Complications of Arthroscopic Subacromial Decompression and Acromioclavicular Joint Resection
Ilya Voloshin
Kevin J. Setter
Sean F. Bak
Louis U. Bigliani
In the past decade, we have seen an exponential increase in arthroscopic surgery of the shoulder. Consequently, complications related to these arthroscopic procedures have also increased. These complications can be divided into two categories: complications related to the arthroscopic techniques in general and those to specific arthroscopic procedures. The goal of this chapter is to discuss the complications specific to arthroscopic subacromial decompression (ASD) and acromioclavicular (AC) joint resection, as well as to provide clinical advice for prevention and treatment of these complications.
OVERVIEW OF ARTHROSCOPIC SUBACROMIAL DECOMPRESSION
In 1972, Neer described subacromial impingement syndrome (IS) of the shoulder (1). The principles of open subacromial decompression include resection of the acromial spur, coracoacromial ligament, inflamed hypertrophic bursa, and when indicated, the distal clavicle. In 1987, Ellman described the technique for arthroscopic subacromial decompression while maintaining the treatment principles set forth by Dr. Neer (2). ASD has proven to be a reliable procedure with success rates being equivalent to open subacromial decompression (80% to 90%) (2, 3, 4, 5, 6, 7). The advantages of the arthroscopic approach include preservation of the origin of the deltoid muscle, a more rapid rehabilitation, and more pleasing results cosmetically. According to most reports, the complication rate of ASD has been the lowest with respect to arthroscopic procedures of the shoulder, ranging between 0.7% to 2% (8,9). However, the reported success rate of 80% to 90% points to a “failure” rate of 10% to 20%. The failure of a procedure may be a consequence of complications of treatment, which can be the result of preoperative diagnostic errors or intraoperative technical errors. However, the failure may also be the result of the intrinsic physiologic response of the patient and factors beyond the control of the surgeon and unrelated to diagnostic or technical errors, including worker’s compensation (4,10).
COMPLICATIONS AND FAILURE OF ASD
Diagnostic Errors
The failure of ASD can be multifactorial and a systematic approach is important in deciphering the factors responsible
for failures. The definition of a failed ASD would include at least one of the following: persistent pain, motion loss, weakness, and inability to return to an active life-style enjoyed prior to the onset of symptoms. Several investigators have attributed nearly 50% of acromioplasty failures to incorrect or missed diagnosis (4,10,11). It is important to differentiate IS from other conditions that may cause similar symptoms in the shoulder, such as glenohumeral instability, os acromiale, AC arthritis, cervical radiculitis, calcific tendonitis, adhesive capsulitis, and nerve compression.
for failures. The definition of a failed ASD would include at least one of the following: persistent pain, motion loss, weakness, and inability to return to an active life-style enjoyed prior to the onset of symptoms. Several investigators have attributed nearly 50% of acromioplasty failures to incorrect or missed diagnosis (4,10,11). It is important to differentiate IS from other conditions that may cause similar symptoms in the shoulder, such as glenohumeral instability, os acromiale, AC arthritis, cervical radiculitis, calcific tendonitis, adhesive capsulitis, and nerve compression.
Glenohumeral instability is common in younger patients, and especially in athletes involved in overhead activity sports (12). Ogilvie-Harris et al. (4) found that 25% of all diagnostic errors in their study were due to instability of the shoulder. The diagnosis of IS in this patient population should be thoroughly scrutinized. Patients with instability may have symptoms and signs of IS, most likely secondary to nonphysiologic kinematics of the shoulder and secondary bursitis. Internal impingement is also possible source of pain in these patients (13). Even though ASD would remove potential associated bursitis in these patients, it would also further destabilize the shoulder unless the capsular laxity and labral pathology are addressed at the same time.
Presence of os acromiale should certainly be sought when considering ASD (Fig. 14-1). Point tenderness over the midacromion is the most reliable sign of a symptomatic os. Currently, the treatment of os acromiale is controversial with some reports showing successful results following arthroscopic excision or near-total excision of mesoacromion without residual sequalae. This approach must be used with caution, realizing that there is no good solution to pain secondary to the loss of the deltoid origin and biomechanical force-couple responsible for shoulder function. The authors’ preferred treatment is coracoacromial ligament release and acromioplasty, which effectively decreases contact pressure between the greater tuberosity and acromion. We have consistently achieved satisfactory results with this method. Other authors have reported success using internal fixation supplemented by bone graft (14,15).
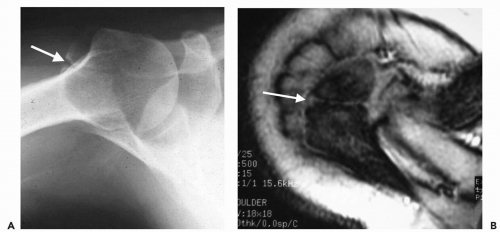 Figure 14-1 A: Axillary projection is typically the best radiographic view for demonstration of os acromiale (arrow). B: Axial magnetic resonance imaging in same patient. |
Degenerative symptomatic AC joint not only can contribute to IS (1), but also can be the cause of persistent pain after subacromial decompression unless addressed at the time of surgery (16). However, the resection of the distal clavicle should not be performed routinely for all patients who have IS, rather only in patients who are symptomatic in the region of the AC joint. For the failed ASD secondary to the AC joint symptoms, subsequent removal of the diseased AC joint offers a reasonable chance of success.
ASD is inappropriate for other potential diagnoses, such as cervical radiculitis, calcific tendonitis, adhesive capsulitis and nerve compression that can be confused with IS and will lead to persistent or exacerbated symptoms.
IS has become an increasingly common diagnosis for patients with painful shoulder. The authors recommend that each patient is approached thoroughly without expeditious attribution of their pain to IS. Complete history and a detailed physical examination must be performed specifically looking for other potential sources of symptoms in patients complaining of the anterosuperior shoulder pain, weakness, and difficulty with overhead activities. Appropriate radiographic workup as well as diagnostic injections are also important to differentiate potential other diagnoses. If the preoperative diagnosis was wrong or missed, ASD is bound to fail. It has been our experience that the most common entity misdiagnosed as IS is AC arthritis. In
younger patients, subtle instability can be missed. Differentiation of these processes can be simplified using selective injection of the subacromial space, AC joint, and glenohumeral joint. A positive impingement test (relief of pain during the Neer impingement maneuver after subacromial injection) is particularly useful in confirming the diagnosis of IS. It is essential that a systematic and thorough evaluation for other diagnoses is performed in the patient who has previously failed ASD.
younger patients, subtle instability can be missed. Differentiation of these processes can be simplified using selective injection of the subacromial space, AC joint, and glenohumeral joint. A positive impingement test (relief of pain during the Neer impingement maneuver after subacromial injection) is particularly useful in confirming the diagnosis of IS. It is essential that a systematic and thorough evaluation for other diagnoses is performed in the patient who has previously failed ASD.
Technical Errors
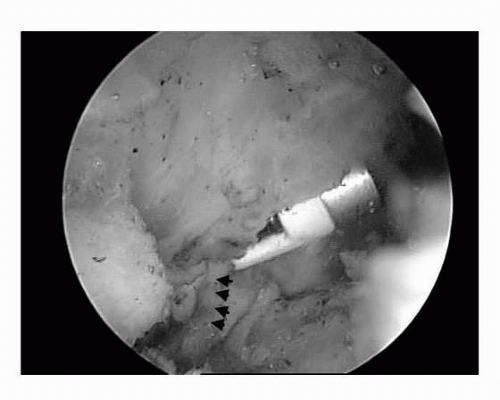
Perhaps one of the most common technical errors in ASD is the inadequate acromial resection (17). Poor visualization due to bleeding is probably the most crucial factor responsible for this complication. Visualization can be improved with good arthroscopic techniques, hypotensive anesthesia (18), and epinephrine in the irrigation fluid (19). Complete bursectomy is also very important for adequate visualization. The senior author successfully employed the “preemptive strike” technique where the electrocautery is passed just anterior to the coracoacromial ligament with the goal of cauterizing the acromial branch of the thoracoacromial trunk prior to the ligament detachment (Fig. 14-2). After this maneuver is performed, the ligament is taken directly off the anterior acromion without any major bleeding. A release rather than a resection of the coracoacromial ligament is performed, allowing for eventual healing of the ligament back to the bone in an elongated fashion. In the event of a massive rotator cuff tear, the ligament is left intact.
With the exception of younger patients with purely functional impingement and bursitis, we do a bony acromioplasty on the majority of patients with IS. To ensure adequate bone removal, the authors start the acromioplasty at the anterolateral corner of the acromion and set the resection level as a reference for the rest of the acromion. Removal of the spur along with 2 to 4 mm of additional bone anteriorly “raises the roof” of the acromion. Inadequate bone removal responsible for persistent IS usually can be successfully treated with revision ASD.
Although inadequate decompression is one of the most common technical errors, fracture of the acromion secondary to excessive bone removal has also been reported (20,21). Obtaining good quality preoperative radiographs, especially the outlet view, allows the surgeon to plan the appropriate amount of bone resection. The shape of the acromion can also be assessed, focusing on the curvature and the presence of the anterior spur. Again, starting the acromioplasty at the anterolateral corner of the acromion and setting the resection level is a useful technique to prevent this complication. These fractures can usually be treated with tension band fixation (21) or excision of the anterior fragment depending on its size.
Detachment of the anterior deltoid origin has been reported in literature (3,22) and can be a devastating complication causing anterosuperior subluxation of the humeral head and dysfunctional shoulder. Extreme care must be utilized to prevent this complication because there is no reliable treatment for anterosuperior humeral head subluxation. If diagnosed intraoperatively, the deltoid must be securely reattached to the anterior acromion to prevent chronic detachment and retraction, which is difficult to treat (22). The authors resect the anterior acromion just to the inferior attachment of the deltoid muscle (Fig. 14-3). Excessive anterior acromionectomy can also cause deltoid origin detachment. Chronic deltoid detachment is best treated with an attempt at soft tissue repair if an adequate cuff remains on the acromion. In the absence of a good soft-tissue stump, the deltoid is reattached via heavy nonabsorbable
suture through bone tunnels in the anteriolateral acromion. It is important to perform a complete subcutaneous and bursal sided mobilization of the deltoid prior to repair to ensure high-tissue quality.
suture through bone tunnels in the anteriolateral acromion. It is important to perform a complete subcutaneous and bursal sided mobilization of the deltoid prior to repair to ensure high-tissue quality.
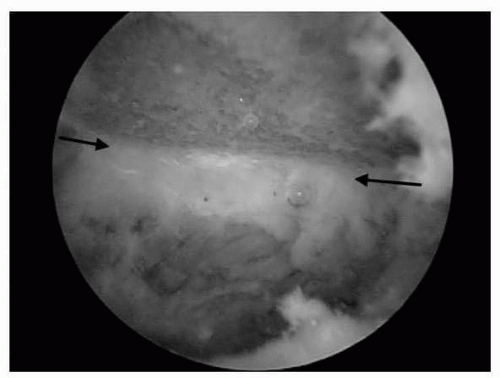 Figure 14-3 Arthroscopic view from posterior portal of left shoulder. The periosteal attachment of the deltoid (arrows) is left intact following thorough anterior subacromial decompression. |
Inadequate bursectomy can potentially be the cause of persistent bursitis and pain in patients after ASD. Not only is complete bursectomy important for visualization, but it is also important for removal of the inflammatory mediators, which play a role in the catabolic processes and continued degeneration in patients with IS (23). The study at our institution demonstrated increased levels of the inflammatory mediators in the bursae of patients with IS compared to controls (23). Gotoh et al. (24) identified increased levels of neuromediators responsible for pain generation in the bursae of patients with IS. Based on these studies, the authors believe that complete bursectomy is an important part of ASD.
Biceps tendon pathology must be addressed at the time of ASD. Our preference is to pull the biceps into the joint and look laterally down the biceps groove to visualize as much of the tendon as possible. This should be a part of the routine diagnostic glenohumeral arthroscopy. In general, where severe inflammation or greater than 50% fraying exists, the biceps is tenodesed. Less extensive disease is treated with debridement. The presence of biceps pathology can often be noted preoperatively on axial magnetic resonance imaging (MRI).
There seems to be a controversy in literature regarding the address of the osteophytes on the distal clavicle (Fig. 14-4). Many reports advocate partial resection or coplaning of the AC joint if necessary to adequately decompress the subacromial space (25, 26, 27, 28, 29). On the other hand, Fischer et al. (30) reported on postoperative AC joint symptoms secondary to the violation of the AC joint during acromioplasty. The authors of this paper advocated an “all-or-none” approach to the AC joint and recommended distal clavicle resection any time the inferior capsule or the inferior osteophytes were removed. The senior author has addressed the inferior osteophytes of the distal clavicle impinging on the rotator cuff by using the coplaning technique. There has not been an increase in postoperative complications related to the AC joint when using this technique (Fig. 14-5). Kuster et al. (31) demonstrated that removal of inferior impinging osteophytes from the distal clavicle in asymptomatic AC joints exhibiting arthrosis did not result in any instability or pain postoperatively; however, routine violation of the inferior capsule of the AC joints with no arthrosis resulted in mild instability and tenderness in 9 out of 12 patients. We remove the impinging osteophytes and do not excise the entire distal clavicle in an otherwise asymptomatic AC joint; however, we try not to violate the AC joint if no impinging osteophytes are present. Percutaneous placement of a needle through the AC joint is an excellent guide during ASD for the location of the AC joint viewed from the subacromial space.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree