Carpal Tunnel Syndrome
David Bozentka
Lawrence W. Weber
CLINICAL PRESENTATION
Carpal tunnel syndrome is the most common peripheral compression neuropathy. The symptoms are related to compression of the median nerve at the wrist. Patients will present with complaints of numbness and tingling of the hand. The median nerve sensory distribution includes the thumb and index, long, and radial half of the ring finger. To differentiate from other compression neuropathies, it is helpful to have the patient determine whether the numbness occurs in this distribution. Patients with carpal tunnel syndrome will often note diffuse hand numbness. In the mild to moderate stages of the syndrome, the patient will note that the paresthesias are intermittent. As the neuropathy progresses to the more severe stages, the numbness will become more constant.
Nocturnal symptoms are common. Patients will often complain of awaking and having to shake their hand in an attempt to relieve their symptoms, termed the shake sign. Pain often occurs about the volar aspect of the wrist and can radiate proximally. Occasionally, the symptoms radiate to the shoulder and rarely to the neck region due to carpal tunnel syndrome. The symptoms are aggravated by activities such as talking on the telephone, reading a book, or driving. Patients will complain of dropping objects, having difficulty buttoning buttons, and often noting that they need to carefully watch as they grasp small objects to ensure adequate grip.
The carpal canal is made up of carpal bones, which form a “C”-shaped ring dorsally, and the transverse carpal ligament that lies volarly. The transverse carpal ligament runs across the canal, attaching to the scaphoid and trapezium radially and the pisiform and hook of the hamate ulnarly. The thenar and hypothenar musculature arise from the transverse carpal ligament and insert on the thumb and small finger, respectively. The median nerve and nine flexor tendons run within the canal (Fig. 45-1). In general, compression of the median nerve at the wrist occurs, related to the canal being too small or the contents being too large for the tunnel.
There are multiple etiologic factors that may lead to the development of carpal tunnel syndrome. These factors are classified as anatomic, physiologic, and positional.1 Anatomic factors include anomalous muscles in the canal, distal radius fractures, or a hematoma following an injury in an anticoagulated patient. Physiologic factors are further divided into metabolic, inflammatory, and fluid changes. Metabolic factors leading to the neuropathy may include diabetes mellitus, alcoholic neuropathy, and hypothyroidism. Although carpal tunnel syndrome is rarely seen in children, it is important to note that the most common etiologies are lysosomal storage diseases: mucopolysaccharidoses and mucolipidoses.2 Inflammatory causes include factors such as rheumatoid arthritis, gout, or infection. Fluid changes associated with hemodialysis and pregnancy may also be related. Certain positional changes of the wrist can lead to compression of the median nerve. By holding the wrist in flexion or extension, the size of the carpal canal decreases, thus placing the nerve at risk for a compression neuropathy. Also, repeated use of vibrating hand tools has been linked to carpal tunnel syndrome.3 These etiologic factors should be entertained prior to concluding that the neuropathy is idiopathic.
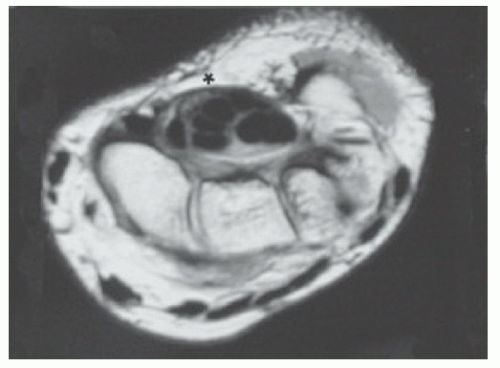 FIGURE 45-1. MRI wrist T1-weighted image axial cut at the level of the carpal canal. The transverse carpal ligament is located just below the asterisk. |
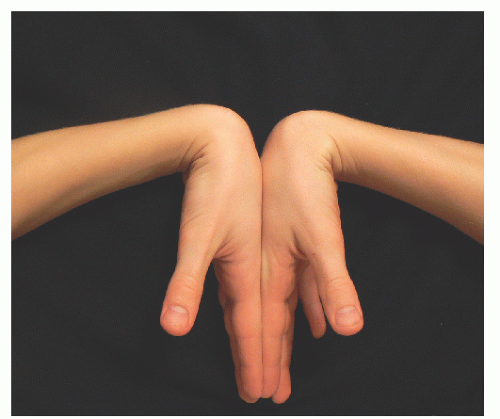
 FIGURE 45-3. The reverse Phalen maneuver is performed by having the patient extend the wrist for 1 minute. |
The differential diagnosis for patients with carpal tunnel syndrome includes sensory motor polyneuropathy, such as in diabetes. Proximal sites of nerve compression can also lead to similar symptoms. A patient with a C6 or C7 radiculopathy will often have numbness in the median nerve distribution. Pronator syndrome, related to median nerve compression in the proximal forearm, will also manifest with similar symptoms and should be ruled out.
CLINICAL POINTS
Presenting symptoms include numbness and tingling of the hand.
Pathology involves compression of the median nerve at the wrist.
Etiology may be anatomic, physiologic, and/or positional.
PHYSICAL FINDINGS
On physical examination, it is important to assess the entire upper extremity including the cervical spine to rule out other potential etiologic factors. An evaluation for carpal tunnel syndrome should include certain provocative maneuvers as well as a thorough motor and sensory evaluation.
Common provocative maneuvers to confirm the diagnosis of a median nerve compression at the wrist include the Phalen maneuver, Tinel sign, and carpal canal compression test.4,5 These tests are considered positive if the symptoms develop in the median nerve distribution. The Phalen maneuver is performed by placing the patient’s wrist in full flexion for 1 minute (Fig. 45-2). The reverse Phalen maneuver involves placing the patient’s wrists in extension (Fig. 45-3). The time at which symptoms develop and the anatomic distribution of the paresthesias during the maneuvers are documented. The Tinel sign is performed by percussing over the median nerve at the wrist (Fig. 45-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree