Cervical Pseudarthrosis
Rick B. Delamarter
Ben B. Pradhan
Vikas V. Patel
OVERVIEW
This chapter reviews the prevention, recognition, and treatment of cervical pseudarthrosis. Both prevention and treatment of pseudarthrosis have evolved considerably over the past 10 to 20 years with many options for bone grafts, osteoinductive agents, and fixation methods.
INCIDENCE OF COMPLICATION
First described by Smith and Robinson (1) and later modified by Cloward (2), anterior cervical discectomy with fusion has become a widely accepted and highly successful technique for treatment of disc herniation and spondylolysis (3). Many variations in technique currently exist, including discectomy with or without fusion, and fusion with or without use of plate fixation. A variety of graft options also include autograft, allograft, and cages (possibly with biologics such as demineralized bone matrix and bone morphogenetic protein). There has subsequently been a wide range in the reported incidence of pseudarthrosis after such procedures, ranging from 0% to nearly 50% (4,5,6,7,8,9,10).
Treatment of clinically symptomatic pseudarthrosis yields a high rate of good to excellent results when fusion is achieved, as shown by Brodsky et al., in 21 of 29 patients who achieved fusion (11) and by Farey et al. in 18 of 19 revision surgery patients who also achieved fusion (12). Similarly, 9 of 13 patients in Newman’s series and 9 of 13 patients that fused in a study by Tribus et al. had good to excellent results after revision surgery (13). Thus, the goal of treatment should be to achieve fusion, and pseudarthrosis, when clinically symptomatic, can be effectively treated with surgical intervention.
RELEVANT ANATOMY RELATED TO SITE COMPLICATION
Revision surgery for pseudarthrosis with the goal of achieving fusion can be approached anteriorly, posteriorly, or both anteriorly and posteriorly.
Anterior Approach
In planning the revision anterior approach, the surgeon must consider whether to utilize a new incision on the contralateral side; this minimizes the difficulty of dissection through scar tissue. However, if there is any history of recurrent laryngeal or superior laryngeal nerve compromise, the previous incision/side should be used to prevent bilateral nerve injury.
As in any standard anterior approach, the major structures (in addition to the above-mentioned laryngeal nerves) include the trachea, esophagus, and the structures of the carotid sheath (carotid artery, internal jugular vein, and vagus nerve). Dissection too far laterally on the vertebral body can also put the vertebral arteries at risk, while dissection superficial to the longus coli can risk damage to the sympathetic trunk and stellate ganglia. This nerve injury may lead to Horner’s syndrome (14,15).
HOW TO PREVENT COMPLICATIONS
Patient Factors
Minimizing the risk of pseudarthrosis includes both patient factors and surgical factors. Optimizing patient health with close medical management of diabetes and abstaining from smoking are two important systemic factors. Patient compliance
in limiting postoperative activity and wearing a cervical collar may also help to achieve fusion in the shortest time. Unfortunately, these cannot always be controlled (16).
in limiting postoperative activity and wearing a cervical collar may also help to achieve fusion in the shortest time. Unfortunately, these cannot always be controlled (16).
Discectomy and End Plate Preparation
Meticulous surgical technique is the most important procedural component to reducing the risk of pseudarthrosis. The uncovertebral joints may indicate the lateral extent of discectomy. It is important to completely remove all of the disc material to the posterior longitudinal ligament (PLL). The PLL may or may not be removed depending on whether it is part of the compressive pathology. End plates should then be prepared by removing enough cortical bone to yield a flat, bleeding, bony surface. Without this vascularity, bony ingrowth, and thus fusion, will be limited.
Bone Graft Selection
Interbody graft selection has evolved from the gold standard of structural iliac crest bone to various alternatives including allograft bone, metal cages, absorbable cages, osteogenic biomaterials, and combinations of these. A number of studies have been published purporting equivalent results with autograft when allograft or cages are used in combination with plate fixation (17,18,19,20,21,22,23), while iliac crest bone graft harvest is known to have a significant level of morbidity (24).
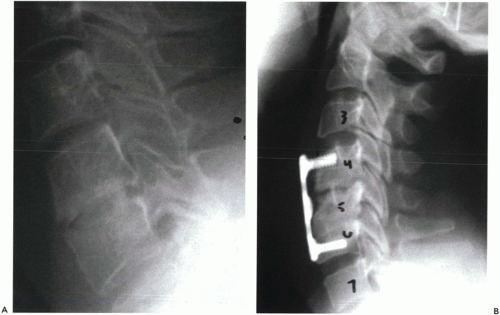 Figure 7.1 A. Note the radiolucent line in the intervertebral space at C4-C5 across which a fusion had been attempted. B. Note the radiolucent halo around the superior screws and anterior displacement of this cervical plate construct in addition to the lucency at C4-C5. These radiographic findings are indicative of pseudarthrosis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





