Closed Reduction and External Fixation of Femoral Shaft Fractures
Afamefuna M. Nduaguba
John M. Flynn
DEFINITION
Femoral shaft fractures occur in children with a bimodal age distribution peaking at ages 2 and 12 years.1
The peak in age distribution at age 2 years is due to relative weakness of primarily woven bone at a time when ambulation increases the risk of fall-related trauma.
ANATOMY
Muscular deforming forces, if severe, increase the need for surgical fixation. In proximal and midshaft femoral shaft fractures, the proximal fragment tends to be forced into abduction and external rotation. This is more significant in proximal fractures than in midshaft fractures.
Fractures of the distal third of the femoral shaft tend not to deform greatly, whereas supracondylar femoral fractures are often forced into apex posterior angulation.
PATHOGENESIS
In toddlers, these injuries tend to be low energy and occur during normal activity. In adolescents, they tend to be higher energy injuries that may result from motor vehicle, biking, or high-speed sporting accidents.
Abuse should be considered in the infant or toddler with a femur fracture, especially if the child is nonambulatory.
PATIENT HISTORY AND PHYSICAL FINDINGS
In an unconscious patient or a patient with an insensate lower extremity, deformity, erythema, crepitance, and swelling might indicate the presence of a femoral fracture.
If child abuse is suspected, a skeletal survey should be obtained and Child Protective Services should be notified. Infants are more likely than toddlers to be the victims of child abuse in the setting of a femoral fracture.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP) and lateral radiographs of pelvis and femur are obtained. The hip and knee should be visualized as well to evaluate for possible associated injuries (FIG 1).
Radiographs should be evaluated for fracture pattern, location, displacement, angulation, and shortening.
SURGICAL MANAGEMENT
Operative management of femoral shaft fractures should be considered in any femur fracture in a child older than 5 years of age. In younger children, polytrauma, head injury, high-energy trauma, open fracture, severe comminution, or body habitus incompatible with spica cast care are relative indications for operative management.
Surgical options include flexible nailing, plating, rigid intramedullary nailing, and external fixation.
Indications specifically for external fixation include polytrauma, concomitant head injury, open fracture with severe soft tissue damage or contamination, severe comminution, and very proximal subtrochanteric or distal fractures at the diaphyseal-metaphyseal junction.
Midshaft transverse fractures are at a higher risk of refracture when treated with external fixation compared to other methods of stabilization.
PREOPERATIVE PLANNING
The surgeon should determine where pins will be placed before surgery.
In each fragment, there must be at least 2 cm of intervening bone between the physis and the outermost pin and at least 2 cm between the fracture and the innermost pin.
The appropriate pin size varies according to the device. The AO/Synthes device guide recommends 4.0-mm Schanz screws be used, whereas the EBI device guide recommends screws not larger than one-third of the bone diameter.
TECHNIQUES
▪ Biomet DFS XS Fixator Technique
Pin and Screw Placement
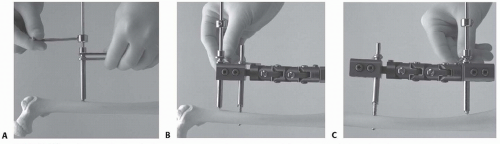
The first pin inserted should go into the shorter or more difficult bone fragment.
After making a stab incision over the first pin site, the surgeon dissects bluntly to the near cortex.
The trocar is inserted into the soft tissue guide and seated onto the femur perpendicular to its long axis. The trocar is removed, and the soft tissue guide is impacted gently to prevent slippage.
The appropriate drill guide (based on the chosen screw size) is inserted through the soft tissue guide down to bone.
After attaching a drill stop onto the appropriate bit, the surgeon drills through the near cortex, using the drill guide to keep the pilot hole perpendicular to the long axis of the bone. Drilling should stop once the near cortex is penetrated.
The surgeon slides the bit up to the far cortex without drilling. The drill stop is adjusted so that the drill can be advanced no more than 5 mm (TECH FIG 1A). The surgeon then drills through the far cortex.
The drill bit and the drill guide are removed without unseating the soft tissue guide.
The appropriate screw is inserted into the pilot hole, and the screw is advanced using the T-wrench until it protrudes 2 mm beyond the far cortex. The screw cannot be backed out of bone without losing grip because of its conical shape.
Any tented skin is released with a scalpel.
The surgeon slides the telescoping arm of the assembled fixator onto the screw in the appropriate position. The clamp bolt is not tightened.
The soft tissue guide is inserted into another clamp position on the same telescoping arm. Again, the clamp bolt should be loose enough to allow translation of the soft tissue cover through the arm.
Once the soft tissue guide has been seated on the near cortex, the clamp bolt is tightened to prevent loss of alignment. Repeating the previously mentioned steps, a second screw is inserted in the position now occupied by the soft tissue guide (TECH FIG 1B).
Once both screws have been placed in the first fragment, the previously mentioned steps are repeated on the second fragment (TECH FIG 1C).
The telescoping arm clamp bolts are tightened before final reduction.
Final Reduction
The final reduction is made with a variety of adjustments.
Length can be adjusted on each telescoping arm by either loosening the telescoping set screw and adjusting length manually or by loosening the compression-distraction screw and using this feature to adjust length (TECH FIG 2A).
The locking connector bolts can be loosened for the correction of angular deformity (TECH FIG 2B).
Each telescoping arm can also be rotated using the rotational set screw on the central body of the fixator (TECH FIG 2C). These can be loosened simultaneously to rotate the central body of the fixator to bring the central locking joints into the plane of correction (TECH FIG 2D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree