Closed Reduction and Percutaneous Pinning of Supracondylar Fractures of the Humerus
Paul D. Choi
David L. Skaggs
DEFINITION
Supracondylar fractures of the humerus are common injuries in children. As many as 67% of children hospitalized with elbow injuries have supracondylar fractures; supracondylar fractures of the humerus represent 3% to 17% of all childhood fractures.7, 10, 11 The annual incidence of supracondylar fractures has been estimated at 177.3 per 100,000.9
The peak age at fracture is 5 to 7 years.
The cause of injury is most commonly trauma to the elbow, most often resulting from a fall from height (70%) or related to sports activities.
Nearly all (98%) supracondylar fractures of the humerus are of the extension type.1 Flexion-type injuries also occur.
Open injuries occur in 1% of cases. Concurrent fractures, most commonly involving the distal radius, scaphoid, and proximal humerus, occur in 1% of cases. Associated neurovascular injuries can occur, with nerve injury existing in 11% of cases and vascular insufficiency present in up to 20% of cases.1, 2, 10 Anterior interosseous nerve injury is the most common nerve injury associated with extension-type supracondylar fractures of the humerus.
ANATOMY
The periosteum most commonly fails anteriorly with extension-type supracondylar fractures of the humerus.
With posteromedial displacement, the periosteum also fails laterally.
Therefore, with posteromedially displaced fractures, forearm pronation can aid in the reduction (FIG 1).
With posterolateral displacement, the periosteum also fails medially.
Forearm supination usually aids in the reduction of these posterolaterally displaced fractures.
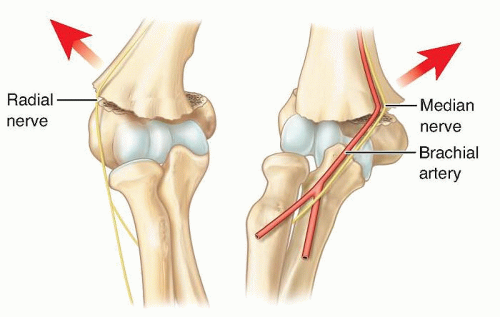
The direction of displacement has implications for which neurovascular structures are at risk from the penetrating injury of the proximal metaphyseal fragment (FIG 2).
Medial displacement of the distal fragment places the radial nerve at risk.
Lateral displacement of the distal fragment places the median nerve and brachial artery at risk.
The ulnar nerve courses through the cubital tunnel posterior to the medial epicondyle. It is at particular risk with flexion-type fractures or when a medial pin is placed for fracture fixation.
The ulnar nerve subluxates anteriorly as the elbow is flexed. Therefore, the elbow should be relatively extended if a medial pin is placed for fracture fixation.
PATHOGENESIS
Supracondylar fractures of the humerus generally occur as a result of a fall onto an outstretched hand with the elbow in full extension.
The distal humerus is very thin at the supracondylar region, a critical factor in producing a consistent injury pattern and failure in the supracondylar humeral region.
During a fall with the elbow in full extension, the olecranon in its fossa acts as a fulcrum.
The capsule, as it inserts distal to the olecranon fossa and proximal to the physis, transmits an extension force to this region, resulting in failure and fracture.
With the elbow in full extension and the elbow becoming tightly interlocked, bending forces are concentrated in the distal humeral region.
Increased ligamentous laxity, leading to hyperextension of the elbow, may be a contributing factor to this injury pattern.
NATURAL HISTORY
The physis of the distal humerus contributes little to the overall growth of the humerus (20% of the humerus); therefore,
the remodeling capacity of supracondylar fractures of the humerus is limited. Near-anatomic reduction of these fractures is important.
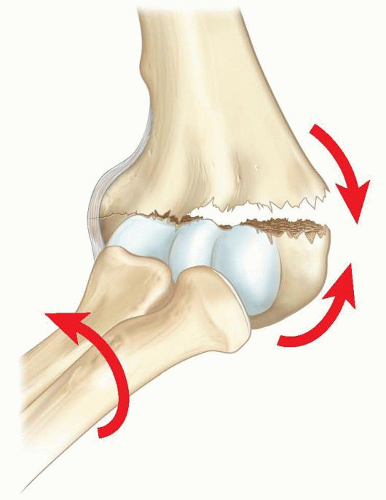
FIG 1 • Reduction of a posteromedially displaced supracondylar fracture of the humerus. Pronation of the forearm closes the hinge and aids in reduction.
The majority of supracondylar fractures of the humerus (other than extension type I fractures) are unstable; therefore, stabilization in the form of cast immobilization or, preferably, operative fixation is usually necessary.
PATIENT HISTORY AND PHYSICAL FINDINGS
Evaluation of the child with an elbow injury must include an overall assessment to look for associated trauma (especially in the proximal humerus and distal radius regions) as well as associated neurovascular injury.
The physical examination may reveal swelling, tenderness, ecchymosis, and deformity. The pucker sign, which occurs as a result of the proximal fracture fragment spike penetrating through the brachialis and anterior fascia into the subcutaneous tissue, may be present.
Thorough neurologic examination of the involved extremity is critical. Physical examinations to perform include the following:
Assessing for potential associated injury to the ulnar nerve. Finger abduction and adduction (interossei) strength are tested. Sensation in the palmar little finger is tested.
Assessing for potential associated injury to the radial nerve. Finger, wrist, and thumb extension (extensor digitorum communis, extensor indicis proprius, extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor pollicis longus) are tested. Sensation in the dorsal first web space is tested.
Assessing for potential associated injury to the median nerve. Thenar strength (abductor pollicis brevis, flexor pollicis brevis, opponens pollicis) is tested. Sensation in the palmar index finger is tested.
Assessing for potential associated injury to the anterior interosseous nerve. Index distal interphalangeal flexion (flexor digitorum profundus index) and thumb interphalangeal flexion (flexor pollicis longus) are tested.
Accurate vascular assessment of the involved extremity is also critical. Examinations to perform include the following:
Palpation of distal radial pulse
General evaluation of perfusion: capillary refill, skin temperature and color
The role of modalities like Doppler ultrasonography and pulse oximetry is still unclear.
Preoperative angiography is not usually warranted.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Initial imaging studies should include plain radiographs of the elbow—anteroposterior (AP), lateral, and sometimes oblique views.
Comparison views of the contralateral elbow are sometimes helpful.
The fat pad sign, particularly posterior, represents an intraarticular effusion and can be associated with a supracondylar fracture of the humerus (53% of the time) (FIG 3A).10
On the AP view, the Baumann angle correlates with the carrying angle and should be 70 to 78 degrees or symmetric with the contralateral elbow (FIG 3B).
On the lateral view, the anterior humeral line (line drawn along the anterior aspect of the humerus) should intersect the capitellum (FIG 3C).
This line crosses the middle third of the capitellum in most healthy children older than 4 years.
In children younger than 4 years, this line may cross the anterior one-third of the capitellum.1
The most commonly used classification system, the Gartland classification, is based on plain radiographic appearance:
Extension type I: nondisplaced
Extension type II: capitellum displaced posterior to anterior humeral line with variable amount of extension and angulation; posterior cortex of the humerus is intact
Extension type III: completely displaced with no cortex intact
A multidirectionally unstable type IV fracture has more recently been described. These fractures are unstable in both flexion and extension because of complete circumferential loss of a periosteal hinge.1, 10
Flexion type
DIFFERENTIAL DIAGNOSIS
Fracture of elbow (other than involving the supracondylar humeral region)
Salter-Harris fractures involving the elbow
Nursemaid’s elbow
Infection
NONOPERATIVE MANAGEMENT
Recent clinical practice guidelines by the American Academy of Orthopaedic Surgeons (AAOS) recommend nonsurgical immobilization of the injured limb for nondisplaced fractures (type I) meeting the following criteria4, 9:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree