are passed around both the osseous fragment and the labrum. It is helpful to pass all sutures first, prior to tying, as this permits access to the medial aspect of the osseous piece.
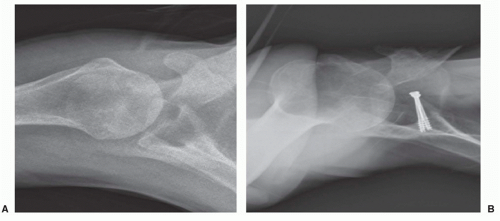 FIGURE 6-7. Malunited anterior glenoid rim fracture (osseous Bankart lesion) (A) treated with arthroscopic mobilization and repair (B). |
For open repair, we alter our standard Bankart approach by dividing the subscapularis and capsule as two distinct layers. The subscapularis is divided approximately 1 cm medial to the lesser tuberosity. Then, using sharp dissection or an electrocautery, the subscapularis tendon is elevated, in a medial direction, from the underlying capsule. The tendon must be freed in a medial direction past the glenoid rim fragment. The anterior capsule is then incised, allowing visualization of the glenoid articular surface. The glenoid fragment is usually found partially healed to the anterior glenoid neck and requires mobilization (Fig. 6-8A). The osseous bed is then prepared by a high-speed burr, and the fragment is repaired with bicortical lag screws, taking care to not leave the screws long posteriorly, where they may injure the suprascapular nerve (Fig. 6-8B). Usually, the anterior glenohumeral ligaments are attached to the osseous fragment and, therefore, are restored with union of the repair.
If, however, the fragment has eroded or appears nonviable, the glenoid rim must be reconstructed. The current treatment of choice for us and within the literature is a Latarjet coracoid transfer procedure. This can be done in an open or, more recently a few groups have published on an arthroscopic technique.26,138 The techniques and results for this procedure have been discussed previously and recurrence in the most recent literature remains low, ranging from 0% to 4.9%.26,34,138,265 Usually, we perform this procedure if the glenoid bone loss is less than or equal to 25%.
If bone loss on the anteroinferior glenoid is greater than 25%, there are two other bone grafting options: nonarticular bone graft and osteochondral allograft. Gerber has discussed reconstruction of the glenoid rim by placement of autogenous iliac crest graft, secured with bicortical screws, and fashioned to match the curvature of the native glenoid. In a preliminary report, he found the technique restored stability in 12 of 13 patients, with the final patient having questionable recurrence of subluxation only.74 In a similar study, Gill reconstructed the anterior glenoid with iliac crest bone graft in 12 patients with CT confirmed anterior glenoid bone loss. There was no recurrence in any patient at average 2-year follow-up. The only patients who developed progressive degenerative change were those who had some degree of degeneration preoperatively.78 Other authors echo these results: Bodey and Denham,25 Haaker,90 and Hutchinson111 all reported high patient satisfaction with a low recurrence rate for iliac crest grafting. Warner reported on 12 patients with anterior-inferior glenoid deficiency, who underwent intraarticular reconstruction of the anterior-inferior glenoid utilizing tricortical iliac crest autograft and capsular shift. At follow-ups ranging from 24 to 61 months, there were no reported cases of instability and CT confirmed osseous union absent arthritic changes.271
Our preference in these difficult situations is to use autogenous bone to fashion a graft for the rim, similar to Gerber. The surgical approach is as described earlier. The remaining atrophic glenoid fragment is excised, taking care to preserve the full length of the anterior capsuloligamentous structures. A pine cone burr is used to freshen and prepare the bed. A tricortical graft is harvested from the iliac crest. With a pine cone burr, the graft is fashioned to approximately conform to the curvature of the glenoid. If sufficient capsular length exists to place the graft in an extracapsular position, sutures of no. 2 Polydek are placed under the graft for later capsulolabral repair (Fig. 6-9A). The graft is then secured with bicortical lag screws, taking care to closely observe the articular surface for screw penetration and to not leave the screws long posteriorly, where they may irritate the suprascapular nerve. Finally, the pine cone burr is again used to complete fashioning of the graft in situ (Fig. 6-9B). With use of the previously placed sutures, the capsule is repaired directly to the native glenoid rim, leaving the bone graft in an extracapsular position (Figs. 6-9C and 6-10). If capsular repair to the host glenoid-graft junction results in excessive loss of external rotation, drill holes are placed in the rim of the graft and the capsulolabral complex is repaired to the rim of the graft. The subscapularis and capsule are then closed side-to-side. The postoperative regimen is as previously described for Bankart repair.
Finally, an osteochondral allograft can be used to reconstruct large anteroinferior glenoid defects. Our recent study examining failed instability repairs reported on the use of this procedure in two patients, successfully eliminating instability in both (Fig 6-11). Shah and colleagues have shown early success using allograft for glenoid defects larger than 25%.236 Provencher and colleagues have begun to use distal tibia osteochondral allograft with similar success.204 Advantages of allograft over autogenous iliac crest graft include the ability to near-anatomically size the glenoid rim, lack of donor-site morbidity, the presence of a smoother articulating surface, and the presence of labral and capsular tissue on the graft to assist in the reconstruction of combined osseous, chondral, labral, and capsular deficiencies. Clearly, the disadvantages are the theoretical possibility of disease transmission and the cost. There are also concerns about less consistent osseous incorporation as compared with autograft. We have recently begun using allograft as our preferred option when bone loss on the glenoid side is greater than can be treated with a coracoid transfer procedure, usually around 40% bone loss. Even in extreme situations, such as combined with a hemiarthroplasty, graft incorporation appears to be good (Fig. 6-12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree