Closed Reduction and Spica Casting of Femur Fractures
Howard R. Epps
Matthew R. Garner
John M. Flynn
DEFINITION
Femoral shaft fractures in children occur with an incidence of 20 per 100,000.2, 6, 14 They constitute 2% of all pediatric fractures.1, 9
In the very young child who presents with a femoral shaft fracture, child abuse must be considered, especially if the child is not yet walking.
In the child who has a history of multiple fractures, osteogenesis imperfecta might be the underlying cause and is often mistaken for child abuse in the young child.
In children who sustain multiple traumatic injuries, the nature and severity of each injury must be considered to optimize treatment.
ANATOMY
The limb bud develops at about 4 weeks age of gestation, with the femoral shaft serving as the primary ossification center. The proximal ossification center is seen by 6 months, and the distal femoral ossification center appears at 7 months.
The femur is initially composed of weaker woven bone, which is gradually replaced with lamellar bone during childhood.
Both endosteal circulation and periosteal circulation supply the femur. The profunda femoris artery gives rise to four perforating arteries, which enter the femur posteromedially. The majority of the blood is supplied by endosteal circulation. During fracture healing, however, the majority of the blood is supplied by the periosteal circulation.
The femoral shaft flares distally, forming the supracondylar area of the femur.
PATHOGENESIS
Age is an important factor to consider in terms of the pathogenesis of the injury. The degree of trauma required to cause injury increases exponentially, as the character of the bone changes and gradually becomes stronger and larger from infancy to adolescence. Low-energy injuries resulting in fractures may point to a pathologic nature of the condition, except in toddlers, in whom low-energy femur fractures are common.
The radiographic appearance of the fracture usually reflects the mechanism of injury and the force applied. High-velocity injuries usually present with more complex, comminuted patterns.
The position of the fracture fragments after the injury depends on the level of the fracture and reflects the soft tissue and muscle forces acting on the femur.
PATIENT HISTORY AND PHYSICAL FINDINGS
In most cases, there is a history of a traumatic event.
The clinician inspects the lower extremity and looks for open wounds, bruising, or obvious deformity.
In the setting of an isolated femur fracture, the thigh appears swollen with minor bruises and abrasions. Shortening may also be present.
Open wounds may change the management of this injury; obvious deformity helps in the initial diagnosis.
The clinician palpates the length of the lower extremity, feeling for bony deformity and checking compartments carefully for tension. Tense compartments may indicate current or developing compartment syndrome.
The affected extremity should be checked to ensure that there is no vascular or neurologic injury.
The clinicians should check carefully for femoral, popliteal, dorsalis pedis, and posterior tibial pulses. Diminished pulses may indicate vascular compromise or compartment syndrome. If diminished, they should be rechecked with Doppler.
Sensation to light touch is tested along the length of the entire lower extremity. Decreased sensation in the lower extremity may indicate nerve damage.
Motor examination may be difficult because of injury. Ankle dorsiflexion and plantarflexion are tested. Diminished strength may indicate nerve damage or compartment syndrome or may also be secondary to pain.
Examining reflexes may also be difficult. The clinician strikes the patellar and Achilles tendons with a reflex hammer and looks for contraction of the quadriceps and gastrocnemius, respectively. Diminished knee or ankle reflexes may indicate femoral or sciatic nerve injury or may also be secondary to guarding.
In cases of high-energy trauma, concomitant injuries to the skin and soft tissue as well as other organ systems are usually present.
The knee is examined to ensure that no ligamentous injury is present. This examination may be performed under anesthesia.
IMAGING AND OTHER DIAGNOSTIC STUDIES
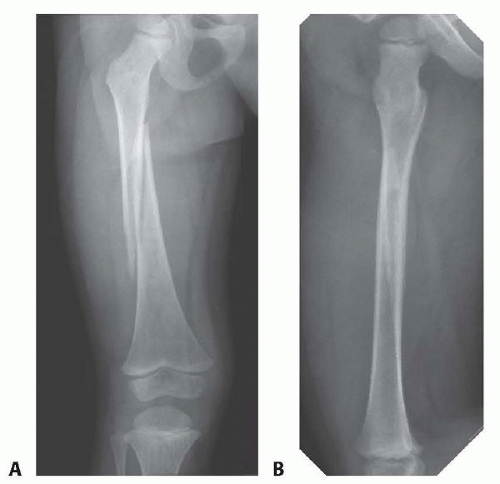
Standard high-quality anteroposterior (AP) and lateral radiographs of the femur are usually all that is needed to define the extent and severity of the injury (FIG 1).
Radiographs should include the joints above and below the fracture site to avoid missing any concomitant injuries.
Rarely, a computed tomography (CT) scan may be helpful in assessing more complex injury patterns. It also helps in revealing subtle injuries that may not be apparent on radiographs, such as stress fractures, and aids in characterizing intra-articular injuries.
DIFFERENTIAL DIAGNOSIS
Soft tissue trauma
Stress fracture
Tumor
Metabolic conditions
NONOPERATIVE MANAGEMENT
Management of femoral shaft fractures depends on the age of the patient.
In infants, stable femoral shaft fractures can be treated in a Pavlik harness or a splint.
In children younger than 6 years, closed reduction and casting is used in the vast majority of cases.
SURGICAL MANAGEMENT
In children younger than 6 years, closed reduction and casting is successful for most femoral shaft fractures.8
For older children and adolescents, 3 weeks of skeletal traction followed by spica casting was once common but has been replaced by internal or external fixation in most cases.
Preoperative Planning
A detailed review of the clinical findings and all appropriate imaging studies is performed before the procedure.
Shortening should be determined to be less than 25 mm using a lateral radiograph,11 although some suggest spica casting can be performed regardless of shortening.4, 7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree