Abstract
Objectives
Analyzing the literature and elaborating recommendations on the following topics: relevance of dorsal root entry zone (DREZ) lesions, surgical treatment for posttraumatic syringomyelia, other therapeutic approaches (peripheral nerve root pain, nerve trunk pain and Sign Posterior Cord [SCI] pain).
Material and Methods
The methodology used, proposed by the French Society of Physical Medicine and Rehabilitation (SOFMER), includes a systematic review of the literature, the gathering of information regarding current clinical practices and a validation by a multidisciplinary panel of experts.
Results
Ninety-two articles were selected, 10 with a level of evidence at 2, 82 with a level of evidence at 4. Some articles lacked information on the type of injury, the pain characteristics and the symptoms’ evolution over time.
Drez
This type of procedure has been validated for its effectiveness on pain at the level of injury (transitional zone pain), but is inefficient for pain located below the level of injury. Posttraumatic syringomyelia (PTS): suspected when there is an increased neurological impairment, changes below the level of injury (mainly bladder dysfunctions) or a sudden onset of pain. The surgery associates arachnoid grafting, cyst drainage, expansile dural plasty (same treatment for posttraumatic tethered spinal cord and posttraumatic myelomalacia).
Peripheral nerve root, nerve trunk or transitional zone pain
Surgical implants (screws or clips) can generate radicular pain caused by inflammation and they can even move around with time. The material-induced constraints can also trigger pain. Surgical removal of osteosynthesis material (with an eventual saddle block) remains a simple procedure yielding good results. Correcting surgeries can also be performed (malunion and nonunion). Finally, compressive neuropathies (carpal tunnel syndrome, ulnar nerve entrapment) already have a well-defined treatment.
Conclusion
The literature review can define the relevance of surgical treatments on some types of SCI pain. However, the results of many articles are difficult to analyze, as they do not report clinical or follow-up data.
Résumé
Objectifs
Analyse de la littérature et élaboration de recommandations sur les thèmes suivants : place de la drezotomie, traitement chirurgical de la syringomyélie post-traumatique, autres approches thérapeutiques (douleurs radiculaires, rachidiennes et tronculaires périphériques).
Matériel et méthodes
La méthodologie utilisée est celle proposée par la Société française de médecine physique et de réadaptation (Sofmer), elle associe une revue systématique de la littérature, un recueil des pratiques professionnelles, une validation par un panel pluridisciplinaire d’experts.
Résultats
Quatre-vingt-douze articles retenus, dix de niveau de preuve 2, 82 de niveau de preuve 4. Caractère très incomplet des articles quant au type d’atteinte neurologique, aux caractéristiques douloureuses et à l’évolution des symptômes dans le temps .
Drezotomie
Indiscutable dans les douleurs lésionnelles, inefficace dans les douleurs sous-lésionnelles. Syringomyélie post-traumatique : suspectée devant l’ascension du déficit neurologique, la modification du comportement sous lésionnel (notamment mictionnel), ou l’apparition de douleurs. La chirurgie associe l’arachnoïdolyse, le drainage du kyste, la plastie d’agrandissement (même traitement pour les moelles attachées et les myélomalacies post-traumatiques).
Douleurs radiculaires, rachidiennes et tronculaires périphériques
Vis ou crochets peuvent générer une radiculalgie et peuvent se déplacer dans le temps. Les contraintes imposées par le matériel peuvent générer des douleurs. L’ablation de l’ostéosynthèse (éventuellement accompagnée d’une radiculolyse) reste un geste simple et souvent positif dans ses résultats. La correction de déformations peut aussi être pratiquée (pseudarthroses, cals vicieux). Enfin, les compressions tronculaires auxquelles il faut penser (canal carpien, nerf ulnaire au coude) ont un traitement bien établi.
Conclusion
La revue de la littérature permet de définir la place de la chirurgie sur certaines douleurs du blessé médullaire. À noter le caractère imprécis de nombreux articles (données cliniques et évolutives), les rendant difficilement exploitables.
1
English version
1.1
Introduction
The objective is to define the relevance of surgical treatments (except central neurostimulation) on Sign Posterior Cord (SCI) pain and to evaluate the relevance and effectiveness of DREZ, surgery for posttraumatic syringomyelia (PTS) and other similar pathologies – for posttraumatic tethered spinal cord and posttraumatic myelomalacia that can be the first stage of a syrinx cavity formation –, for which we need to refine the various modalities. Finally, what can we do for the other types of pain, radicular pain, nerve trunk peripheral pain but also segmental pain? The literature review highlighted a therapeutic strategy for these various situations.
