Chronic Exertional Compartment Syndrome
Jonathan A. Godin
Jocelyn R. Wittstein
L. Scott Levin
Claude T. Moorman III
DEFINITION
Compartment syndrome can be either acute or chronic.
Acute compartment syndrome is usually due to trauma to, or reperfusion of, the extremity. Chronic exertional compartment syndrome (CECS) is often associated with the repetitive loading or microtrauma of endurance activities.
Both acute and chronic compartment syndromes are due to increased interstitial pressure within a compartment, resulting in decreased perfusion and ischemia of soft tissues.
In contrast to the reversible nature of CECS, acute compartment syndromes progress rapidly and require urgent fasciotomy to avoid irreversible soft tissue necrosis in the affected compartment.
Wilson first described the concept of CECS in 1912, but Mavor16 was the first to successfully treat a patient with anterior compartment syndrome of the leg using a fasciotomy.
Clinical manifestations of compartment syndrome include exercise-induced pain relieved by rest, swelling, numbness, and weakness of the extremity.8, 23
CECS is often bilateral and is equally prevalent among males and females.
Diabetic patients may be at increased risk of developing CECS.6
The leg is the most common site, with the anterior and lateral compartments most frequently affected. Although this chapter focuses on CECS of the leg, the clinical features, diagnostic strategy, and treatment methods are similar for all locations.
ANATOMY
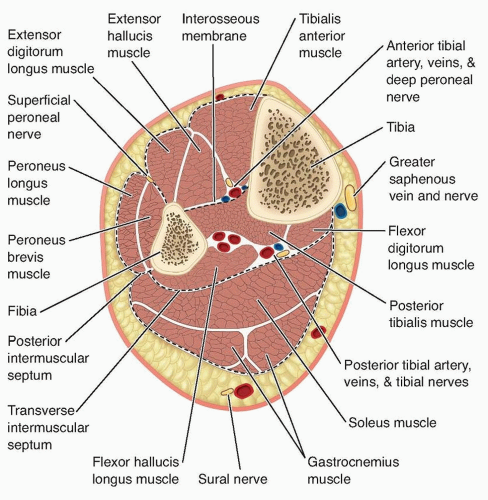
The leg contains four compartments: anterior, lateral, superficial posterior, and deep posterior (FIG 1).
The anterior compartment contains the anterior tibial artery, the deep peroneal nerve, and four muscles (tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius). Its borders are the tibia, fibula, interosseous membrane, anterior intermuscular septum, and deep fascia of the leg.
The lateral compartment contains the superficial peroneal nerve and two muscles (peroneus longus and peroneus brevis). Its borders are the anterior intermuscular septum, the fibula, the posterior intermuscular septum, and the deep fascia.
The common peroneal nerve branches into the superficial and deep peroneal nerves within the substance of the peroneus longus after passing along the neck of the fibula.
The superficial peroneal nerve continues within the lateral compartment, whereas the deep peroneal nerve wraps around the fibula deep to the extensor digitorum longus until reaching the anterior surface of the interosseous membrane.
The lateral compartment does not contain a large artery; the peroneal muscles receive their blood supply via several branches of the peroneal artery.
The superficial posterior compartment contains the sural nerve and three muscles (gastrocnemius, soleus, and plantaris) and is surrounded by the deep fascia of the leg.
The deep posterior compartment contains the posterior tibial and peroneal arteries, tibial nerve, and four muscles (flexor digitorum longus, flexor hallucis longus, popliteus, and tibialis posterior). It is bordered anteriorly by the tibia, fibula, and interosseous membrane and posteriorly by the deep transverse fascia.
A fifth compartment that encloses the tibialis posterior muscle has been described,4 but its existence is controversial. It has been suggested that the presence of an extensive fibular origin of the flexor digitorum longus muscle may create a subcompartment within the deep posterior compartment that may develop elevated pressures.11
PATHOGENESIS
The etiology of CECS is not entirely understood. It is thought to be due to an abnormal increase in intramuscular pressure during exercise resulting in impaired local perfusion, tissue ischemia, and pain.
One study demonstrated a 20% increase in muscle volume during exercise.15
Contributing factors may include exertion-induced swelling of the muscle fibers, increased perfusion volume, and increased interstitial fluid volume within a constrictive compartment.
The elevated intramuscular pressure decreases arteriolar blood flow and diminishes venous return.
This, in turn, results in tissue ischemia and accumulation of metabolites.
Elevated lactate levels and water content have been documented in muscle biopsies from compartments with elevated pressures following exercise.21
Muscle hypertrophy and increased perfusion volume with exertion do not explain the elevated resting pressure seen in patients with CECS, however. The mechanical damage theory hypothesizes that heavy exertion results in myofibril damage, release of protein-bound ions, increased osmotic pressure in the interstitial space, and, therefore, decreased arteriolar flow in the compartment.
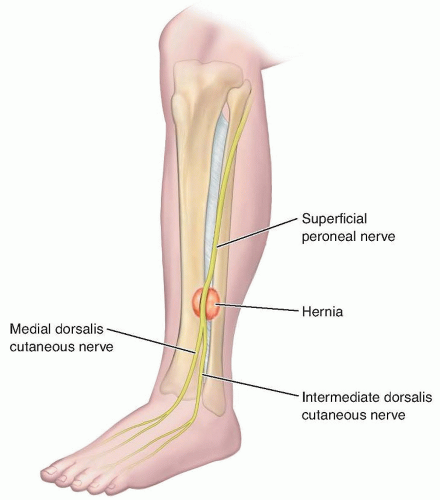
Additionally, in some cases, focal fascial defects may be a contributing factor.
Anterolateral fascial hernias are present in 39% to 46% of patients with CECS, as compared to less than 5% of asymptomatic individuals.9, 31
These defects typically are located near the anterior intermuscular septum between the anterior and lateral compartments, and they can entrap the superficial peroneal nerve exiting the junction of the middle and distal thirds of the leg (FIG 2).
Evidence suggests that patients with CECS have a lower capillary density in relation to muscle fiber size compared to controls. This decreased capillarity leads to decreased structural capacity for muscle blood flow.7
None of the existing theories explain all of the available data on the etiology of CECS. Most likely, the pathogenesis of the elevated intracompartmental pressures seen in CECS is multifactorial.
NATURAL HISTORY
CECS of the leg is a common injury in people involved in running and endurance sport activities, such as young athletes and military personnel.
Pain, as well as occasional numbness and weakness, develops at a predictable interval after initiation of a repetitive, endurance-type activity and resolves with rest.
The symptoms are long-standing and recurrent because patients tend to self-limit before subsequently attempting to resume activities.
PATIENT HISTORY AND PHYSICAL FINDINGS
The following symptoms may be present upon exertion and resolve with rest:
A sensation of cramping, burning, aching, or tightness in the region of the affected compartment(s)
Numbness or weakness in the extremity
A transient foot drop may develop if the deep peroneal nerve is affected.
A temporary loss of eversion strength may occur if the superficial peroneal nerve is affected.
Physical examination of the resting lower extremity often is unremarkable.
Examination following exercise may reveal the following:
Tightness or tenderness to palpation of the involved compartments
If a fascial defect is present, a focal area of tenderness and swelling may develop as the underlying muscle bulges through the defect.
A positive Tinel sign over the defect if the superficial peroneal nerve is compressed
Numbness and/or motor weakness may be present in the superficial peroneal, deep peroneal, or tibial nerve distributions.
When the history and physical examination findings are consistent with CECS, the diagnosis should be confirmed with pre- and postexercise compartment pressure measurements.
Most clinicians follow the diagnostic criteria of Pedowitz et al,20 in which a resting pressure greater than or equal to 15 mm Hg or a 1-minute postexercise measurement greater than or equal to 30 mm Hg or a 5-minute postexercise measurement greater than or equal to 20 mm Hg is considered abnormal and diagnostic of CECS.
The exercise performed at the time of testing must be intense enough to reproduce the patient’s symptoms; otherwise, the postexercise pressure measurements may result in a false-negative result.
Several methods for measuring compartment pressures have been described in the literature.
These include the slit catheter, wick catheter, needle manometry, digital pressure monitor, microcapillary infusion, and solid-state transducer intracompartmental catheter methods.1, 2, 17, 18, 25, 31
The Stryker Intra-Compartmental Pressure Monitor (Kalamazoo, MI) is a handheld digital monitor that can be used to check multiple compartments. It can be used either with a side port needle or an indwelling slit catheter to obtain serial measurements in a single compartment.
A new handheld digital device recently developed by Synthes (Paoli, PA) also allows placement of indwelling catheters and may be useful for obtaining serial measurements.
Near-infrared spectroscopy has been used to determine tissue oxygen saturation.32 This may be a noninvasive, painless alternative to intracompartmental pressures in the diagnosis of CECS but is not currently standardized or readily available.
The vibration test consists of placing a vibrating tuning fork over bone at the area of suspected stress; an elicitation of pain is consistent with a stress fracture.
Pain when performing resisted ankle dorsiflexion and inversion is consistent with tibialis posterior tendinitis or posteromedial periostitis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
When pressure measurements are not consistent with CECS, further diagnostic studies may be necessary to explore the differential diagnosis.
Plain radiographs may demonstrate a periosteal reaction in patients with tibial stress fractures or posteromedial tibial periostitis.
Bone scan will show increased uptake, and MRI may show edema or a black line at the site of a stress fracture.
Ultrasound may play a role in diagnosis by identifying anterior compartment thickness.22
Tingling, numbness, or a positive Tinel sign at a specific location may warrant an electromyogram (EMG) and nerve conduction velocity (NCV) studies to evaluate for peripheral nerve entrapment.
Pain and coolness with paradoxical claudication may warrant an angiogram to evaluate for popliteal artery entrapment.
DIFFERENTIAL DIAGNOSIS
Tibial stress fractures
Posteromedial tibial periostitis
Tenosynovitis of posterior tibialis or ankle dorsiflexors
Peripheral nerve entrapment
Radiculopathy secondary to lumbar pathology
Complex regional pain syndrome
Peripheral vascular disease
Popliteal artery entrapment syndrome
Deep venous thrombosis
NONOPERATIVE MANAGEMENT
Nonoperative management usually requires activity limitation or cessation.
Adjuncts to activity modification include anti-inflammatory medications, stretching, and foot orthotics.
Symptoms usually return with resumption of prior activity level. Surgery, therefore, is indicated in patients who cannot tolerate activity restriction.
SURGICAL MANAGEMENT
Surgical treatment involves fasciotomy of the affected compartments, sometimes with partial fasciectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree