Abstract
Objective
The aim of this study was to assess the efficacy of gaseous cryotherapy following total knee arthroplasty (TKA) and to compare it to routinely used strategies for applying cold therapy.
Patients and methods
Sixty-six patients undergoing primary unilateral TKA were randomized into three groups and received “gaseous cryotherapy (GC)”, “cold pack” and “cryocuff” applications, respectively throughout the hospital stay. Primary outcomes (knee pain intensity, mobility and girth measurements) were recorded on preoperative day 1 as well as on postoperative day (POD) 7. Cutaneous temperature of the knee sides were also measured on POD7 just before and immediately after cold application.
Results
Although skin temperature dropped to 14 °C following GC versus 22 to 24 °C for the other two applications ( P < 0,05), the three groups did not differ at POD7 regarding the three primary outcomes. No adverse effects were observed with any of the ways of application.
Conclusions
Gaseous cryotherapy was not more beneficial than routinely used strategies for applying cold therapy. Further studies with larger sample size and with a more frequent and closer gaseous cryotherapy applications are needed to confirm our results.
Résumé
Objectif
Évaluer l’efficacité de la cryothérapie gazeuse après prothèse totale de genou (PTG) et la comparer à des modalités traditionnelles d’application thérapeutique du froid.
Patients et méthodes
Soixante-six patients programmés pour une PTG unilatérale primaire ont été randomisés en trois groupes qui ont bénéficié respectivement de « cryothérapie gazeuse » (CG), d’un « cold pack » et du « cryocuff » au cours de leur période d’hospitalisation. L’intensité de la douleur et les mesures périmétriques, et de mobilité du genou, qui constituaient les variables principales, ont été enregistrées la veille de l’intervention chirurgicale ainsi que sept jours après l’intervention (J + 7). La température cutanée du genou a également été mesurée dans les trois groupes à J + 7, juste avant et après l’application du froid.
Résultats
Bien que la température cutanée ait chuté jusqu’à 14 °C suite à la CG versus 22 à 24 °C pour les deux autres formes d’application ( p < 0,05), les trois groupes expérimentaux ne différaient pas significativement à J + 7 en termes d’intensité de la douleur, de mobilité et de mesures périmétriques. Aucun effet secondaire n’a été observé au sein des trois groupes expérimentaux.
Conclusions
La cryothérapie gazeuse ne s’est pas révélée plus efficace que des modalités traditionnelles d’application thérapeutique du froid. Des études complémentaires sur des échantillons plus larges, avec une application plus fréquente et une pulvérisation plus proche, sont nécessaires pour confirmer ces résultats.
1
English version
1.1
Introduction
Cold has been long known to have therapeutic effects: Hippocrates reported use of ice or snow to reduce edema formation and pain about 400 years before Christ . Nowadays, it is extensively used and is considered to be a key treatment for various acute injuries. Use of cold therapy (cryotherapy) has long been empirical. Although several studies have been conducted on the topic, numerous questions and controversies remain regarding its effects and the optimal ways to use it . Such discrepancies result from the significant heterogeneity between studies, which prevents comparative study, and from the low number of controlled and randomized studies .
Literature reports several physiologic effects of cryotherapy including reduction of skin , muscle and articular temperature, vasoconstriction of skin blood vessels leading to decrease in blood flow , and reduction of the inflammatory process resulting from decrease of tissue metabolism and from reduction in enzymatic activity . Application of cold also induces analgesia by means of an anti-nociceptive effect on the gate control system and the decrease of nerve conduction speed as well as prevention/reduction of post-traumatic edema and blood loss in post-surgical patients thanks to a decrease of vascular permeability and the vasoconstriction .
Various cooling mechanisms or devices used in clinics or on the sports field have been reported in the literature . Gaseous cryotherapy is one of them; this sophisticated cold application is based on the projection of CO 2 microcrystals under high pressure (CO 2 is now used instead of nitrogen-cold air ). This technique is supposed to decrease skin temperature to a greater extent than an ice bag and cause a more pronounced “thermal shock”; Mourot et al. also observed that gaseous cryotherapy triggered a systemic cutaneous vasoconstriction response . According to Chatap et al., hyperbaric CO 2 cryotherapy can also decrease pain scores in elderly inpatients with acute or chronic pain . However, no other studies have investigated the clinical benefits of hyperbaric gaseous cryotherapy. Thus, no published data are available regarding its benefits following total knee arthroplasty (TKA), which is a frequent surgical option to treat patients with end-stage knee osteoarthritis (OA) .
Although cryotherapy is used most of the time in post-surgical patients, there is no consensus regarding the optimal method of application i.e. forms of cryotherapy, temperature and frequency application, etc. and the specific management of cryotherapy after TKA . The need for further research stated in a survey on current practice of cryotherapy after TKA is confirmed by recent literature reviews on this topic .
Accordingly, the aim of the present work was to study whether gaseous cryotherapy is more effective in the postoperative care of people with TKA than routinely used cold application strategies i.e. cold gel packs or the Cryocuff ® .
1.2
Patients and methods
1.2.1
Participants
This prospective study concerned patients who were undergoing primary unilateral (TKA) in the Liège University Hospital. Patients were eligible for the study according to the following inclusion criteria: age between 40 and 85 years, severe osteoarthritis requiring a TKA. The exclusion criteria were: severe varus or valgus deformity, not proficient in French, rheumatoid arthritis, as well as major associated medical problems such as peripheral vascular disease, associated acute pathology, cold urticaria, and Raynaud’s phenomenon.
All patients received a low contact stress (LCS) prosthesis (De Puy, Johnson and Johnson) and were operated on by a senior orthopaedic surgeon with an anteromedial approach of the knee joint. A tourniquet was used in all patients and devascularisation of the leg lasted 45 to 55 minutes.
All patients gave written informed consent to participate. The medical ethics committee of the Liège University Hospital approved the study protocol.
1.2.2
Experimental design/procedure
On preoperative day 1 (PreOD1), patients were randomized into three groups using a computer generated table of random numbers; these groups differed by the main method that was going to be used to apply cold therapy throughout the hospital stay.
In the “gaseous cryotherapy” group (GC), a Cryotron™ device (Cryonic Médical, Salins-les-Bains, France) was used. This device consists of medical-grade liquid CO 2 in a cylinder equipped with an electrovalve and an immersed tube, a spray gun, and a nozzle. The CO 2 is sprayed on dry skin over the knee using a slow, regular, sweeping movement. A pistol fitted with a laser-guided infrared measurement system allows to control instantaneously the degree of skin cooling. A light switches on when the skin temperature drops to about 4 °C in order to avoid a risk of frostbite. As recommended by the manufacturer, the tip of the nozzle was kept 15 to 20 cm away from the skin. Gaseous cryotherapy provides painless (dry gas) air under high pressure (50 Bar) at a very low temperature (−78 °C) which causes the skin temperature to fall very quickly. Hyperbaric CO 2 cryotherapy was applied to patients for 90 seconds (30 seconds over the internal side of the knee, 30 seconds over the other side and 30 seconds over the popliteal fossa). The CO 2 was sprayed three times per day.
In the “cold pack” group (CP), a traditional “gel pack” (Physiopack ® ) (width 13 cm, length 30 cm, weight 400 g) was frozen for a minimum of 2 hours before application. The gel pack was placed transversally over the knee and secured with an elastic wrap. A towel was used as a barrier to prevent frostbite. The gel pack was applied to patients for 20 minutes, five times a day.
The “cryocuff” group (CC) was treated with a water-circulating device (Aircast ® Cryocuff ® , Inc., Summit, New Jersey) combined to the AutoChill ® System (Aircast ® , Inc., Summit, New Jersey) to provide cold and focal compression. A specific cuff surrounding the knee with pressurized ice water is linked by a tube to a cooler holding water and ice. It was applied to the knee for 20 minutes, five times a day.
All patients received cold therapy starting from postoperative day (POD) 2 (an earlier application was not possible because of the thickness of the dressings) and the therapy continued until the last hospitalization day. In all the groups, the applications were spaced by at least 1 hour: the first two cold applications were done in the morning (respectively before the physiotherapy session and before lunch) whereas the others took place in the afternoon. All patients were treated by the same physical therapist; they also received physiotherapy (30 min/day) which included traditional exercises including knee mobilization, muscle strengthening and gait training.
On Saturdays and Sundays, patients of the GC and CC groups were not treated with gaseous cryotherapy or with the Cryocuff ® : a gel pack identical to the CP group was applied to them.
1.2.3
Outcomes
Data were recorded on PreOD1 as well as on POD7 (corresponding to the minimal hospitalization length of stay); measurements took place in the morning, before cold application. The primary outcomes were the following:
- •
pain intensity. We used a visual analog scale (VAS) to measure knee pain intensity. The scale was a 10 cm line with no graduations that had the words “no pain” at one end and “worst pain imaginable” at the other end. The patient was asked to answer the following question: “How intense is your pain in the knee now?” by making a vertical mark on the line at the place that best reflected the intensity of the pain. The distance between the left end of the line (no pain) and the mark in millimeters was the VAS pain score (range 0–100);
- •
swelling of the phatologic knee and of the contralateral (“control”) knee was measured by bilateral girth measurements. They were taken with a meter tape at three levels i.e. at the joint line, 5 cm below it and 10 cm above it;
- •
passive and active knee flexion and extension range of motion were measured in a supine position using a goniometer. Its axis was placed over the lateral femoral epicondyle. The proximal end of the goniometer was aligned with the greater trochanter of the femur and the distal arm was aligned with the lateral malleolus. Measurements were recorded with respect to full extension being 0 degree with positive numbers indicating a more flexed position and negative numbers indicating hyperextension. During knee flexion, subjects were instructed to maximally flex the hip and knee and draw the heel toward the buttocks.
The cutaneous temperature of the internal and external sides of the knee was a secondary outcome; it was measured on POD7 just before and immediately after cold application as well as 30 minutes after application by using an infrared portable thermometer.
1.3
Statistics
Means and standard deviations were calculated by using basic statistical analysis. The between-group comparisons (at baseline and at POD7) were performed by means of an analysis of variance (Anova). Variables changes between PreOD1 and POD7 and the differences between the non-operated and the operated knee were analyzed by means of a paired t -test; analysis of variance with repeated measurements was used to examine changes in cutaneous temperature. A per-protocol analysis was used.
For all tests, a P -value ≤ 0.05 was considered statistically significant. All statistical analyses were performed with SPSS software, version 16.0.
1.4
Results
Forty female patients (mean ± standard deviation [SD]), 70.7 ± 8.6 y; height, 162.3 ± 7.8. cm; weight, 76.5 ± 14.9 kg) and 26 male patients (70.1 ± 8.5 y; height, 175.1 ± 5.3 cm; weight, 81.3 ± 10.1 kg) met the inclusion criteria and were selected for the current study. They all accepted to participate and were all submitted to the measurements during both evaluation sessions, i.e. PreOD1 and POD7.
In terms of age, bodyweight and height, there was no significant difference ( P > 0.05) between groups ( Table 1 ).
| GC ( n = 22) | CP ( n = 22) | CC ( n = 22) | ||||
|---|---|---|---|---|---|---|
| Males M ± SD | Females M ± SD | Males M ± SD | Females M ± SD | Males M ± SD | Females M ± SD | |
| n | 8 | 14 | 9 | 13 | 9 | 13 |
| Age (years) | 71.5 ± 6.5 | 72.3 ± 7.7 | 67.2 ± 11.9 | 68.8 ± 9.5 | 71.7 ± 5.6 | 70.9 ± 8.8 |
| Weight (kg) | 78.6 ± 5.4 | 79.2 ± 19.2 | 77.7 ± 11.2 | 75 ± 15.4 | 87.3 ± 10.3 | 75 ± 8.2 |
| Height (cm) | 173.1 ± 3.6 | 163.4 ± 6.4 | 175.2 ± 6.8 | 162.8 ± 10.2 | 176.8 ± 4.9 | 160.7 ± 6.5 |
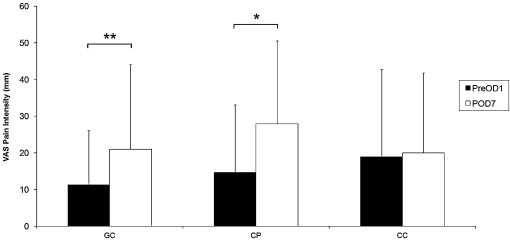
The between-group comparisons at baseline revealed no significant difference with regard to pain intensity. Following surgery, it increased significantly in the CP ( P < 0.05) and GC groups ( P < 0.01) whereas it remained stable in the CC group ( Fig. 1 ). At POD7, pain intensity was slightly higher in the CP group than in the other groups but the difference between groups remained non-significant ( P = 0.452).
At PreOD1 and when pooling all patients ( n = 66), the knee girth measurements were significantly lower in the “control” knee than in the pathological knee at the joint line ( P = 0.042) and 5 cm below it ( P = 0.029), but not 10 cm above it ( Table 2 ). Passive and active knee range of motion in flexion and extension were significantly reduced in the pathological knee ( Table 2 ).
| Patients ( n = 66) | |||
|---|---|---|---|
| Control knee M ± SD | Operative knee M ± SD | P -value | |
| Girth measurements | |||
| JL (cm) | 39.7 ± 4.8 | 40.5 ± 3.9 | 0.042 |
| JL − 5 (cm) | 35.8 ± 4.1 | 36.2 ± 3.9 | 0.029 |
| JL + 10 (cm) | 43.9 ± 6.4 | 44.3 ± 6 | 0.6 |
| Mobility | |||
| Active flexion (°) | 121.5 ± 11.4 | 116.6 ± 12.3 | < 0.001 |
| Passive flexion (°) | 126.1 ± 11.7 | 120.6 ± 12.5 | < 0.001 |
| Active extension (°) | 0.9 ± 3.6 | 3.6 ± 5.5 | < 0.001 |
| Passive extension (°) | −1.5 ± 4.4 | 1.3 ± 5.8 | < 0.001 |
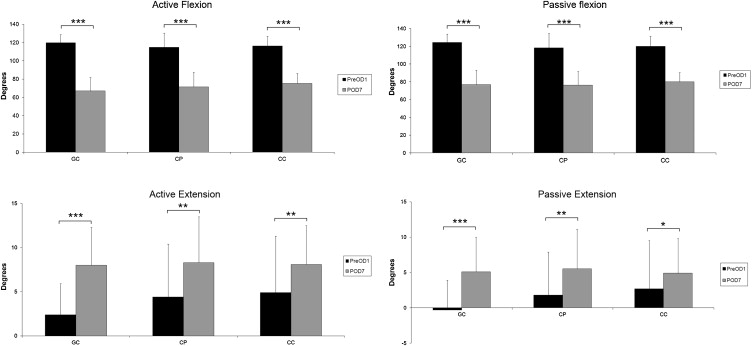
Following surgery, range of motion of the operated knee further decreased ( P < 0.05) in all groups ( Fig. 2 ). There was no significant difference between groups.
Girth measurements of the operated knee increased following surgery; at POD7, they remained significantly higher than baseline values ( P < 0.001) for all measurement sites ( Table 3 ). Statistical analysis revealed no significant difference between groups.
| GC | CP | CC | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PreOD1 M ± SD | POD7 M ± SD | P -value | PreOD1 M ± SD | POD7 M ± SD | P -value | PreOD1 M ± SD | POD7 M ± SD | P -value | |
| JL (cm) | 40.2 ± 4 | 43 ± 4.5 | < 0.001 | 41 ± 4.7 | 43.5 ± 4.5 | < 0.001 | 40.3 ± 3.1 | 42.9 ± 3.4 | < 0.001 |
| JL − 5 (cm) | 35.2 ± 3.3 | 37.6 ± 3.3 | < 0.001 | 36.8 ± 5 | 38.8 ± 4.5 | < 0.001 | 36.2 ± 3.1 | 38.9 ± 3.6 | < 0.001 |
| JL − 10 (cm) | 43.1 ± 6.2 | 46.8 ± 5.7 | < 0.001 | 44.6 ± 6.6 | 47.9 ± 5.9 | < 0.001 | 44.5 ± 4.7 | 47.4 ± 4.8 | < 0.001 |
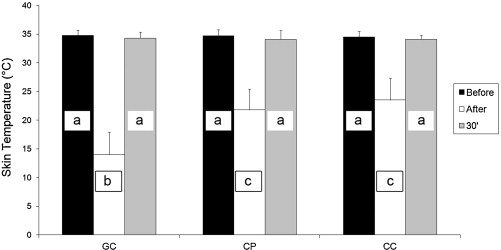
No significant differences were observed between internal and external sides regarding skin temperature; accordingly, results of both sides were merged. Fig. 3 presents skin temperature at the knee side before and immediately after the application, as well as 30 minutes later for the three experimental groups. In each experimental group, temperature significantly decreased following the application ( P < 0.001) and returned to baseline values within 30 minutes post-application. No between-group difference regarding skin temperature was observed except following the application, when skin temperature was decreased in a greater extent when using gaseous cryotherapy than when using the other forms of cryotherapy ( P < 0.05).
We did not observe any adverse effects with any of the ways of application.
1.5
Discussion
The aim of this study was to assess the efficacy of gaseous cryotherapy in the postoperative care of people with TKA; therefore, we compared it to the easiest and most traditional way to apply cold (gel pack) as well as to the Cryocuff ® which has been used in several previous studies involving patients following TKA . Selecting patients after TKA to study cryotherapy benefits appears to be relevant because it is a well circumscribed intervention, which causes extensive tissue damage as well as severe postoperative pain and edema . The absence of a control/placebo group can be explained by the fact that cryotherapy is well accepted in the postoperative management of knee surgery , considering the severe postoperative pain and the significant benefit of cryotherapy in pain control observed in several studies . Benefits of cryotherapy following TKA was confirmed by Morsi who studied 30 patients undergoing staged bilateral TKA . In every patient, one TKA had a continuous-flow cooling device for 6 days postoperatively (skin temperature kept at a mean of 7°C for the first 2 hours and at 12°C after that) whereas the other TKA in the same patient was done 6 weeks later and had no cooling device. Morsi reported that pain intensity score as well as analgesic consumption were always greater in the control group . In addition to the effect on nerve conduction speed , cold is supposed to inhibit swelling by reducing edema .
As far as we know, the present study is the first one that assesses the efficacy of hyperbaric gaseous cryotherapy in the postoperative care of people with TKA. The literature includes only a few studies of its physiological and clinical effects . The three experimental groups did not differ significantly at POD7 regarding pain intensity, mobility and girth measurements. Changes from PreOD1 to POD7 were also identical between groups except for pain intensity, which remained stable only in the CC group; the latter observation might result partly from slightly higher baseline pain values in this group compared to the others. Consistent with the literature mobility, which usually decreases drastically 1 day after surgery , was still reduced at POD7 as a result of swelling, pain and muscle spasm . At POD7, girth measurements (reflecting swelling resulting from haemorrhage and edema ) remained also significantly higher than baseline values in all the groups.
Thus, clinical results were similar between groups although gaseous cryotherapy was applied only three times for 90 seconds whereas the cold pack and Cryocuff ® were used five times a day for 20 minutes. Skin temperature resulting from such cold applications also differed considerably: baseline skin temperature was similar in the three groups (averaging 34–35°C) and decreased significantly in all groups when cold was applied; however, it reached 22 to 24°C at the end of the cold pack or cryocuff applications and dropped to a mean of 14°C following the gaseous cryotherapy. This more important thermal shock (fast decline in temperature), also reported by Mourot et al., results from the sublimation of dry ice to carbon dioxide gas which is a very endothermic reaction . Mourot et al. reported a skin temperature reaching 7.3°C at the end of a 2-minute gaseous cryotherapy application when maintaining the pipe at a distance of 7 to 10 cm of the skin surface of the dorsal aspect of one hand . Therefore, a greater thermal shock might have occurred in our study if a longer application time and/or a closer application of gaseous cryotherapy had been applied. In this context, better clinical effects might also have occurred because decreased pain perception, reduction of edema, diminished metabolic enzyme activity, vasoconstriction are supposed to occur when skin temperature is reduced to about 10°C to 15°C .
As previously stated, the current study does not suggest difference between techniques regarding the clinical efficiency; therefore the specific advantages and drawbacks of each modality should be taken into account when a choice between techniques has to be made. Gaseous cryotherapy provides similar benefits to the more traditional cooling methods with lesser and shorter sessions; however a specific training for application is needed and the device (as well as the cylinders of gas) is costly. The traditional cold pack is very easy to use, even for patients, and is not expensive; however, the often-limited flexibility of the frozen cold pack decreased the size of the contact area. The Cryocuff ® is easy to use, combines cryotherapy and compression , has been especially developed to conform well to the tissue and allows to keep a stable temperature for a longer time than with a cold pack; however it is more expensive than a cold pack and its combination to the AutoChill ® System (to provide continuous cold and pulsating pressure) requires electrical power.
This present study suffers a few limitations. Our data were analyzed only on a per-protocol basis and the randomisation of our sample into three experimental groups decreases the statistical power of the present work. The hyperbaric gaseous cryotherapy, the Cryocuff ® , as well as the cold pack secured with a wrap provided some compression, which might influence positively the outcomes; results of studies comparing cold compression therapy with either modality alone remain controversial . Furthermore, in the CC and GC groups, the Cryocuff ® and the Cryotron™ were not used during the weekend (patients had a similar treatment as the CP group); although the methodology used in the current study best reflects the clinical practice of our hospital (during the weekend, only the nurses are treating the patients), it might underestimate the benefits of gaseous cryotherapy over the cold pack application. Considering our experimental design, we did not report the outcomes time course and based our results only on the POD7. Yet, measurements of pain intensity one day following the surgery would have been useful in better interpreting the changes of this outcome. Although benefits of cryotherapy on length of stay have been reported in previous studies , we did not consider this outcome. Indeed the discharge decision is influenced by several factors, i.e. the future (hospitalisation in an inpatient rehabilitation service, in a day hospital or at the patient’s home), the achievement of functional independence (transfers, ambulation) and the living situation (alone or not, presence of a home help) of the patient .
1.6
Conclusion
No difference between groups was observed regarding the clinical outcomes. Further studies with larger sample size and with a more frequent and closer gaseous cryotherapy applications are needed to confirm that gaseous cryotherapy is not more beneficial than more traditional cold applications following TKA.
Disclosure of interest
The authors declare having no private or personal interest to influence the results of the present study. A commercial society lent the Cryotron™ device for a definite period of time and gave several cylinders of compressed medical-grade carbon dioxide gas to conduct the study.
Acknowledgments
The authors acknowledge the valuable help and assistance of Ms Annie Depaifve, Mr Paul Remont, Mr Richard Frères, Mr Sébastien Wolfs as well as Mr André Tits.
2
Version française
2.1
Introduction
Les effets thérapeutiques du froid sont connus depuis longtemps : 400 ans avant JC, Hippocrate parlait déjà de l’utilisation de la glace ou de la neige pour réduire la formation des œdèmes et soulager la douleur .
De nos jours, le froid est couramment utilisé et considéré comme un traitement clé dans de nombreuses blessures et pathologies. L’utilisation de la thérapie par le froid (cryothérapie) a longtemps été empirique. Bien que de nombreuses études se soient intéressées au sujet, plusieurs questions et controverses restent en suspens au sujet de ses effets et concernant la meilleure modalité d’application . Cela résulte de l’hétérogénéité des travaux, empêchant toute étude comparative ainsi que du faible nombre d’études contrôlées et randomisées .
La littérature rapporte plusieurs effets physiologiques de la cryothérapie telles qu’une baisse de la température cutanée , musculaire et articulaire , une vasoconstriction des vaisseaux cutanés débouchant sur une baisse du débit sanguin et une réduction du processus inflammatoire grâce à une diminution du métabolisme tissulaire et de l’activité enzymatique . L’application de froid entraîne également une analgésie par l’élévation du seuil de la douleur et le ralentissement de la conduction nerveuse ainsi que la prévention/réduction des œdèmes post-traumatiques et de la perte sanguine chez le patient opéré en raison de la diminution de la perméabilité vasculaire et de la vasoconstriction . La littérature rapporte divers systèmes ou appareils de refroidissement utilisés dans les cliniques ou sur les terrains de sport . La cryothérapie gazeuse est une de ces techniques ; cette application de froid sophistiquée est basée sur la sublimation de CO 2 liquide qui, à l’aide d’un pistolet, permet la projection de microcristaux de carboglace associés à une pression hyperbare (le CO 2 a remplacé l’azote liquide qui était utilisé initialement ). Cette technique est destinée à réduire brutalement la température cutanée créant ainsi un « choc thermique » bien plus prononcé qu’avec une poche de glace ; Mourot et al. ont noté que la cryothérapie gazeuse déclenchait une réaction systémique de vasoconstriction cutanée . Selon Chatap et al., la cryothérapie hyperbare au CO 2 permet également de réduire les scores de la douleur chez les patients âgés hospitalisés souffrant de douleurs aiguës ou chroniques . Cependant, aucune autre étude ne s’est intéressée aux bénéfices cliniques de cette cryothérapie gazeuse hyperbare. Ainsi, aucune donnée n’est disponible sur les bénéfices de cette technique après arthroplastie totale du genou, intervention chirurgicale pourtant fréquente en cas de gonarthrose avancée . Bien que la cryothérapie soit utilisée le plus souvent en postopératoire, il n’existe aucun consensus concernant la méthode optimale d’application (choix de la technique, température cutanée à atteindre, fréquence d’application ) ainsi que sur les modalités d’application spécifiques de la cryothérapie après arthroplastie totale du genou . Un sondage concernant les pratiques cliniques usuelles de la cryothérapie après prothèse totale du genou (PTG) a souligné la nécessité de mener des études complémentaire sur le sujet ; cette nécessité a été confirmée par de récentes revues de littérature sur ce sujet . Pour ces raisons, l’objectif de cette étude était d’examiner si la cryothérapie gazeuse est plus efficace dans la prise en charge postopératoire des patients opérés d’une PTG que les techniques de cryothérapie plus couramment utilisées comme les poches de gel congelé « cold pack » ou le « Cryocuff ® ».
2.2
Patients et méthodes
2.2.1
Participants
Cette étude prospective concernait des patients de l’hôpital universitaire de Liège programmés pour une PTG. Les critères d’inclusion étaient : âge entre 40 et 85 ans, gonarthrose sévère nécessitant une PTG. Les critères d’exclusion étaient les suivants : déformation importante en varus ou valgus, compréhension limitée du français, polyarthrite rhumatoïde ainsi que certaines conditions associées, comme une maladie vasculaire périphérique (MVP) ou des pathologies sérieuses, l’urticaire au froid et la maladie de Raynaud. Tous les patients ont été opérés par un chirurgien orthopédique sénior. La voie d’abord a toujours été antéro-médiane et une prothèse LCS (De Puy, Johnson and Johnson) a systématiquement été utilisée. L’intervention s’est déroulée sous garrot pneumatique avec un temps de dévascularisation de 45 à 55 minutes. Tous les sujets ont signé un formulaire de consentement éclairé. Le comité d’éthique de l’hôpital universitaire de Liège a approuvé le protocole d’étude.
2.2.2
Protocole et procédure
La veille de la chirurgie (J − 1), les patients ont été randomisés en trois groupes selon une liste informatisée de nombre pris au hasard ; la seule différence entre les groupes étant la méthode de cryothérapie à utiliser au cours de l’hospitalisation.
Dans le groupe « cryothérapie gazeuse » (CG), un Cryotron™ (Cryonic Médical, Salins-les-Bains, France) a été utilisé. Cet appareil contient du CO 2 médical liquide dans un cylindre équipé d’une électrovalve et d’un tube immergé, d’un pistolet et d’un embout. Le CO 2 est projeté sur la peau sèche au niveau du genou avec un mouvement de balayage lent et régulier. Le pistolet équipé avec un système de capteur de mesure à infrarouge, guidé par laser, permet de contrôler instantanément le degré de refroidissement de la peau. Une lumière s’allume quand la température de la peau atteint 4 °C afin d’éviter le risque d’engelures. Suivant les recommandations du fabricant, l’embout était tenu à distance de 15 à 20 cm de la peau. La cryothérapie gazeuse permet de pulvériser de l’air à haute pression (50 Bar) et à température très basse (−78 °C) ce qui cause une chute très rapide de la température de la peau. La cryothérapie gazeuse hyperbare était appliquée aux patients pendant 90 secondes (30 secondes sur la face interne du genou, 30 secondes de l’autre côté et 30 secondes sur le creux poplité) à raison de trois fois par jour.
Dans le groupe « cold pack » (CP), une poche de gel traditionnelle (Physiopack ® ) (largeur 13 cm, longueur 30 cm, poids 400 g) était mise au congélateur au minimum 2 heures avant l’application. La poche de gel recouvrait le genou et était fixée avec une bande élastique. Une serviette servait de barrière afin d’éviter les engelures. Cette poche de froid était utilisée sur les patients 20 minutes, cinq fois par jour.
Le groupe « cryocuff » (CC) était traité avec un système de cryothérapie basé sur la circulation d’eau froide (Aircast ® Cryocuff ® , Inc., Summit, New Jersey) associé à l’AutoChill ® System (Aircast ® 4, Inc, Summit, New Jersey) afin d’assurer une compression froide et localisée. Un manchon spécifique entourant le genou est alimenté en eau glacée par une glacière contenant de l’eau et de la glace. Ce manchon était appliqué pendant 20 minutes, à raison de cinq fois par jour.
Pour tous les patients, la cryothérapie commençait le deuxième jour postopératoire (J + 2) (une application plus tôt était difficile en raison de l’épaisseur du pansement) et la thérapie continuait jusqu’au dernier jour d’hospitalisation. Dans tous les groupes, les applications étaient espacées d’au moins une heure : les deux premières avaient lieu le matin (respectivement avant la séance de kinésithérapie et avant le déjeuner) alors que les autres avaient lieu l’après-midi. Tous les patients étaient traités par le même kinésithérapeute ; ils bénéficiaient également de séances de kinésithérapie (30 minutes par jour) comprenant des exercices traditionnels (mobilisation du genou, renforcement musculaire et entraînement à la marche).
Le samedi et le dimanche, les patients des groupes CG et CC ne bénéficiaient pas de cryothérapie gazeuse ou du Cryocuff ® : une poche de gel identique à celle du groupe CP était utilisée.
2.2.3
Variables
Les mesures ont été effectuées à J − 1 et J + 7 (correspondant à la durée d’hospitalisation minimale) ; les mesures se faisaient le matin, avant l’application du froid. Les variables principales étaient :
- •
l’intensité de la douleur, évaluée au moyen d’une échelle visuelle analogique (EVA). L’échelle se présente comme une ligne sans graduation de 10 cm avec les mots « aucune douleur » à l’extrémité gauche et « pire douleur imaginable » à l’extrémité droite. Le patient devait répondre à la question suivante : « quelle est l’intensité de votre douleur au genou en ce moment ? » et il devait indiquer un trait sur l’échelle afin de refléter le plus précisément l’intensité de sa douleur. La distance entre le côté gauche (aucune douleur) et la marque faite par le patient (en millimètres) était définie comme le score EVA (de 0 à 100) ;
- •
le gonflement du genou pathologique et celui du genou controlatéral (« contrôle ») était évalué à l’aide de mesures périmétriques bilatérales. Ces mesures étaient effectuées à l’aide d’un mètre ruban en trois endroits : l’interligne articulaire, 5 cm en dessous et 10 cm au-dessus ;
- •
l’amplitude articulaire passive et active en flexion et extension du genou ; ces mesures étaient prises à l’aide d’un goniomètre avec le patient en position allongée. L’axe du goniomètre était placé au niveau du condyle fémoral latéral. L’extrémité proximale du goniomètre était alignée le long du grand trochanter et le bras distal positionné le long de la malléole externe. Zéro degré correspondait à une extension complète ; les nombres positifs indiquaient un flexum de genou et les nombres négatifs soulignaient une hyperextension. Durant la flexion du genou, les sujets avaient pour instruction de fléchir au maximum la hanche et le genou et d’amener le talon vers les fesses.
La température cutanée de la peau mesurée à la face interne et externe du genou constituait une variable secondaire ; cette mesure était enregistrée à J + 7 juste avant et immédiatement après l’application de froid, mais également 30 minutes après l’application en utilisant un thermomètre portable à infrarouge.
2.3
Statistiques
Les moyennes et écarts-types (ET) ont été calculés à l’aide de méthodes d’analyse statistique communément utilisées. Les comparaisons intergroupes (à l’inclusion et à J + 7) ont été réalisées avec une analyse de variance (Anova). L’évolution des variables entre J − 1 et J + 7 et la comparaison des mesures du genou opéré et du genou contrôle ont été étudiées au moyen d’un test- t apparié ; une analyse de variance avec des mesures répétées a servi à comparer la température cutanée mesurées à trois moments différents. Une analyse per-protocole a été conduite.
Pour tous les tests, la valeur p ≤ 0,05 était considérée comme statistiquement significative. Toutes les analyses ont été réalisées avec le logiciel SPSS, version 16.0.
2.4
Résultats
Au total, 66 patients ont été inclus. Quarante femmes (moyenne ± écart-type, âge 70,7 ± 8,6 ans ; taille 162,3 ± 7,8.cm ; poids 76,5 ± 14,9 kg) et 26 hommes (âge 70,1 ± 8,5 ans ; taille, 175,1 ± 5,3 cm ; poids 81,3 ± 10,1 kg). Ils ont tous accepté de participer et ont été évalués à deux reprises, c’est-à-dire J − 1 et J + 7. En termes d’âge, de poids et de taille, il n’y avait aucune différence significative ( p > 0,05) entre les groupes ( Tableau 1 ).