1.2
Material and method
For this literature review, our bibliographical search used the following keywords: chronic neuropathic pain in spinal cord injury/ human/ adult AND surgical approaches/ Dorsal root entry zone (DREZ) lesioning/ surgical treatment of posttraumatic syringomyelia/ cord detethering/ arachnoiditis/ nerve decompression/ root decompression/ spinal surgery. The quality of each article was evaluated using the grid from the French Health Authority (HAS) (see general article on methodology).
1.3
Results
Of all the articles reviewed, 92 were selected. In fact, many articles on this topic focused on the pathophysiology of pain and were considered too general and far from the themes we wanted to work on. We kept five grade A articles, five grade B articles and 82 grade C articles.
We discovered that most publications were quite incomplete regarding the type of spinal cord injury (paraplegia or tetraplegia, complete or incomplete SCI, neurological level of injury), the types of neuropathic pain (below, above or at the level of injury) and the evolution of the symptoms in time. Often, there were no available results for a given treatment and the severity of the pain is not quantified either with the validated pain scales or with functional or behavioral scales.
1.4
Dorsal root entry zone lesion (DREZ)
1.4.1
Procedure
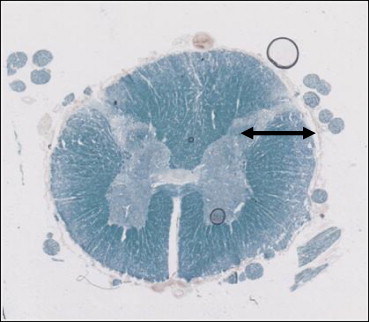
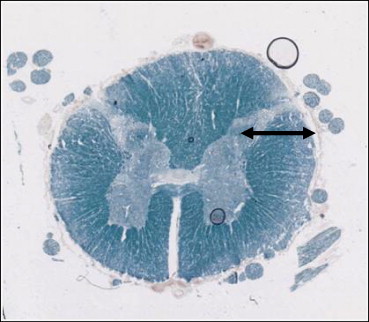
To section the small pain fibers as they enter the spinal cord in the tip of the dorsal horn ( Fig. 2 ).
1.4.2
Literature analysis
There is a consensus for limiting it to segmental pain (at the level of injury). It is very efficient – up to 70% of good results in lower SCI injury levels, conus medullaris injury for example, but mainly for incomplete SCI – .
Technical indication: it is recommended to go up above the injury level.
1.4.3
Drawbacks/complications
There is a minimal risk to further impair the motor functions. The risk of triggering deafferentation-related pain is also minimal. Nevertheless, up to 30% of complications were reported, mainly for bladder/bowel functions, if the technique is bilateral .
1.4.4
Choosing the techniques
DREZ microcoagulation is the classic technique. Radiofrequency DREZ, laser DREZ or computer-assisted (CA) DREZ are more and more performed. Globally, radiofrequency DREZ reports better results than laser DREZ. CA DREZ is more specific because it can target the neurons with an identified hyperactivity, leading to a more selective destruction of the pain-triggering targets. . In fact, in the literature it seems that the authors promote their own technique, without any reliable study comparing all these different procedures. For laser DREZ, YAG laser is deemed more efficient than CO2 laser. It is cheaper – interdisciplinary transversal use – and reports less risks of adverse events. However, it is criticized for its “all or nothing” characteristics (useless or excessive destruction). They report that the effectiveness of radiofrequency DREZ depends more on the temperature chosen than the intensity. CA DREZ, by detecting more specifically the hyperactive neurons, can yield up to 78% of positive results .
1.5
Discussion
Unfortunately, this review unveils the lack of clinical descriptions, especially regarding the level of injury. Two meta-analyses showed that studies often lacked a control group as well as inclusion/exclusion criteria. There is usually no information on the SCI: complete or incomplete, levels of injury. The risks are often not reported or with very few information and the improvement percentages are often forgotten .
Globally, DREZ is a validated technique, effective on segmental pain at the level of injury, mainly for the lower injury levels, incomplete SCI and for unilateral pain. The procedure must be extended to the contiguous metameters above the level of injury and, at best, be guided by recording the neuronal hyperactivity, which is the first cause of pain.
1.5.1
Posttraumatic syringomyelia (PTS) (Grade C Recommendation)
This is a common pathology affecting up to 28% of SCI patients corroborating the reports from autopsic studies (20%) , and largely exceeds the first estimates (3%) . Of course, not all patients will go on to develop clinical symptoms, but being aware of the prevalence of this affection can help professionals to educate their patients to avoid actions such as straining or Valsalva-type activities that may trigger or worsen the symptoms.
Pain is usually the first clinical symptom of syringomyelia with a prevalence estimated between 37 to 80% . This pain is usually located at the level of injury (segmental pain).
The therapeutic modalities take into account the pathophysiology of the affection. Everybody, except in rare cases, agrees with the Williams theory referring to the blockage of the cerebrospinal fluid (CSF) at the level of injury by a vertebral-disc compression and/or by a simple arachnoiditis thus forcing CSF in the cystic cavity, resulting in expansion and extension.
The therapeutic modalities include the shunting of syrinx cavities, arachnoid grafting, and duraplasty for CSF bypass.
All shunting procedures report similar results when used alone: subarachnoid, syringoperitoneal, and syringopleural. The results report from 12 to 53% of successful cases, 10 to 56% of patients who underwent this procedure do not report any improvement and 12 to 32% report a surgery-triggered aggravation . There are some risks: a low-pressure cerebrospinal fluid state, shunt failure, infection amounting to 16% of immediate complications, thus this surgical procedure should not be performed alone.
Can we improve the results by adapting the technique? Ultrasound imaging during surgery can help evaluate the cyst drainage . Complete marsupialization is sometimes performed but the risks are obvious; implanting valves on syringoperitoneal shunts to decrease postdural puncture headache (PDPH) can increase the risk of shunt malfunction.
Finally, if we agree on cyst drainage, one of the issues is that septa are often detected. Some consider that we should not necessarily collapse them , others considering it useful to perform endoscopic membrane collapsing . We should discard extreme solutions (cordectomy), or non-validated and anecdotic procedures (myelopiccolotomy, perispinal omental grafting for blood circulation).
According to Williams’ criteria, the treatment must include arachnoid grafting and duraplasty in addition to the shunt. The result with this combined procedure at five-year follow-up reports over 50% of improved patients (vs. 15% with the shunting procedure alone) .
In fact, the therapeutics options are becoming more consensual and the following triad is often proposed : arachnoid grafting, subarachnoid drain and expansile duraplasty. Nashold even suggested associating it to DREZ for an even better treatment of segmental pain .
The effectiveness of rational surgery is obvious: 70% at two years , 70% at three years , 72% at three years , 73% at one year , 85% at seven years .
However, in the various articles selected, pain is rarely correctly identified for this indication, it is not defined whether the pain is solely located at the level of injury or also above the level of injury. Pain below the level of injury is not mentioned in this indication.
1.5.2
To sum up, what kind of surgery should we offer?
It is well admitted that surgery must take into account the pathophysiology. The suggested methods are as follows:
- •
drainage: all systems are similar . The literature analysis reports 12 to 53% of successful cases, 10 to 56% of patients who underwent this procedure do not report any improvement and 12 to 32% report a surgery-triggered aggravation. If we add the 16% of immediate complications , due to a low-pressure cerebrospinal fluid state, shunt failure or infection and the fact that only 15% of the shunts are still working after five years , this technique, used alone, is not valid anymore;
- •
the validated technique is now more complete since it combines: arachnoid grafting, cyst drainage and/or complete marsupialization with an expansile duraplasty. This combined technique can bring an improvement of the disorders in 75% of cases with a significant impact on pain.
There is additional information that could be essential for postsurgical care. Some authors suggest , after performing an arachnoid grafting and duraplasty, the early mobilization of patients after surgery to avoid new adherences that tend to have a very early onset. This might also be relevant for other surgeries – herniated disc, carpal tunnel syndrome, etc.
1.5.3
When should the surgery take place?
If everybody agrees that the surgery should take place when there is a worsening of the neurological symptoms above the initial level of injury, the primary indication remains the onset of pain, first symptom of the disease with an estimated prevalence going from 37 to 80% .
1.5.4
Should we wait for the onset of syringomyelia?
Lee et al. advocate a surgery similar to the one performed for the syrinx in patients with a tethered cord and/or a posttraumatic myelomalacia. The symptoms are similar: impaired motor functions above the level of injury, autonomic dysreflexia, pain (undefined), bladder/bowel dysfunctions, and sensory impairment. It is important to note that a proper follow-up and monitoring of these patients, using the latest imaging techniques could help identify a potential condition and thus act before the cyst formation. Lee et al. report a 62% success rate for positive impact of the surgery on pain, but here again, there is no data on long-term follow-up, pain characteristics or pain intensity.
1.6
The other surgical techniques (Grade C recommendations)
Regarding compressive neuropathies, the major incidence increase for the two main neuropathies – carpal tunnel syndrome and ulnar nerve entrapment – is well-known and should be evoked when faced with pain and/or motor impairments in these nerve trunk areas. The treatment is a classic one: test or treatment injections for the former and nerve trunk transposition surgery for the latter. It is important to identify some syndromes that are rare but that can be triggered by being in a wheelchair and the ensuing efforts: thoracic outlet syndrome (TOS) and pudendal neuropathy (PN). TOS must be identified and differentiated from a worsening of the neurological disorders as seen in syringomyelia; PN must be evoked when faced with perineal pain when lying down.
Regarding radicular pain with a fast onset, it is essential to verify the position of the surgical implants (screws or clips) that can generate pain if it had an early onset. Later on, it is important to look for dislocated material and/or the worsening of kyphosis that can reduce the intervertebral foramen. SCI patients should benefit from multidisciplinary care and the surgeon should be involved in the monitoring and follow-up of patients. The surgeon can decide, even a long time after the initial injury, to perform an arthrodesis for non-union or even a simple surgical removal of the osteosynthesis material, we found no data on this topic, besides one article explaining the necessity of X-ray monitoring for the implanted material, since any dislocation or displacement can trigger spinal cord pain that can be mistaken for segmental pain . Our experience showed that it is a useful tool for segmental pain. Larson recommends associating spinal cord decompression to the surgical removal of the material .
Regarding sacral pain, a myelotomy of the conus medullaris is suggested by Livshits et al. , especially when there is spasticity.
Richards et al. brings important information: for gunshot SCI, surgically removing the bullet does not have an impact on the pain.
Spinal cord decompression should be systematically considered in the initial posterior approach in thoracolumbar trauma (laminectomy). It is mandatory when faced with the onset of Lhermitte’s SCI Syndrome that are aggravated in incomplete SCI.
1.7
General discussion
The data from the literature highlights the fact that the factors generating pain below the level of injury are very poorly understood. This pain is most probably neuropathic but is not similar to the pain felt by amputated patients. Many factors still need to be discovered that could explain how the spinal cord below the lesion restructures itself with the ensuing symptomatic outcomes.
The main issue is the lack of information found in the literature. The articles do not mention the level of injury, the completeness of the neurological lesion or the quantified results for studies that looked quite promising. Authors seem to be conducting their own experiences by themselves. Progress can only be made if prospective studies are conducted by using the various technical methods suggested.
DREZ is highly relevant for treating segmental pain at the level of injury. The vote for the attendees at the experts conference shows that 28% of specialists had no opinion, 10% found its indication for segmental pain. We should not forget the local disorders – badly implanted surgical material (screws, clips) in the initial surgery, implants mobility later on, relevance of cord detethering surgery.
The surgical treatment of syringomyelia takes into account the validated Williams’ criteria: spinal cord decompression and restoring the CSF flow by arachnoid grafting, subarachnoid drain and expansile duraplasty. The attendees’ vote shows the rare use of surgery for pain treatment in this indication (only 14%); most physicians prefer to wait for the onset of motor impairment above the level of injury to refer their patients to a surgeon (34%). Other similar pathologies (posttraumatic myelomalacia, posttraumatic tethered cord) can benefit from the same treatment except of course the drainage.
Regarding radicular pain and the use of additional X-rays to find the cause (malunion, non-union, dislocated material), we note that the attendees votes show that 14% of physicians had no opinion, and that for a quarter of them they never recommend these surgeries. Whereas, it is a simple method to try and address the pain issue that is not easy to solve when no cause is found. This also advocates the needs for multidisciplinary care (medical and surgical) for treating SCI patients. Finally, the peripheral nerve trunk compressive syndromes must be addressed and treated accordingly.
1.8
Conclusion
Surgery can be effective in treating the pain of posttraumatic SCI patients. It is widely admitted that in most cases DREZ can resolve the issue of segmental pain; the treatment of syringomyelia is well defined just like for similar pathologies: posttraumatic myelomalacia, posttraumatic tethered cord. We should not forget the other pain-triggering factors such as osteosynthesis implants, malunion and non-union. Finally, the wheelchair position and sitting behavior require efforts that can have a negative impact on the peripheral nerve trunks. This is true for carpal tunnel syndrome and ulnar nerve entrapment, but also other syndromes that could be overlooked in this nosological framework such as: thoracic outlet syndrome (TOS) and pudendal neuropathy (PN).
The literature highlights the rare articles that are valid on a scientific level; authors promote their own techniques without sufficient semiological data that could lead to a positive reading of the results. Only prospective studies can validate new surgical techniques, knowing that segmental pain benefits from more options. Pain above the level of injury should evoke either a syringomyelia or compressive neuropathies. Regarding pain below the level of injury it is still badly understood and thus hard to treat.
1.9
Appendix 1: Results from the questions asked to the 166 physicians who attended the Experts Conference and the 50 others who answered via the SOFMER website
DREZ
What are in your opinion the indications for DREZ?
- •
28%: no opinion;
- •
10%: segmental pain at the level of injury;
- •
2% pain above the level of injury;
- •
8% pain below the level of injury;
- •
50% pain is refractory to medical treatments;
- •
2% segmental pain for cauda equina syndrome.
Syrinx
Clinical criteria for surgery
- •
12%: syrinx volume;
- •
14%: pain;
- •
8%: refractory to medical treatments;
- •
12%: impairment below the level of injury;
- •
34%: motor impairment above the level of injury.
Other surgical techniques
Do you systematically prescribe X-rays of the traumatic injury area in case of radicular pain?
- •
14%: no opinion;
- •
62%: yes;
- •
24%: no.
2
Version française
2.1
Introduction
L’objectif est de définir la place de la chirurgie (à l’exception des neurostimulations centrales) dans les douleurs du blessé médullaire et d’apprécier en la précisant la place de la drezotomie, la place de la chirurgie lors des syringomyélies post-traumatiques et les états voisins (moelle attachée, myélomalacie qui peuvent du reste être le prélude au syrinx), chirurgie dont il faut préciser les modalités. Enfin, que peut-on faire pour les autres douleurs, radiculaires, tronculaires périphériques, mais aussi rachidiennes ? La revue de la littérature nous a permis de dessiner la conduite à tenir thérapeutique pour ces différentes situations.
2.2
Matériel et méthode
Pour faire la revue de la littérature sur ce sujet, la recherche bibliographique a utilisé les mots clés suivants : chronic neuropathic pain in spinal cord injury/ human/ adult AND surgical approaches/ Dorsal root entry zone (Drez)lesioning/ surgical treatment of posttraumatic syringomyelia/ cord detethering/ arachnoiditis/ nerve decompression/ root decompression/ spinal surgery . La qualité de chaque article a été évaluée à l’aide de la grille de la haute autorité (voir article général sur la méthodologie).
2.3
Résultats
Sur les articles consultés dans la littérature, 92 ont été retenus. Bien des articles en effet qui traitent de ce sujet sont axés sur la physiopathologie de la douleur et ont été considérés comme trop abstraits et distants des thèmes que nous voulions aborder. Nous avons retenu cinq articles de grade A, cinq de grade B, 82 de grade C.
Il faut surtout noter le caractère très incomplet des publications concernant notamment le type d’atteinte neurologique (para- ou tétraplégique, complet ou incomplet, niveau lésionnel), les caractéristiques de la douleur (supra-, infra- ou lésionnelle) et l’évolution des symptômes dans le temps. Bien souvent aussi, les résultats d’un traitement proposé ne sont pas donnés et l’importance des douleurs n’est pas quantifiée ni par les échelles validées, ni par les échelles fonctionnelles ou comportementales.
2.4
La drezotomie
2.4.1
Principe
Elle consiste à sectionner les fibres sensitives de petit calibre à leur entrée dans l’apex de la corne grise dorsale de la moelle spinale ( Fig. 1 ) .