Carpal Fractures
Scaphoid
General Information
The scaphoid is the most commonly fractured carpal bone. This fracture occurs most frequently in young adult men, but may be seen in elderly persons and patients as young as 12.
Diagnostic Criteria
The criteria for diagnosis of a scaphoid fracture include an appropriate history, clinical suspicion, and objective documentation (x-rays or other imaging modality) of the fracture. The consequences of undertreatment of a scaphoid fracture and over immobilization of a wrist sprain make it essential to conclusively determine that a scaphoid fracture either does or does not exist. The determination that a fracture is not present may be accomplished either by clinical examination (no tenderness in the snuffbox or over the distal pole of scaphoid) or imaging modalities (a negative plain x-ray is not conclusive). Failure to diagnosis a scaphoid fracture may lead to the development of nonunion and wrist arthritis. Other traumatic conditions producing wrist pain similar to that produced by a scaphoid fracture include distal radius fracture, fracture of another carpal bone, ligamentous injury to the wrist, and wrist sprain. A patient with a long-standing nonunion (who may be unable to recall any prior significant trauma to the wrist) may present with a more recent injury, which may lead to the incorrect conclusion that the fracture seen on x-rays is an acute injury.
History
Typically, a scaphoid fracture occurs as a result of a forceful extension of the wrist. Most commonly, this occurs as a result of a fall, motor vehicle accident, or sporting event mishap. The patient complains of pain on the radial aspect of the wrist, limited mobility, and some degree of swelling. It is not unusual for the patient
to present for evaluation days and sometimes weeks after the injury. The patient may attribute his or her symptoms to a sprain or less severe injury to the wrist.
to present for evaluation days and sometimes weeks after the injury. The patient may attribute his or her symptoms to a sprain or less severe injury to the wrist.
Physical Examination
Clinical examination should include observation for areas of swelling (commonly noted on the dorsal/radial aspect of the carpus) and ecchymosis (more commonly noted volarly). Palpation should include all areas of the wrist, including the distal radius and ulna, the anatomic snuffbox, the individual carpal bones, as well as the carpal metacarpal joints. Tenderness to palpation of the anatomic snuffbox or over the distal pole of the scaphoid should make a fracture of the scaphoid a diagnostic consideration. Wrist motion is usually reduced, but if there has been a delay between the injury and time of presentation, motion may be good.
Radiographic Assessment
Standard anterior posterior (AP) and lateral x-rays of the injured wrist should be obtained. In addition, a scaphoid view or an ulnarly deviated AP view is extremely helpful in producing a longitudinal view of the scaphoid and may help define a subtle, nondisplaced fracture. Fractures of the scaphoid may be seen in the proximal, middle, or distal third of the bone (Fig. 1). They may be described as nondisplaced, displaced, angulated, malrotated, and/or comminuted. The plain x-rays also should be inspected for evidence of degenerative changes secondary to a chronic nonunion (beaking of the radial styloid or narrowing of the radio-scaphoid joint space distal to the nonunion site) (Fig. 2).
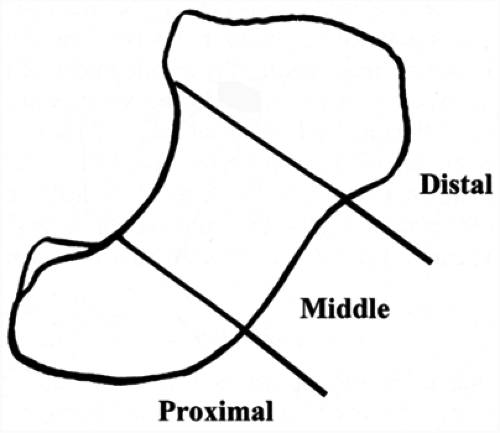 FIG. 1. Fractures of the scaphoid are classified as involving the proximal, middle (waist), or distal third (including scaphoid tubercle). |
Commonly, an acute fracture may not be seen on initial films. Repeat films taken in 10 to 14 days may subsequently reveal a fracture as a result of slight resorption of bone around the fracture site. If clinical suspicion suggests that a fracture still may be present in spite of negative delayed x-rays, further imaging studies are indicated. A bone scan, computed tomography (CT) scan, and magnetic resonance imaging (MRI) have all been reported to have a high level of sensitivity for detecting occult scaphoid fractures.
Treatment
The patient should be immobilized in a thumb spica splint if he or she presents with an acute injury and is clinically suspected to have a scaphoid fracture but no fracture is identified on x-rays. The patient should be discouraged from using the hand for any heavy activities.
Once the diagnosis of scaphoid fracture is made, treatment is dictated by the location of the fracture within the scaphoid as well as the degree of displacement of the fracture.
Fractures of the Middle Third (Waist)
Nondisplaced fractures of the waist of the scaphoid are the most common type of scaphoid fracture and should be immobilized in a thumb spica cast until radiographic evidence of healing is present. This typically takes between 9 and 12 weeks; however, it may take 16 weeks or longer. There is some evidence that the rate of union is slightly higher if a long arm thumb spica cast is used initially. The time to union also may be slightly shorter if a long-arm cast is used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









