Key points
- •
Symptoms include numbness, tingling, and/or pain in the ventral-lateral hand, possibly thenar atrophy and weakness, which typically worsens at night.
- •
Positive provocative testing includes Tinel, Phalen, and carpal compression.
- •
Positive electrical testing includes nerve conduction studies revealing initially prolonged median peak sensory latencies (slowing across the wrist), with normal ulnar and radial latencies.
- •
Ultrasound imaging reveals median nerve enlargement at the proximal wrist, median nerve compression during stress testing, and muscle intrusion during hand motion (digit flexion or extension) that compresses the median nerve.
Introduction
Carpal tunnel syndrome (CTS) is a very common nerve compression syndrome, generally not considered difficult to diagnose. However, the method of diagnosis may vary among clinicians. Although diagnosis is important, determination of the degree or severity is useful because it may influence the treatment approach. For example, during the early stages and milder forms of CTS, there may be ample time to begin a trial of conservative treatment without risk of significant denervation. However, in more advanced cases with axon loss, delayed interventional treatment increases the risk of irreversible progressive median nerve (MN) injury. In addition, neuromuscular ultrasound (NMUS) can demonstrate contributing factors that often injure the MN, and once identified, these factors can be addressed in the treatment plan for improved outcomes.
Definition
CTS refers to a constellation or aggregate of hand symptoms that are linked to the median neuropathy at the wrist. There are many various causes, some beyond the scope of this article; however, it is usually considered to be multifactorial :
- •
Increased intracarpal pressure
- •
Decreased MN mobility (from fibrous fixation)
- •
Median nerve deformation (ie, compression, stretching, traction)
- •
Increased stiffness of the synovium and flexor retinaculum (ie, transverse carpal ligament [TCL])
- •
Relative thenar muscle hypertrophy or increased thenar muscle mass with intrusion into the carpal tunnel
- •
Flexor tendon thickening and tightening during activity
Symptom Criteria
The following are typical symptoms that accompany CTS. It is important to keep in mind that these symptoms may be quite variable, thus requiring clinical examination and electrodiagnostic (EDX) testing to confirm.
- •
Numbness: thumb and first 2 to 3 fingers (and lateral aspect of the fourth digit), primarily ventral
- •
Tingling: same distribution as numbness
- •
Weakness: thumb abduction and opposition (dropping or problems holding objects)
- •
Pain: ventral wrist and hand
- •
Autonomic features (temperature or color changes, dry skin, swelling)
- •
Provocative factors: nocturnal worsening; aggravated by sustained wrist flexion or extension, repetitive hand activity
Introduction
Carpal tunnel syndrome (CTS) is a very common nerve compression syndrome, generally not considered difficult to diagnose. However, the method of diagnosis may vary among clinicians. Although diagnosis is important, determination of the degree or severity is useful because it may influence the treatment approach. For example, during the early stages and milder forms of CTS, there may be ample time to begin a trial of conservative treatment without risk of significant denervation. However, in more advanced cases with axon loss, delayed interventional treatment increases the risk of irreversible progressive median nerve (MN) injury. In addition, neuromuscular ultrasound (NMUS) can demonstrate contributing factors that often injure the MN, and once identified, these factors can be addressed in the treatment plan for improved outcomes.
Definition
CTS refers to a constellation or aggregate of hand symptoms that are linked to the median neuropathy at the wrist. There are many various causes, some beyond the scope of this article; however, it is usually considered to be multifactorial :
- •
Increased intracarpal pressure
- •
Decreased MN mobility (from fibrous fixation)
- •
Median nerve deformation (ie, compression, stretching, traction)
- •
Increased stiffness of the synovium and flexor retinaculum (ie, transverse carpal ligament [TCL])
- •
Relative thenar muscle hypertrophy or increased thenar muscle mass with intrusion into the carpal tunnel
- •
Flexor tendon thickening and tightening during activity
Symptom Criteria
The following are typical symptoms that accompany CTS. It is important to keep in mind that these symptoms may be quite variable, thus requiring clinical examination and electrodiagnostic (EDX) testing to confirm.
- •
Numbness: thumb and first 2 to 3 fingers (and lateral aspect of the fourth digit), primarily ventral
- •
Tingling: same distribution as numbness
- •
Weakness: thumb abduction and opposition (dropping or problems holding objects)
- •
Pain: ventral wrist and hand
- •
Autonomic features (temperature or color changes, dry skin, swelling)
- •
Provocative factors: nocturnal worsening; aggravated by sustained wrist flexion or extension, repetitive hand activity
Clinical findings
Physical Examination
Sensory examination is often normal in CTS, despite patient complaints and other diagnostic findings. The pattern of sensory loss may not follow the classic MN distribution in the hand (which includes the ventral thumb, index, middle, and lateral half of the ring finger) due to anatomic variations. Examination for pin sensation is quite subjective, but monofilament testing adds some degree of objectivity and can be used to map out sensory loss within the MN distribution. Abnormal 2-point discrimination (and vibratory loss) is a later manifestation due to more severe nerve injury.
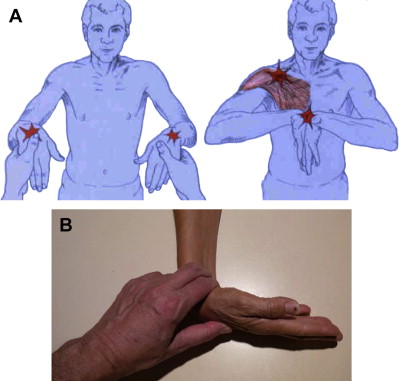
Positive provocative Tinel and Phalen ( Fig. 1 ) tests are not considered reliable or confirmatory, but may be helpful by adding to the clinical impression. The problem is that they are not objective tests, and the precise method of application is highly variable among clinicians. Fig. 1 A illustrates the proper and commonly used improper method of performing the Phalen test. Carpal compression may also be useful and can be applied simultaneously with the Phalen test as the operator grasps the patient’s wrist and maintains flexion dorsally while providing focal pressure over the MN ventrally (see Fig. 1 B).
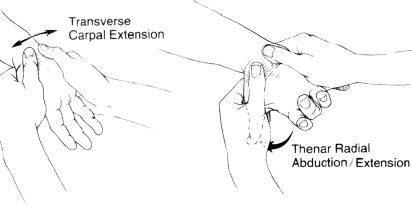
Palpation of the wrist for mechanical restriction over the carpal canal can assist in diagnosis and has been demonstrated to have a sensitivity of greater than 90%, using EDX as the gold standard. The most reliable motion testing involves transverse extension and thenar extension/abduction ( Fig. 2 ). Palpatory diagnosis also correlates well with EDX.
Strength testing can identify thenar muscle weakness if applied correctly—the examiner being aware that resistance must be applied along the first metacarpal or at the number 1 metacarpal-phalangeal joint, and toward the radial side of the index to avoid testing the radial innervated abductor pollicis longus ( Fig. 3 ). The median innervated thumb muscles should never be tested by pulling a digit through the patient’s flexed index and thumb, because that tests the thumb adductor and long thumb and finger flexors, which receive ulnar innervation for the former, while the flexor pollicis longus and index finger flexors receive their median innervation proximal to the tunnel. It is also important to exclude contribution from the abductor pollicis longus, which would not be affected by CTS either, because it is radial nerve innervated. It may seem that the patient has normal strength if the distal abductor pollicis brevis and opponens pollicis muscles are not properly isolated and challenged.

One sign that may be apparent with advanced MN injury is the observation of thenar atrophy. Indentation or hollowing of the thenar mound is a late sign accompanying weakness and implies severe CTS. In fact, some authors have determined that it may be too late to operate once the nerve damage has reached this state. Bland discovered that patients with absent sensory or motor responses (degeneration of many MN fibers) had the worst outcomes.
Differential Diagnosis
Neuromusculoskeletal and vascular differential diagnoses of carpal tunnel symptoms include, but are not limited to: brain, cervical spine, musculoskeletal system, and neurologic diseases other than CTS ( Box 1 ). It may be helpful to consider the history and physical examination in any attempt to clarify the perspective from central to distal. There are many predisposing factors including, but not limited to: alcoholism, endocrine diseases (diabetes and thyroid), rheumatologic disease, amyloidosis, trauma, infections, uremia, and obesity.
Brain
Cerebral insult (including tumors, thalamic lesions, lacunar strokes)
Demyelinating diseases
Cervical spine
Cervical disc disease, spondylosis, stenosis, and associated radiculopathy
Spinal cord injury (including syringomyelia, tumors)
Musculoskeletal (peripheral)
Myofascial pain syndrome
Osteoarthritis, inflammatory arthropathies (including Raynaud’s)
Tendonitis, tendinosis, epicondylitis
Compartment syndrome
Ganglions and hand tumors
Neurologic
Brachial plexopathy (including Parsonage Turner syndrome and thoracic outlet syndrome)
Complex regional pain syndrome
Compression neuropathy proximal to the wrist
Ischemic monomelic neuropathy
Polyneuropathy (including diabetic, mononeuropathy multiplex)
Motor neuron disease
Demyelinating diseases
Infections (Lyme disease, tabes dorsalis, leprosy)
Objective Diagnostic Studies
Diagnostic studies that produce measurable changes to document nerve injury help confirm the diagnosis of CTS. The most commonly used tests include EDX and NMUS. Quantitative sensory testing will not be discussed here.
Electrodiagnosis
The electrodiagnostic approach to CTS is not simply looking at latencies and other waveform parameters. It includes the use of this information while taking into account the clinical acumen to decide
- •
If there are electrodiagnostic abnormalities, are they meaningful and do they support the clinical impression of CTS, or does one reject the clinical impression based on the electrodiagnostic findings for management purposes?
- •
If there are no electrodiagnostic abnormalities, is the suspected diagnosis of CTS still likely for purposes of treatment strategies?
These queries are 2 ends of the diagnostic spectrum with which the electrodiagnostician must struggle. The area in between poses much less challenge.
The spectrum of peripheral nerve injury includes axon and/or myelin disruption and tends to be simplified because effects are measured rather than underlying pathophysiology. Myelin injury may occur in isolation or with secondary axonal death. Axonal death is also referred to as axonopathy, denervation, and Wallerian degeneration (WD). WD includes both axon death and myelin digestion. CTS typically involves myelin disruption initially, followed by axonal death. Macrophages and Schwann cells clear the myelin debris associated with WD. However, if there is a loss of Schwann cells and other growth-supporting molecules, reinnervation becomes less likely. Muscle wasting is a sign of long-standing WD and heralds a poor prognosis for resolution of the atrophy, regardless of any intervention.
Initially, CTS symptoms are transient because of vascular compromise with resultant ischemia caused by overwork or wrist flexion during sleep. Eventually “symptom-producing conduction block” (sCB) may ensue when there is a loss of myelin of 2 successive internodes between nodes of Ranvier. Depending on how many axons are involved, there will be varying degrees (intensity and frequency) of paresthesias, dyesthesias, and eventually weakness. Recovery of conduction block by remyelination promotes recovery of sensation and strength. The remyelinated segment may conduct slower; however, slowing does not cause weakness. A classic example of slowing unrelated to the presence of clinical symptomology is early Charcot-Marie-Tooth disease. In addition, there may be axons suffering from slowing and others with sCB.
Dysmyelination or Myelinopathy
All types and severities of myelin injury were traditionally referred to as “demyelination,” but this oversimplification implies a lack of myelin, which occurs infrequently. If this were true, symptoms would be constant, and the periodic symptoms associated with activity or nocturnally would not exist. Dysmyelination or myelinopathy and sCB better describe the physiologic states of CTS, as follows :
- 1.
Varying degrees of myelin damage
- a.
Partial thickness (thinning) of internode(s)
- b.
Total thickness of one internode
- c.
Total thickness of internodes but not consecutively
- d.
Total thickness of consecutive internodes (sCB)
- a.
- 2.
Extent of remyelination following myelin injury
- 3.
Extent of remyelination following axonal injury regrowth/reinnervation and sprouting
Patterns of myelin damage may have both electrodiagnostic and clinical manifestations. The thinning of myelin along an axon or loss of myelin at nonconsecutive internodes each cause slowing of conduction that lacks clinical manifestations, whereas the loss of myelin at 2 consecutive internodes would result in sCB. Summation of the axon conducting properties in the MN will express varying degrees of these patterns—slowing with no clinical manifestations, or partial to complete block that manifests in sensory and eventually motor symptoms. Remyelinated segments will conduct slowly due to suboptimal myelin.
Axonopathy
The compound muscle action potential (CMAP) attenuates both proximally and distally if acute injury outpaces reinnervation by axonal regrowth or peripheral sprouting from neighboring axon nerve terminals. The CMAP amplitude may return to normal, but residual slowing (prolonged latencies) is likely from either poorly myelinated (dysmyelinated) regenerating parent axons or sprouts from neighboring axons. These axons will never conduct as fast as the original uncompromised axon. Therefore, denervation may be present, or there could be only minor electrical changes such as mild slowing. When a large amount of motor denervation occurs and exceeds reinnervation, then there is detectable clinical weakness.
In chronic repeated compression, the MN is often thinned and flattened at the site of compression, yet may be enlarged both proximal and distal to the compression. With repeated compression, WD occurs gradually, and over a longer period of time there may be collapse of the endoneurial tubes, thus preventing axonal regrowth (a time-sensitive process). CTS has an advantage compared with other nerve injuries, as the reinnervation distance is relatively short, requiring less time to complete the nerve repair before there is a loss of all supporting molecules.
Technique
Multiple electrophysiologic techniques have been described for use in confirming a diagnosis of CTS. However, there is a lack of consensus as to a single best approach. For a broad description of the various EDXs used to evaluate CTS, the reader is encouraged to review several recent articles. There are also joint organization practice publications that break down recommendations by standards, guidelines, and options.
More focus is usually given to the measurement of sensory fiber conduction because large-diameter myelinated sensory axons are affected before smaller diameter motor axons. Ipsilateral studies should include measurement of sensory and motor conduction in the MN across the wrist, including comparison with nearby nerves (radial and/or ulnar) that do not traverse the carpal tunnel, to minimize the effects of temperature, polyneuropathy, or other factors that may lead to misinterpretation of abnormal MN findings. It is essential to perform sensory conductions from the wrist to the second or third digit, and if there is an abnormality, then from the palm to the digit. Proximal segment conduction attenuation relative to the distal palmar response theoretically will establish if sCB is present, with a significantly larger sensory nerve action potential at the palm than the wrist, suggesting focal compression of the MN at the wrist. However, caution must be exercised using motor comparisons because of volume conduction from ulnar innervated muscles, which might not cause an initial downward deflection due to phase cancellation from the multiple muscles activated by dual stimulation of the median and ulnar nerves.
Motor nerve conduction velocity measured in the forearm is also often slowed. Some attribute this to degeneration of motor fibers proximal to the site of entrapment. However, recording electrodes over the abductor pollicis brevis may pick up slower motor fibers, while faster fibers are blocked at the wrist and not recorded at the end organ. When such slowing is detected between the elbow and the wrist, there is a tendency to attribute it to MN dysfunction at the wrist, but further conduction studies should be considered to demonstrate that the slowed conduction between the wrist and the elbow (mixed conduction) is due to blockage of the fastest conducting fibers:
- •
A lack of conduction with this technique may be due to retrograde degeneration of the MN axons and would mitigate against recovery with decompression of the MN at the wrist.
- •
If there is slowing of conduction between the elbow and the wrist, evaluation of forearm muscles should be done to rule out electrodiagnostic abnormalities proximal to the level of the wrist, which would impact the interpretation of a slowing across the wrist.
Needle electromyography (EMG) can confirm denervation if there is motor involvement. Fibrillations and positive sharp waves identify axonal injury and assist in determining chronicity, but are poor indicators of the degree of denervation. Volitional potential abnormalities can assist chronicity determination. If there is a low CMAP from stimulation at the wrist (with pickup at the abductor pollicis brevis muscle and without a reliable palmar study), the EMG will clarify if this is due to sCB or denervation and whether there is any reinnervation. Needle EMG should also be performed if a radiculopathy is a possible cause of symptoms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







