Abstract
Objective
If the pathophysiology of bladder cooling reflex (BCR) elicited during an ice water test (IWT) is well-known (triggered by activation of cold receptors within the bladder wall supplied by unmyelinated C fiber afferents) and is widely used for the diagnosis of upper motor neurological lesions, the significance of having a perception of cold in the bladder (PCB) during IWT has not been properly defined yet.
Patient and methods
Hundred and twenty patients undergoing IWT were analyzed and separated into four groups: group 1 (G1): patients with idiopathic overactive bladder syndrome (OAB); group 2 (G2): patients with functional dysuria (difficult urination due to bladder-neck obstruction, or congenital large bladder); group 3 (G3): patients with multiple sclerosis (MS) and group 4 (G4): patients with cauda equina syndrome (CES). All patients had a cystometry and IWT. After performing IWT, the patients were asked specific questions regarding the various sensations experienced during the cystometry and IWT, especially for detecting the presence or not of a cold sensation when their bladder was filling up.
Results
Patients with idiopathic OAB had more frequently a PCB than patients with MS ( P < 0.02). Patients with bladder-neck obstruction were more likely to retain a PCB than patients with CES ( P < 0.01). Lack of PCB is more frequent in patients with neurological diseases ( P < 0.001), with a sensitivity of 66% and specificity of 65%.
Conclusion
Patients without neurological disease have a heightened PCB during the IWT than patients with neurological diseases. The lack of PCB may reflect an alteration of the afferent pathways or spinal reflex pathways or central neural pathways.
Résumé
Objectifs
Si la signification du réflexe au froid obtenu au cours d’un test à l’eau glacée (TEG) est bien connue (positivité si lésions neurologiques supraspinales ou syndrome obstructif), l’altération de la perception du froid vésical (PFV) lors du TEG a été peu étudiée.
Patient et méthodes
Cent vingt TEG ont été analysés. Quatre sous-groupes de 30 patients ont été individualisés en fonction de la pathologie causale : groupe 1 : hyperactivité vésicale idiopathique ; groupe 2 : dysurie fonctionnelle ; groupe 3 : sclérose en plaques (SEP) ; groupe 4 : syndrome de la queue de cheval. À la fin du TEG, il était demandé quelle sensation avait été perçue, permettant d’apprécier la PFV.
Résultats
Les patients souffrant d’hyperactivité vésicale idiopathique ont plus souvent une PFV conservée que les patients atteints de SEP ( p < 0,02). Les patients atteints de dysurie fonctionnelle perçoivent plus fréquemment le froid que ceux atteints de syndrome de la queue de cheval ( p < 0,01). L’absence de PFV est plus fréquente chez les patients atteints de pathologie neurologique ( p < 0,001). La sensibilité de ce signe en faveur d’une atteinte neurologique centrale ou périphérique est de 66 %, et sa spécificité est de 65 %.
Conclusion
Les patients indemnes de pathologies neurologiques perçoivent plus souvent le froid intravésical que les patients souffrant de pathologies neurologiques centrales ou périphériques. Cette altération de la PFV pourrait être le témoin d’une lésion des voies afférentes ou des centres intégrateurs spinaux ou encéphaliques.
1
English version
1.1
Introduction
A normal bladder mictional reflex is usually triggered by the stimulation of mechanoreceptors activating type A fibres afferent pathways. The information regarding bladder filling is being transmitted via these myelinated fibres allowing an individual to know when he or she needs to urinate . Normal bladder sensitivity is thus necessary for proper bladder functions . Cold sensitivity is implied in a mictional reflex, called bladder cooling reflex (BCR). This reflex triggers an involuntary detrusor contraction when the bladder is being filled with cold saline solution. BCR seems to be mediated by the type C afferent fibres and integrated at the level of the sacral spinal cord . This spinal cord reflex exists at a physiological level in the child until the age of 4 then it disappears as it becomes inhibited by the supraspinal centres. When this reflex reappears in children over the age of 6 or in adults it is considered as an indicator of potential spinal cord lesions or lesions of the central motor neuron . This reflex is similar to the Babinski’s reflex, a physiological plantar reflex in newborns that can reappear in case of lesions of the central nervous system (CNS) .
Interpreting the results of the ice water test (IWT) in terms of detrusor motricity is a well-known process. IWT has a sensitivity of 65% and a specificity of 85% for the diagnosis of detrusor hyperactivity and points out to a neurological pathology at the origin of the bladder/bowel symptoms . IWT sensitivity increases with its repetition . In patients with spinal cord injury (SCI), the IWT is positive in 95% of the patients with complete SCI and 86% of patients with incomplete SCI . However a certain proportion of patients that seem apparently free from neurological pathologies do have a positive IWT, this represents around 15% of patients . The IWT can also be positive in case of bladder outlet obstruction (BOO) .
The presence or lack of PCB has rarely been studied. The aim of this work is to analyze PCB in different populations of patients affected or not by central or peripheral neurological pathologies and to look for a correlation between PCB alteration and the pathology.
1.2
Patient and methods
Hundred and twenty patients were included in the study. These 120 patients were separated into four groups according to their original pathology. Each group included 30 patients:
- •
group 1: patients suffering from idiopathic overactive bladder syndrome (OAB), without any identified neurological cause or BOO;
- •
group 2: patients suffering from functional dysuria (difficult urination) due to functional bladder dysfunctions, congenital large bladders, or bladder-neck disease;
- •
group 3: patients with multiple sclerosis (MS):
- ∘
16 patients complained about a clinical bladder overactivity syndrome and associated pain,
- ∘
10 patients had an isolated clinical bladder overactivity syndrome (urge to urinate with or without incontinence),
- ∘
four patients had dysuria and a sensation of improper bladder emptying;
- ∘
- •
group 4: patients with cauda equina syndrome (CES).
1.2.1
Technique
Each patient benefited from urodynamic exploration following the recommendations for good urodynamic practices from International Continence Society (ICS) , followed by an IWT according to the following methodology:
- •
before filling the bladder with ice water the patient had a cystometry where the bladder was filled with water at room temperature and at the same speed than the IWT (100 ml/min). This precaution allows for differentiating a detrusor contraction really triggered by a cold stimulus from a detrusor contraction triggered by filling up the bladder, with the same given speed and volume ;
- •
IWT itself is a cystometry examination with a filling speed of 100 ml/min and ice water (<4 °C) . IWT is considered positive in several situations determining three types of positive IWT . The IWT can unveil a detrusor hyperactivity that was not previously observed on cystometry examinations at room temperature. This type of results can classify the IWT as class A positive (if the uninhibited detrusor contraction happens before 200 ml of fluid in the bladder) or class B positive (if the uninhibited detrusor contraction happens between 200 and 400 ml of fluid in the bladder). Sometimes there is detrusor overactivity on a regular cystometry examination. In that case the IWT is considered positive (class C) if the uninhibited detrusor contraction occurred when the bladder was filled with half the volume used during regular cystometry examination .
1.2.2
Study of the perception of cold in the bladder (PCB)
Questioning patients at the end of urodynamic examination have evaluated PCB. The following question was asked to each patient: “Did you feel a difference during the last test?”. If the patients reported a sensation of cold, they were asked to specify if the cold was felt at bladder level or urethral level in order to take only PCB into consideration. In fact, differentiating the perception of cold sensation in the urethra (not considered for the study) and a real PCB is essential since the perception of cold at urethral level is more commonly seen and does not seem to have the same pathophysiological significance .
1.2.3
Statistics
We used the Student’s t -test to compare the means of independent data, after checking for Gaussian distribution of the data studied and variances. The Pearson’s Chi 2 test was used to look for differences between two distributions. The significance was set at P < 0.05.
1.3
Results
1.3.1
Demographics analysis
The patient’s demographics (age and sex) from the different groups are summed up in Table 1 . The mean age for patients affected with neurological disease is 51.26 years (standard deviation [S.D.]: 12.4). The mean age for patients not affected by neurological disease is 49.28 years (S.D.: 14.19). There is no significant difference between the mean age of patients with neurological disease and the patients without any neurological disease, P = 0.42. There are more women in group 1 than in group 2 ( P = 0.03), group 3 ( P = 0.007) and group 4 ( P = 0.0003). Among patients affected by neurological diseases there are 24 men and 36 women. Among patients free from neurological pathologies there are nine men and 51 women. There are more women in the group of patients with a functional pathology (OAB or dysuria) than in the group of patients with neurological pathologies (MS or CES), P = 0.004.
| Group 1 | Group 2 | Group 3 | Group 4 | |
|---|---|---|---|---|
| Idiopathic bladder overactivity (BOA) | Functional dysuria | Multiple sclerosis | Cauda equina syndrome (CES) | |
| Mean age (standard deviation) | 52.77 years (14.45) | 45.8 years (13.27) | 49.23 years (8.7) | 53,3 years (15.18) |
| Repartition (men/women) | 1 M/29 W | 8 M/22 W | 10 M/20 W | 14 M/16 W |
Patients in group 3 with MS have a mean Expanded Disability Status Scale (EDSS) score of 5 (ranges: 2–8, S.D.: 1).
1.3.2
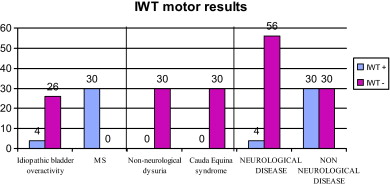
Results of the ice water test
Twelve patients out of 30 in group 1 (idiopathic OAB) are affected by detrusor overactivity, including eight patients with a negative IWT, two with type B positive IWT and two with type C positive IWT.
In group 2, among patients affected by functional dysuria 22 of them had a normally active detrusor and eight had an underactive detrusor. None of the IWT came back positive.
All patients in group 3 (MS) had an overactive detrusor: 10 of them had type A positive IWT, nine had type B positive IWT and 11 had type C positive IWT.
Patients with CES all had an underactive detrusor and negative IWT ( Fig. 1 ).
1.3.3
Perception of cold in the bladder
The proportion of patients not reporting a cold sensation during the IWT is described below ( Fig. 2 ):
- •
group 1 (idiopathic OAB): 43.3% (e.g., 13 patients out of 30);
- •
group 2 (non-neurological dysuria): 26.6% (e.g., eight patients out of 30);
- •
group 3 (MS): 73.3% (e.g., 22 patients out of 30);
- •
group 4 (CES): 60% (18 patients out of 23).
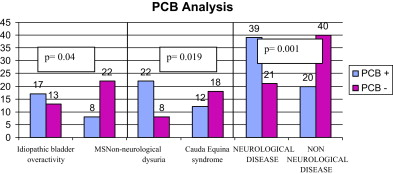
Not feeling the cold sensation during the IWT is significantly more common in patients with neurological pathologies ( P = 0.001), than in patients with bladder disorders in a non-neurological context. Out of the 120 individuals in this study, 34 had a positive IWT on a motor level, meaning an overactive detrusor unveiled or aggravated by filling the bladder with ice water. This positive IWT brings up a neurological etiology and is correlated to the lack of PCB ( P = 0.03).
In spite of patients describing similar clinical symptoms, patients suffering from idiopathic bladder overactivity report more PCB than patients with MS, the difference is significant ( P = 0.04).
In the same manner, there is a significant difference in PCB if we compare patients with CES and patients suffering from non-neurological dysuria ( P = 0.019) ( Fig. 2 ).
Globally, the lack of PCB is correlated to a central or peripheral neurological affection with 66% sensitivity and 65% specificity.
1.4
Discussion
In mammals the perception of cold can be felt in the bladder. PCB is transmitted by unmyelinated type C afferent sensitive fibres. Recently in humans, some specific thermoreceptors have been implicated in the proper functioning of the nervous pathways in the bladder. These receptors involved in the PCB in human beings are transient receptor potential channel of melastatin type 8 (TRPM8) that play a role in the thermal sensitivity in mammals . In rats, these receptors are quite similar to cutaneous thermoreceptors compared with other types of sensitive receptors like mechanoreceptors or receptors to nociceptive stimuli .
If the existence of PCB is clearly admitted, its pathophysiological action is still being debated. One of the physiological hypotheses for the existence of this thermal sensitivity in the bladder would be its participation in the regulation and maintenance of a stable central core body temperature. In bladder pathologies some changes in TRPM8 expression in cell bodies appear. In fact authors reported an increased TRPM8 expression in patients suffering for OAB compared to healthy patients (control group) . Changes in bladder wall thickness would be responsible for an increase in type C fibres due to the sprouting phenomenon (anarchical new growths of nerve fibres). However the significance of this histological change on PCB has not been demonstrated yet .
In our study, it appears that patients free for neurological pathologies report more significantly a PCB than patients suffering from central (MS) or peripheral (CES) neurological affections. The lack of PCB would be a sign that neurological pathways are interrupted in an abnormal way. If PBC seems to be a clinical symptom for a central or peripheral neurological affection, its sensitivity and specificity remain quite modest.
Some patients with neurological affections, especially in the CES subgroup perceive this sensation of cold (false negative). This could be explained by the incomplete nature of the peripheral injuries in these patients.
In patients free from neurological pathologies some patients do not report any PCB (false negative). Several hypotheses can be brought up to explain why some patients from the control group do not report the PCB:
- •
first, one of the limit of the study is the constitution of the control groups. These patients are affected by bladder pathologies with an unclear mechanism that we considered as non-neurological. However, we cannot totally exclude the hypothesis that some patients might be affected by a neurological pathology that could be asymptomatic or just beginning. This could be the case of patients with bladder-neck disease, congenital large bladder or idiopathic detrusor hyperactivity, who might suffer from a beginning dysautonomic disorder;
- •
second, it might be possible that the activation of bladder thermoreceptors in some healthy patients do not trigger a cold sensation, either because these patients are unable to describe their perception, or because the activation of visceral thermoreceptors does not necessarily trigger a conscious sensation. The sensation induced by the activation could also be quite difficult to locate ;
- •
third, it is possible that a bladder filling threshold needs to be reached in order for some patients to perceive the cold. Asking the subjects to indicate the precise moment when they perceived the sensation of cold in the bladder during the cystometry could validate this hypothesis.
Very few studies focused on PCB in neurological pathologies. Regarding peripheral neurological pathologies, two studies were found. Guntenberg et al. reported in 1975 a study on the bladder and urethral sensitivity in patients affected by unilateral or bilateral sacral nerve roots injuries. For patients with a unilateral injury of the sacral nerve, the thermal sensitivity of the bladder was evaluated during a cystoscopy by projecting jet streams of cold and hot saline solution against the bladder wall both on the normal side and the denervated side. On the side of the lesion, the difference in temperature was not perceived by the patient neither was touch (pin prick test) . The study of Ishigooka et al. consisted in the evaluation of PCB in 32 patients with diabetes mellitus, well-known for causing sensitive disorders usually regarding the bladder sensations. In this study 16 patients had a validated diabetic cystopathy and 16 patients had a normal urodynamic checkup. None of the IWT were positive in this population. PCB was more often altered in patients with diabetic cystopathy . The results are in accordance with the thermal sensitivity disorders of the bladder observed in our group of patients affected by a peripheral neurological pathology.
Regarding central neurological pathologies, in 2000 Ismael et al. in their study reported an evaluation of PCB in response to the IWT in a population of 39 patients with MS. The cold was felt in a higher proportion of patients than in our study since 71% of patients reported a sensation of cold versus 26.7% of patients with MS in our study. The difference in results can be explained by the fact that patients in this study were asked on all cold sensations: bladder, urethral and lower abdomen .
Hellström’s et al. study on patients with various pathologies (central and peripheral neurological affections, BOO, effort urinary incontinence, idiopathic OAB) and on normal subjects, showed that PCB was most often missing for patients with central or peripheral neurological lesions or in patients with BOO. This result in patients with BOO could be explained by some degree of bladder denervation secondary to the obstruction . Tammela et al. have confirmed this same notion; they studied PCB in 73 patients with BOO (prostate hypertrophy). In these patients, detrusor overactivity was more common in patients without PCB probably reflecting a denervation caused by BOO .
In 2006, Mukerji et al. studied PCB and the onset of pain during the IWT in 64 patients, separated into four groups: painful bladder syndrome (17 patients), idiopathic detrusor overactivity (22 patients), neurological detrusor overactivity (four patients) and stress urinary incontinence (control group, 21 patients). The IWT was negative for all subjects in the control group and the group of patients presenting a painful bladder syndrome. IWT was positive for the four patients with a neurological disease and positive in 27.3% of the cases in patients with idiopathic detrusor overactivity where primary obstructive cause was not precisely defined. PCB was reported in 9.3% of patients from all groups, but without any significant difference highlighted between these groups with a small number of patients. In patients with painful bladder syndrome, pain during IWT was reported in 94.1% of cases and was significantly stronger than during the other bladder filling tests .
1.5
Conclusion
IWT is usually done as a motor test to unveil or worsen detrusor overactivity. When the test is positive, it strongly points out to a neurological pathology causing the bladder disorders. IWT also allows for testing bladder sensitivity to cold. The lack of PCB is an argument for a potential central or peripheral neurological affection.
Conflict of interest statement
All authors disclose any actual or potential conflict of interest.
2
Version française
2.1
Introduction
Le réflexe mictionnel normal est déclenché par la stimulation de mécanorécepteurs qui activent des voies afférentes constituées de fibres Aδ. C’est via ces fibres myélinisées que sont véhiculées les informations concernant la réplétion vésicale et qui permettent à l’individu de savoir qu’il a besoin d’uriner . Une sensibilité vésicale normale est de ce fait nécessaire à un fonctionnement vésical adapté .
La sensibilité au froid est impliquée dans un réflexe mictionnel, appelé réflexe au froid vésical ( bladder cooling reflex ). Ce réflexe consiste en la survenue d’une contraction détrusorienne réflexe, involontaire, lors de la réalisation d’un stimulus froid endovésical. Le réflexe au froid serait médié par les fibres afférentes sensitives de type C, et intégré au niveau de la moelle sacrée . Ce réflexe spinal existe de façon physiologique chez l’enfant jusqu’à quatre ans environ, puis disparaît puisqu’il devient inhibé par les centres supraspinaux. La réapparition de ce réflexe chez l’enfant de plus de six ans ou chez l’adulte est considérée comme le témoin de lésions spinales ou du motoneurone central . Ce réflexe est comparable au réflexe cutané plantaire, signe de Babinski, physiologique chez le bébé, et réapparaissant en cas de lésion du système nerveux central .
L’interprétation des résultats du test à l’eau glacée (TEG) en termes de motricité détrusorienne est bien connue. Le TEG a une sensibilité de 65 % et une spécificité de 85 % pour le diagnostic d’hyperactivité détrusorienne et est en faveur d’une pathologie neurologique à l’origine des symptômes vésicosphinctériens . La sensibilité du TEG augmente avec sa répétition . Chez les patients souffrant de lésions médullaires, le TEG est positif pour 95 % des patients portant des lésions complètes et 86 % des patients ayant des lésions incomplètes . Toutefois, une certaine proportion de patients a priori exempts de pathologie neurologique a un TEG positif, de l’ordre de 15 % des patients . Le TEG peut être positif en cas d’obstruction sous vésicale .
La présence ou l’abolition de la perception du froid vésical (PFV) est peu étudiée. Le but de cette étude est d’analyser la PFV dans différentes populations de patients atteints ou non de pathologies neurologiques centrales ou périphériques, et de rechercher un lien entre l’altération de la PFV et la pathologie.
2.2
Patient et méthodes
Cent vingt patients ont été inclus dans l’étude. Ces 120 patients ont été répartis en quatre groupes selon leur pathologie causale. Chaque groupe comportait 30 patients :
- •
groupe 1 : patients souffrant d’hyperactivité vésicale idiopathique, sans cause neurologique ni obstructive retrouvée ;
- •
groupe 2 : patients souffrant de dysurie fonctionnelle, non obstructive et non neurologique (dyssynergies vésicosphinctériennes fonctionnelles, mégavessies congénitales, maladies du col) ;
- •
groupe 3 : patients atteints de sclérose en plaques (SEP). Ces patients avaient été adressé pour exploration de troubles vésicosphinctériens, symptomatiques :
- ∘
16 patients se plaignaient de syndrome clinique d’hyperactivité vésicale et de dysurie associée,
- ∘
dix patients présentaient un syndrome clinique d’hyperactivité vésicale isolée (urgenturie avec ou sans incontinence),
- ∘
quatre patients présentaient une dysurie et une sensation de mauvaise vidange vésicale ;
- ∘
- •
groupe 4 : patients atteints de syndrome de la queue de cheval.
2.2.1
Technique
Chaque patient a bénéficié d’une exploration urodynamique répondant aux recommandations International Continence Society (ICS) , puis d’un TEG suivant la méthodologie suivante :
- •
l’instillation d’eau glacée est précédée d’une cystomanométrie avec remplissage vésical d’eau à température ambiante et à vitesse identique à celle du TEG (100 mL par minute). Cette précaution permet de différencier une contraction détrusorienne réellement déclenchée par le stimulus froid, d’une contraction détrusorienne déclenchée par le remplissage vésical, à une vitesse et à un volume donné ;
- •
le TEG lui-même est une cystomanométrie à vitesse de remplissage de 100 mL par minute, avec de l’eau glacée (< 4 °C) .
Un TEG est considéré comme positif dans plusieurs situations, déterminant trois catégories de positivité du TEG . La réalisation d’un TEG peut permettre de démasquer une hyperactivité détrusorienne qui n’avait pas été observée sur des cystomanométries à température ambiante. Ce type de résultats permet de classer le test comme positif de classe A (si apparition de la contraction détrusorienne non inhibée avant 200 mL de remplissage) ou de classe B (si apparition de la contraction détrusorienne non inhibée entre 200 et 400 mL de remplissage). Parfois, il existe déjà une hyperactivité détrusorienne sur la cystomanométrie de base. Dans ce cas, le TEG est considéré comme positif (type C) si la contraction désinhibée du détrusor survient pour un volume infusé inférieur à la moitié du volume infusé en conditions cystomanométriques de base .
2.2.2
Étude de la perception du froid vésical
La PFV a été évaluée en questionnant les patients en fin de bilan urodynamique. La question suivante a été posée à chaque patient : « avez-vous ressenti une différence pendant ce dernier test ? ». Si les patients signalaient une sensation de froid, il leur était demandé de préciser si ce froid était ressenti au niveau vésical ou urétral, afin de ne prendre en compte que la PFV. En effet, différencier une perception de froid urétral (non considéré dans l’étude) et une véritable PFV, est important puisque la perception d’une sensation de froid au niveau urétral est beaucoup plus fréquente et ne semble pas avoir la même signification physiopathologique .
2.2.3
Statistiques
Pour les comparaisons des données moyennées, un test de Student a été réalisé, après vérification de la répartition gaussienne des valeurs étudiées et des variances. Pour la recherche de différences entre deux distributions, un test de « Chi 2 » a été réalisé. Une significativité p < 0,05 a été retenue.
2.3
Résultats
2.3.1
Analyse démographique
Les caractéristiques démographiques (âge et sexe) des patients dans les différents groupes sont résumées dans le Tableau 1 .








