Abstract
Urinary dysfunction is a major clinical problem and a significant cause of disability in multiple sclerosis (MS) patients. Indeed, the bothersome symptom of urinary dysfunction may adversely affect social relationships and activities in MS patients. Since many causes of urinary dysfunction are described, a thorough evaluation including history, clinical examination and evaluation of quality of life is necessary. Generally, diagnosis of urinary disorders is complex with intricated pathophysiologic factors. In these cases, urodynamic investigations are necessary to better understand symptoms pathophysiology and choose the best treatment.
Résumé
Les troubles vésico-sphinctériens constituent un problème majeur au cours de la sclérose en plaques (SEP) et sont source d’handicap. En effet, la gêne induite par de tels symptômes peut affecter les relations sociales du patient et ses activités quotidiennes. En raison des très divers types et mécanismes des dysfonctions urinaires qui ont pu être décrites au cours de la SEP, une évaluation complète doit être effectuée incluant examen clinique et appréciation de la qualité de vie. La complexité des tableaux, l’intrication des mécanismes physiopathologiques justifient dans la majorité des cas la réalisation d’un bilan urodynamique pour mieux comprendre les mécanismes des troubles et déterminer au mieux la stratégie thérapeutique.
1
English version
Urinary disorders are often observed in multiple sclerosis (MS) patients . This urinary dysfunction can sometimes lead to permanent urological alterations, such as hydronephrosis, reflux, recurrent urinary tract infections, stones, renal alteration, and it always inevitably leads to diminished patient quality of life . Overactive bladder (OAB), combined with urgency, frequency, nocturia and urge incontinence, is the most common syndrome, which is sometimes also associated with voiding dysfunction and urinary retention. Clinical evaluation is always necessary. Urodynamic investigations may contribute to a better understanding of the pathophysiology of these symptoms that are generally related to overactive detrusor and detrusor sphincter dyssynergia .
1.1
Urinary dysfunction in multiple sclerosis (MS) patients
Overactive bladder and voiding dysfunction with a risk of urinary retention, are the most common symptom patterns in MS patients.
Urge incontinence is one of the main symptoms of overactive bladder. Some cases of overactive bladder can be attributed to specific conditions, such as acute or chronic urinary tract infection, and bladder stones, but most cases result from neurologic dysfunction with inability to suppress detrusor contractions. This neurogenic detrusor overactivity can be due in MS to suprapontine lesions or spinal cord lesions (above the lumbosacral level). In MS patients neurogenic detrusor overactivity is likely to be mediated by capsaicin-sensitive C-fiber afferents. In addition to changes in reflex pathways, it has been demonstrated that a functional outlet obstruction resulting from detrusor sphincter dyssynergia may alter the properties of bladder afferent neurons. Decreased afferents due to pelvic floor deficiency can lead to involuntary detrusor contraction and can be observed in MS patients specially in women. Recently, a role of the urothelium in afferent activation has been strongly suggested. It has been demonstrated that the transduction mechanisms can be altered with modification of the activation of sensory afferent fibers during bladder filling.
Voiding dysfunction and particularly urinary retention can be observed in MS patients. Underactive detrusor can be one of the mechanisms, but in fact the main cause is a detrusor external sphincter dyssynergia (DESD). DESD is characterized by involuntary contractions of the external urethral sphincter during an involuntary detrusor contraction. It is caused by neurological lesions between the brainstem (pontine micturition center) and the sacral spinal cord (sacral micturition center). This is the case in MS patients. DESD was hypothesized to be an abnormal flexor response of the perineal musculature to bladder contraction and considered as a continence reflex exaggerated owing to the loss of supraspinal influences.
This incoordination between detrusor smooth muscle and external urethral sphincter and/or bladder neck, induces an obstruction, which determines excessive bladder pressures during voiding and residual volume. Thereby, the risk of recurrent urinary tract infections, ureteral reflux, hydronephrosis and pyelonephritis, increases.
Incoordination between bladder and urethra during voiding, determines a weak stream and/or urinary retention. Urinary flow can be low during all the voiding (“tonic dyssynergia”) or can be irregularly interrupted by perineal muscle spams (“clonic dyssynergia”). Symptoms are often variable and can be influenced by general fatigue, subjet position, bladder repletion, concomitant anorectal dysfunction, urinary tract infection, urinary lithiasis, orthopaedic complications, and generally by any factor inducing spasticity increase.
1.2
Clinical evaluation
Urinary tract dysfunction during the course of MS requires full clinical evaluation since these urinary disorders represent a considerable psychosocial burden and a real risk of upper urinary tract involvement and kidney disease.
A thorough history is always the first step in the evaluation of urinary dysfunction in MS. Onset, duration of complaint, precipitants (position change, urinary tract infection), frequency, severity, quantity, number of pads, constipation, associated diseases (diabetes, surgeries, obesity), medications (e.g., anticholinergics, calcium channel blockers, diuretics, sedatives, alpha-agonists, alpha-antagonists) must be precised .
Quantitative evaluation of urinary symptoms can be done by means of specific symptoms scores.
The 24-hour bladder diary can provide an accurate record of urinary output, average voided volume, frequency of voiding, and frequency and nature of incontinent episodes, as well as type and volume of fluid intake. Patients are asked to measure their urine output in a measuring cup during any “normal” 24-hour period they choose. Since urinary dysfunction can have a major impact on all aspects of well-being in MS, this impact can be assessed by using validated condition-specific quality of life instruments (Qualiveen questionnaire can be used since this tool is validated in neurogenic patients specially in MS).
Physical examination is necessary to detect contributory factors and any underlying serious medical conditions. Evaluations should always consider associated uro-gynecologic alterations (benign prostatic hypertrophy, associated stress urinary incontinence in female MS patients). The sacral dermatomes should be tested by assessing anal tone, perineal sensation and the bulbocavernosus reflex.
Post-void residual (PVR) urine volume is assessed by catheterizing and measuring residual urine within 5 minutes after voiding (or by means of ultrasonography).
Numerous and various symptoms can be observed in MS patients .
Overactive bladder syndrome characterized by urgency, urinary frequency and/or urge incontinence is very frequent reported in 37 to 99% of patients. Obstructive symptoms with voiding dysfunction, urinary retention are also frequently reported, affecting between 34% and 79% of patients. Overactive bladder and voiding dysfunction often coexist in 50% of the cases.
The clinical presentation of vesicourethral dysfunction is variable over time and there is little correlation between the clinical and urodynamic symptomatology. Two factors are associated with presence and severity of vesicourethral dysfunction: the MS duration and the severity of the neurological deficiencies and disabilities. The prevalence of urinary dysfunction is correlated with the severity of the overall deficiencies (EDSS score). The prevalence of overactive bladder is also correlated with the importance of the pyramidal lesion but no correlation has been found concerning voiding dysfunction. To date, a link between MRI data and urological symptoms has not been established.
Current guidelines concerning management of urinary disorders in MS patients are scarce .
The first-line evaluation is based on simple parameters.
A specific questionnaire about voiding must be used in all the patients (frequency, number and easiness of voiding, appraising voiding volume, sensation of complete emptying or not), continence (number and appraising volume of leakage, use of pads), symptoms of urinary tract infection and anorectal symptoms.
Combined rapid tests of urine, “dipstick” test, is advisable for all patients with MS presenting with new bladder symptoms. Negative predictive value for ruling out urinary tract infection is excellent (98%) but the positive predictive value for confirming infection is only 50%.
In all the cases, it is necessary to track down urinary retention. A measure of post-void residual urine by supra-pubic ultrasonography or in-out catheterisation must be done.
When micturitional symptoms are discovered or spontaneously reported during this minimal evaluation, other evaluations must be performed with a three-day voiding chart, an ultrasound scan of the urinary tract, a urine bacteriology, a urodynamic study, a urinary creatinine clearance, and finally an evaluation of the impact of urinary symptoms on a quality of life scale (which may be based on the specific and validated Qualiveen Questionnaire). When risk factors are observed, e.g. high vesical pressure during the filling phase or during micturition, specific radiologic investigations must be performed (CT-scan, cystourethrography and sometimes renal scintigraphy when urinary creatinine clearance is altered).
Few guidelines are currently available .
The FLUE-MS is a tool that is easy to use in clinical practice because it comprises simple visual decision trees and clear ‘red flags’ that lead the physician to specialised advice and specific neuro-urology management in cases where there is a risk of urological complications ( Fig. 1 ).
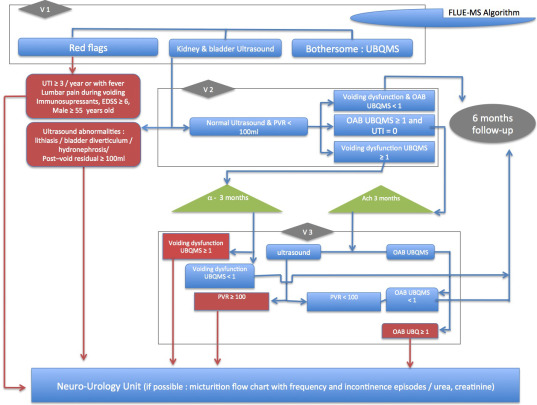
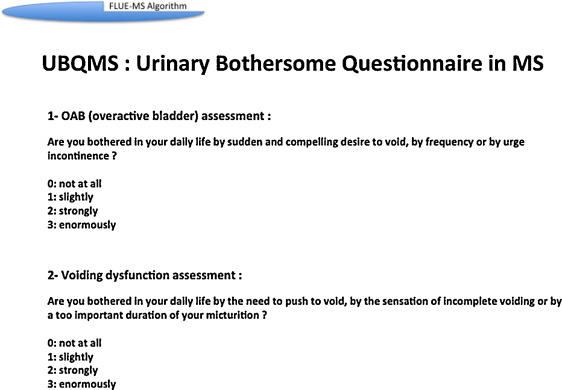
Furthermore, the incorporation of two very simple UBQMS questions that are easily comprehensible for the patient enable first-line treatment to be administered in cases of both OAB (i.e. urgency, frequency, urge incontinence) and voiding dysfunction (i.e. urinary retention) ( Fig. 2 ). These questions can be systematically answered during successive visits by patients to the neurologist or general practitioner.
FLUE-MS ‘red flags’ are highly individualised and illustrate the complications that can be expected, as reported in the published literature. Identification of one ‘red flag’ is the trigger that leads to a patient being transferred to a neuro-urologist. Recurrent urinary tract infections (UTI), i.e. more than three per year, and UTI with fever, which may indicate pyelonephritis or prostatitis, are recognised as serious risk factors that can lead to renal insufficiency.
Similarly, the presence of hydronephrosis, bladder deformities, such as diverticulum, increased bladder wall thickness and reflux, which are identifiable using ultrasound imaging, are associated with dangerous urodynamic conditions including elevated intravesical pressure, bladder compliance alteration, and severe detrusor sphincter dyssynergia.
Furthermore, post-void residual urine volume of > 100 mL, which can be evaluated by means of in-out catheterisation, often leads to a consideration as to whether there is a need to introduce intermittent catheterisation based on expert advice. Other more complex situations in which specialist intervention is required include cases where there is lumbar pain during voiding, possibly indicating vesical reflux in males > 55 years, since these patients fall within an age range in which urological problems as benign prostatic hypertrophy (BPH) may occur. The need for immune-suppressants necessitates detailed discussions about the potential presence of UTIs and their prevention, and an EDSS > 6 are all specific circumstances in which detailed evaluation and specialist treatment are required.
1.3
Urodynamic evaluation
Urodynamic explorations allow a precise evaluation of pathophysiology of urinary dysfunction and of risk factors for urinary tract damage in MS patients, thus helping to plan their optimal management. Indeed, diagnosis of urinary incontinence and more generally of urinary dysfunction, is complex with intricated pathophysiologic factors. Thus, in many cases, urodynamic investigations are necessary to better understand symptoms pathophysiology and choose the best therapeutic strategies. But in all the cases, urodynamic must be considered as a complementary investigation and always interpreted in conjunction with clinical data and the results of the others morphological and/or radiological investigations .
Measurement of the urinary flow rate (uroflowmetry) is used to confirm the presence of bladder outlet obstruction and more precisely the presence of a DESD. Urinary flow rate is measured with a flowmeter that measures a quantity of fluid passed per unit time, expressed in mL/s. Uroflow depends on detrusor contractility and urethra-sphincter resistance. Voided volume should be greater than 150 mL. Patients are instructed to void normally as in usual conditions, with a comfortably full bladder, which is sometimes difficult in these MS patients with neurogenic detrusor overactivity leading to a reduced bladder capacity. Measurement of residual urine volume (by means of ultrasounds or catheterization) is necessary to properly interpret the uroflowmetry results. The precise shape of the flow curve is decided by detrusor contractility, the presence of any abdominal straining and by the bladder outlet. A normal flow curve is a smooth curve without any rapid changes in amplitude. Rapid changes in flowrate may evoke detrusor sphincter dyssynergia with lack of urethral sphincter relaxation during micturition and sometimes involontary flow interruption and abdominal straining.
Cystometry is the method used to measure the pressure-volume relationships of the bladder. The intravesical pressure is measured while the bladder is filled, but this simple technique is not accurate because intravesical pressure does not represent in all the cases the true detrusor pressure: as the bladder is an intra-abdominal organ, the intravesical pressure is subjected to changes (during cough, patient movements…) and not represent the real detrusor pressure. Thus, it is more appropriate to use substracted cystometry, which involves measurement of both the intravesical and intra-abdominal pressure simultaneously. Electronic substraction of the intra-abdominal pressure from the intravesical pressure enables detrusor pressure measurements. In current practice intra-abdominal pressure is estimated from rectal pressure. In MS patients in complete urinary retention (for example under self intermittent catherisation), only bladder pressure without rectal pressure measurement can be used. Urinary tract infection should always be checked before urodynamic investigation. Artificial bladder filling is used, via a catheter, with sterile water or normal saline. The filling phase starts when filling commences and ends when the patient and urodynamic expert decide that “permission to void” has been given. In current practice the filling rate is usually 50 mL/min. Different events must be analysed during filling and voiding phases: first sensation of bladder filling (feeling of the bladder filling), first desire to void, strong desire to void. Increased bladder sensation is defined as an early first sensation of bladder filling (or an early desire to void) and/or an early strong desire to void, which occurs at low bladder volume and which persists. Reduced bladder sensation is defined as diminished sensation throughout bladder filling. Absent bladder sensation means that, during filling cystometry, the individual has no bladder sensation. Urgency, during filling cystometry, is a sudden compelling desire to void.
Assessment of the detrusor function during filling cystometry is one of the major goals of the urodynamic investigation in MS patients with urinary dysfunction. All detrusor activity before the “permission to void” is defined as “involuntary detrusor activity”. Normal detrusor function is defined as bladder filling with little or no change in pressure. No involuntary phasic contractions occur despite provocation (rapid filling, ice water, postural changes, hand washing). Detrusor overactivity is a urodynamic observation characterised by involuntary detrusor contractions during the filling phase which may be spontaneous or provoked. In MS, there are certain patterns of detrusor overactivity: phasic detrusor overactivity is defined by a characteristic wave form and may or may not lead to urinary; terminal detrusor overactivity is defined as a single, involuntary detrusor contraction, occurring at cystometric capacity, which cannot be suppressed and results in incontinence usually resulting in bladder emptying (voiding).
Bladder compliance describes the relationship between change in bladder volume and change in detrusor pressure. Compliance (C) is calculated by dividing the volume change (ΔV) by the change in detrusor pressure (Δpdet) during any change in bladder volume (C= ΔV/Δpdet). Cystometric capacity is the bladder volume at the end of the filling cystometrogram, when “permission to void” is usually given.
The most frequent cystomanometric finding in MS patients is detrusor overactivity (mean occurrence of 65%, ranges from 34% to 99%) followed by detrusor underactivity (mean occurrence of 25%, ranges from 0% to 40%) and poor bladder compliance (2 to10%). Detrusor sphincter dyssynergia is observed in 35% of the patients. Cystometry can be considered normal in 1/3 of symptomatic patients. Cystometrogram may change over time independently of any micturitional and neurological clinical stability.
There is no influence of age on the urodynamic patterns but in contrary, gender may be an independent factor of influence, with a significant increase in the maximum amplitude of the involuntary detrusor contractions, of the detrusor leak point pressure (lowest detrusor pressure at which urine leakage occurs in the absence of either a detrusor contraction or increased abdominal pressure) and of the maximum detrusor pressure in men as compared to women. Duration of the MS evolution is only correlated with the presence or not of a detrusor sphincter dyssynergia.
There is no specific urodynamic presentation linked to progression form, remittent or progressive, although a link has been reported between the MS activity and urodynamic presentation.
The correlation between detrusor overactivity, detrusor sphincter dyssynergia and the severity of sensory-motor deficiencies (EDSS) or of pyramidal damage appears probable. In contrary, no correlation between underactive detrusor and neurological status has been found. Finally, the existence of a correlation between certain lesion levels and the cystomanometric data remains controversial, but the presence of encephalic or suprasacral lesions and lesions on the brain stem may be a predisposing factor for dyssynergia and detrusor underactivity respectively.
Urodynamic investigations allow the diagnosis of DESD in MS patients with voiding dysfunction. The classic test to recognize detrusor external sphincter dyssynergia is combined cystometry and external sphincter electromyography. Meanwhile, DESD can be suggested if a flowmetry examination is possible to perform, when an interrupted urine flow with residual volume are observed.
Cystometry may be recorded with a rectal pressure measurement to analyse abdominal pressure simultaneously with bladder pressure to eliminate artifacts due to abdominal muscle contraction. Indeed, the diagnosis of DESD requires a detrusor contraction. However, many MS patients are unable to initiate such a contraction, particularly in severe DESD. Furthermore, in moderate DESD, some patients will strain to try to urinate, which causes a simultaneous increase in sphincter activity, bladder and rectal pressure. Sphincter dyssynergia is diagnosed by increased EMG activity during an involuntary detrusor contraction. DESD is further suggested by a high voiding pressure, persistent elevated MUP (maximal urethral pressure). Smooth sphincter dyssynergia is more difficult to confirm. Video imaging techniques allow the diagnosis of bladder neck dyssynergia. Fluoroscopic imaging during an involuntary contraction objectifies persistent narrowing of the internal sphincter and/or of the bladder neck.
When the micturition is possible, combined uroflow and sphincter EMG (eventually with a single rectal pressure record) allow DESD screening.
In fact, a very common and important question, is whether dyssynergia can be diagnosed in the absence of a bladder contaction. Even if the DESD rigorous definition is not applicable, we can consider that DESD is the only mechanism of urinary retention in a MS patient who have overactive bladder without bladder neck or urethral organic obstruction (urethral stenosis, prostatic hypertrophy).
However, recognizing DESD is not the main problem in the management of MS bladder. The real challenge is not to prove absolutely DESD with urodynamic tests, but to evaluate its consequences, especially high detrusor pressure during storage and/or micturition, which can determine bladder or renal complications.
1.4
Conclusion
Urinary incontinence, overactive bladder and more generally urinary dysfunction is a major clinical problem and a significant cause of disability in MS patients. Indeed, the bothersome symptom of urinary dysfunction may adversely affect social relationships and activities in these patients. Since many causes of urinary dysfunction are described, a thorough evaluation including history, clinical examination and evaluation of quality of life is necessary.
Clinical evaluation is still the main step in the management of urinary disorders in MS. Questionnaires are highly recommended and significantly improve symptoms comprehension and therapeutic decision. Investigations, biological, radiological or urodynamic are indicated in all symptomatic patients. Specific algorythms such as FLUE-MS, can be used in order to track down any complications and help to a better follow-up of the patients.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



