Abstract
The agitation crisis in the awakening phase after traumatic brain injury (TBI) is one of the most difficult behavioral disorders to alleviate. Current treatment options are heterogeneous and may involve excessive sedation. Practice guidelines are required by professionals in charge of TBI patients. Few reviews were published but those are old and based on expert opinions. The purpose of this work is to propose evidence-based guidelines to treat the agitation crisis.
Methods
The elaboration of these guidelines followed the procedure validated by the French health authority for good practice recommendations, close to the Prisma statement. Guidelines were elaborated on the basis of a systematic and critical review of the literature.
Results
Twenty-eight articles concerning 376 patients were analyzed. Recommendations are: when faced with an agitation crisis, the management strategy implies to search for an underlying factor that should be treated such as pain, acute sepsis, and drug adverse effect (expert opinion). Physical restraints should be discarded when possible (expert opinion). Neuroleptic agent with a marketing authorization can be used in order to obtain a quick sedation so as to protect the patient from himself, closed ones or the healthcare team but the duration should be as short as possible (expert opinion). The efficacy of beta-blockers and antiepileptics with mood regulation effects like carbamazepine and valproate yield the most compelling evidence and should be preferably used when a background regimen is envisioned (grade B for beta-blocker and C for antiepileptics). Neuroleptics, antidepressants, benzodiazepines, buspirone may be prescribed but are considered second-line treatments (expert opinion).
Conclusion
This study provides a strategy for treating the agitation crisis based on scientific data and expert opinion. The level of evidence remains low and published data are often old. New studies are essential to validate results from previous studies and test new drugs and non-pharmaceutical therapies.
1
Introduction
Agitation crisis is one of the hallmark symptoms of traumatic brain injury due to the difficult care management and impact on caregivers and closed ones. Even if agitation is not specific to TBI, it is a very common complication after awakening because of amnesia and attention disorders. The patient often has a hard time understanding the situation and can be quite anxious. According to the different studies, an agitation episode occurs in 11% to 70% of patients with severe TBI (see Stephan et al., in this issue ). This important variability can be explained by the heterogeneity of the population (previous personality pre-TBI, history of drug abuse, localization of the brain damage), the definition of agitation and scales used. The duration of agitation varies from a few days to several weeks. Several external factors can trigger anxiety and heighten the agitation: pain, contention, excessive stimulations, an aggressive attitude from closed ones or even healthcare professionals and psychotropic drugs .
Uncoordinated motor agitation is typical of the awakening period: motor agitation, projection against bed rails, the patient gets up from the bed and sits back down continuously. At a more advanced stage, more evolved behaviors may be observed: compulsive and “finalized” agitation (e.g. taking the bed or chairs apart, trying to remove constraints, destroying or dismantling the equipment in the room like the toilet, bathroom, electrical system), these behaviors can be associated with running away, non-stop calls, screams. This elaborated motor activity can be extremely overwhelming. Sexual disinhibition is also typical of this stage. Sometimes observed as verbal, even physical, violent uncontrolled aggressive behaviors. These periods of great agitation often alternate with periods of sleepiness and inversion of the nycthemeral rhythm.
Agitation-related risks are major ones and require the implementation of appropriate measures. Falls, self-inflicted harm, friction and burns (from certain types of contentions), “domestic” risks (e.g. destroying hospital equipment in the room), aggressive feedback from the healthcare team and closed ones are classical risks for the patient. There are also risks for healthcare professionals, physical violence (“voluntary” or not) and above all, physical and mental burnout, which can lead to outbursts and escalating to violence.
Overmedication with excessive sedation and its consequences (swallowing disorders, paradoxical agitation) goes against the overall rehabilitation project for the patient and is in fact a very commonly observed consequence when teams have not been properly trained for TBI management or when there is not enough personnel to care for the patients.
Non-pharmaceutical care management is often brought up but has rarely been described . The heterogeneity of practices regarding medication care of agitation and aggressiveness also justifies a better knowledge of the latest scientific data. In that line, according to a survey conducted on US healthcare professionals , the 5 medicines most frequently used for expert physicians to treat agitation in patients with TBI are carbamazepine, tricyclic antidepressants, trazodone, amantadine and beta-blockers. For the non-expert group, those were carbamazepine, beta-blockers, haloperidol, tricyclic antidepressants and benzodiazepines. A more recent and similar work by Francisco et al. showed that experts preferentially used valproate, lorazepam, propranolol, nadolol, trazadone and carbamazepine whereas non-experts used in priority lorazepam, carbamazepine and risperidone. This study also pointed out no clear consensus for medication management of agitation with noticeable differences between experts and non-experts.
In this context, one of the questions selected by the steering group concerned the implementation of pharmaceutical and non-pharmaceutical management of agitation and aggressiveness in patients with severe TBI.
Several reviews of the literatures have been published , yet most of them are dated, some only focused on pharmaceutical treatments , were not specifically targeted to TBI patients , did not specifically evaluate behavioral disorders or did not take into account the level of scientific evidence .
The objective of this work was to conduct a critical review of the literature, confronted to experts’ opinions, in order to propose practice guidelines according to evidence-based medicine criteria regarding the treatment of agitation and aggressiveness.
2
Methods
The literature review was performed on Medline, in French and English from January 1990 to March 2012 (research done by the services of the French Health Authority (HAS) according to the practice guidelines protocol). An additional research was performed up to June 2015 without the help of the French Health Authority. Finally, researches were conducted on books and articles not referenced in this database. The Medline search was based on a combination of the following keywords: “Brain Injuries, craniocerebral Trauma, Brain trauma*, Head injur*, Head trauma*, Crisis, Complementary Therapies, Behavior Therapy, Cognitive Therapy, Feedback, Holistic Nursing, Psychoanalysis, Psychotherapy, Family Therapy, psychological treatment, psychological therap*, behaviour management, psychotherapy, family intervention, music therapy, Critical Care, Drug Therapy, Central Nervous System Stimulants, Methylphenidate, Dopamine Agents, Dopamine, Amantadine, Dopamine Agonists, Bromocriptine, Levodopa, Antidepressive Agents, Sertraline, Fluoxetine, Paroxetine, Citalopram, tianeptine, Trazodone, Amitriptyline, Clomipramine, Trimipramine, Mianserin, mirtazapine, milnacipran, duloxetine, Iproniazid, venlafaxine, Cholinesterase Inhibitors, Physostigmine, donepezil, rivastigmine, Adrenergic beta-Antagonists, Propranolol, Haloperidol, Methotrimeprazine, Clozapine, quetiapine, ziprasidone, Anticonvulsants, Valproic Acid, Carbamazepine, lamotrigine, Lithium, zolpidem, modafinil, Brain Injuries/drug therapy”.
When the objective of an article was the evaluation of a therapeutic strategy for the agitation or aggressive crisis in adult patients with TBI, it was systematically analyzed. Time since TBI was more specifically studied since the agitation crisis occurs preferentially during the post-traumatic amnesia stage. Similarly, the time course of drug effects is an important criterion to consider in the management of the crisis. Articles that had a more general objective to evaluate the effects of a treatment for agitation or aggressiveness in patients with TBI were also considered.
Were included in this review of the literature: open studies without a control group, case series and clinical cases. Results of the articles selected were classified according to evidence-based medicine criteria (see Table 1 for level of evidence and recommendations grade). Furthermore, potential biases were taken into account: heterogeneity of the population, inclusion delay, multiple treatments, use of adapted and specific scales, and compatibility with the marketing authorizations in France.
| Evidence level | Types of interventional studies | Grades of recommendation |
|---|---|---|
| 1 | High power randomized controlled trials (RCT) Meta-analysis of RCT | Grade A Established scientific evidence |
| 2 | Low-power RCT Non-randomized comparative studies Cohort studies | Grade B Scientific presumption |
| 3 | Case-control studies | Grade C Low level of evidence |
| 4 | Comparative studies with considerable bias Retrospective studies Case series |
Based on the data from the literature, recommendations were made by a group of professional (9 PM&R physicians, 4 psychiatrists, 3 psychologists, 1 primary care physician, 1 physical education professor, 1 social worker, 1 lawyer, 1 director of a medicosocial structure) and 2 persons representing the families of patients with TBI. Then, these guidelines were read and criticized by a reading group also made of professionals (10 PM&R physicians, 7 psychologists, 2 head registered nurses, 1 psychiatrists, 1 neurologist, 1 primary care physicians, 1 prison physician, 1 physical education professor, 1 social worker, 1 physiotherapist, 1 occupational therapists, 1 lawyer, 1 magistrate, 1 director of a medicosocial structure and 1 insurance representative) and 2 persons representing the families of patients with TBI (see the introductory article of Luauté and Mathé, in this issue ). This good practice recommendation received the label from the French High Authority for Health, meaning that these guidelines were established according to the methodological guidelines and procedures recommended by HAS ( http://www.has-sante.fr/portail/jcms/c_431294/recommandations-pour-la-pratique-clinique-rpc ; the website of the French High Authority for Health [HAS] gives access to documents in English). The protocol lists several criteria (criteria 1, 2, 3, 5, 6, 7, 9, 13, 15) of the PRISMA method .
2
Methods
The literature review was performed on Medline, in French and English from January 1990 to March 2012 (research done by the services of the French Health Authority (HAS) according to the practice guidelines protocol). An additional research was performed up to June 2015 without the help of the French Health Authority. Finally, researches were conducted on books and articles not referenced in this database. The Medline search was based on a combination of the following keywords: “Brain Injuries, craniocerebral Trauma, Brain trauma*, Head injur*, Head trauma*, Crisis, Complementary Therapies, Behavior Therapy, Cognitive Therapy, Feedback, Holistic Nursing, Psychoanalysis, Psychotherapy, Family Therapy, psychological treatment, psychological therap*, behaviour management, psychotherapy, family intervention, music therapy, Critical Care, Drug Therapy, Central Nervous System Stimulants, Methylphenidate, Dopamine Agents, Dopamine, Amantadine, Dopamine Agonists, Bromocriptine, Levodopa, Antidepressive Agents, Sertraline, Fluoxetine, Paroxetine, Citalopram, tianeptine, Trazodone, Amitriptyline, Clomipramine, Trimipramine, Mianserin, mirtazapine, milnacipran, duloxetine, Iproniazid, venlafaxine, Cholinesterase Inhibitors, Physostigmine, donepezil, rivastigmine, Adrenergic beta-Antagonists, Propranolol, Haloperidol, Methotrimeprazine, Clozapine, quetiapine, ziprasidone, Anticonvulsants, Valproic Acid, Carbamazepine, lamotrigine, Lithium, zolpidem, modafinil, Brain Injuries/drug therapy”.
When the objective of an article was the evaluation of a therapeutic strategy for the agitation or aggressive crisis in adult patients with TBI, it was systematically analyzed. Time since TBI was more specifically studied since the agitation crisis occurs preferentially during the post-traumatic amnesia stage. Similarly, the time course of drug effects is an important criterion to consider in the management of the crisis. Articles that had a more general objective to evaluate the effects of a treatment for agitation or aggressiveness in patients with TBI were also considered.
Were included in this review of the literature: open studies without a control group, case series and clinical cases. Results of the articles selected were classified according to evidence-based medicine criteria (see Table 1 for level of evidence and recommendations grade). Furthermore, potential biases were taken into account: heterogeneity of the population, inclusion delay, multiple treatments, use of adapted and specific scales, and compatibility with the marketing authorizations in France.
| Evidence level | Types of interventional studies | Grades of recommendation |
|---|---|---|
| 1 | High power randomized controlled trials (RCT) Meta-analysis of RCT | Grade A Established scientific evidence |
| 2 | Low-power RCT Non-randomized comparative studies Cohort studies | Grade B Scientific presumption |
| 3 | Case-control studies | Grade C Low level of evidence |
| 4 | Comparative studies with considerable bias Retrospective studies Case series |
Based on the data from the literature, recommendations were made by a group of professional (9 PM&R physicians, 4 psychiatrists, 3 psychologists, 1 primary care physician, 1 physical education professor, 1 social worker, 1 lawyer, 1 director of a medicosocial structure) and 2 persons representing the families of patients with TBI. Then, these guidelines were read and criticized by a reading group also made of professionals (10 PM&R physicians, 7 psychologists, 2 head registered nurses, 1 psychiatrists, 1 neurologist, 1 primary care physicians, 1 prison physician, 1 physical education professor, 1 social worker, 1 physiotherapist, 1 occupational therapists, 1 lawyer, 1 magistrate, 1 director of a medicosocial structure and 1 insurance representative) and 2 persons representing the families of patients with TBI (see the introductory article of Luauté and Mathé, in this issue ). This good practice recommendation received the label from the French High Authority for Health, meaning that these guidelines were established according to the methodological guidelines and procedures recommended by HAS ( http://www.has-sante.fr/portail/jcms/c_431294/recommandations-pour-la-pratique-clinique-rpc ; the website of the French High Authority for Health [HAS] gives access to documents in English). The protocol lists several criteria (criteria 1, 2, 3, 5, 6, 7, 9, 13, 15) of the PRISMA method .
3
Results
3.1
Non-pharmacological measures
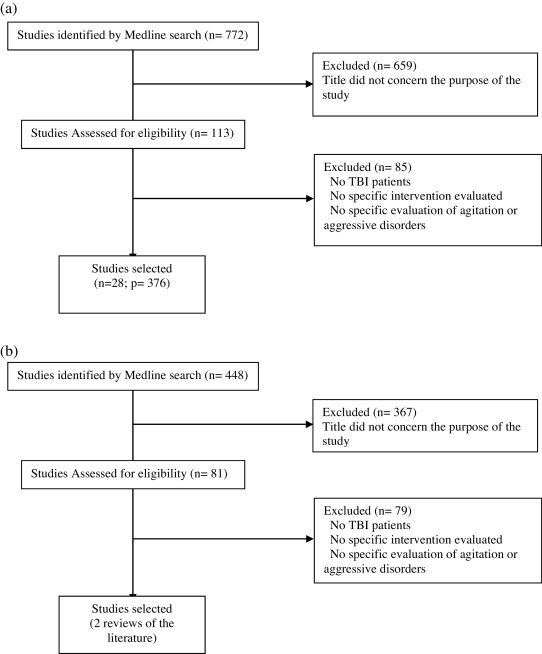
No experimental study has been found regarding the study of non-pharmacological therapeutic intervention for the agitation or aggressiveness crisis from the 448 articles identified by the literature research and the 81 articles analyzed (see Wiart et al., in this issue ) ( Fig. 1 ).
Guidelines are proposed essentially based on two synthetic literature reviews and the opinion of experts from the working group.
For the agitation crisis, it is recommended to look for and treat the pain and its causes (undetected fracture), look for iatrogenic effects of medications, limit contentions as much as possible and when necessary, they must be medically prescribed and regularly reassessed by a trained team. Expert opinion.
It is recommended to discard all non-essential physical constraints (question the relevance of intravenous perfusion, urinary catheterization, nasograstric intubation); making sure that the patients’ environment is peaceful, reassuring, so patients can start finding their marks. Fatigue should be taken into account with implementation of resting periods. It is also relevant to ensure a physical presence; adapt the bedroom to avoid risk of falls, equip the bed with security rails, put foam at the bottom of the bed, eventually set the bed on the floor under certain circumstances (when the patient has no tracheotomy, nasogastric tube, traction, contentions, etc). Prevent wanderings and pathological walking behaviors are sometimes necessary and require the use of specific devices such as alert systems, shoulder-length door with exterior opening allowing medical supervision, electronic bracelet, video monitoring… Ensuring the management of anxiety and reassuring the patients is an important issue but need to have enough trained healthcare personnel. Some specific training programs have been developed such as the Non-Violent Crisis Intervention – Expert Opinion.
It is recommended to involve family members who must be informed on behavioral disorders and on the way to react in order to avoid an escalation of violence and aggressiveness, how to adopt a calming attitude. The attitude of caregivers and healthcare professionals faced with these disorders can play a precipitating, reducing or aggravating role according to their level of knowledge on the pathology and their training, their ability to anticipate patients’ needs, capacity for empathy as well as adapting to patients’ symptoms (i.e. personal care, perceived as stressful, comprehension difficulties…) – Expert opinion.
It is recommended to try and restore a proper sleep-wake pattern – Expert opinion.
Post-intensive care unit (ICU) department or coma awakening rehabilitation department are more adapted to this type of care management. Training and personnel supervision are recommended – Expert opinion.
The consultation by a psychiatrist must be possible and obtained quickly. A hospitalization in a specialized psychiatric unit can sometimes shed another light and contribute to improving behavioral disorders in some patients in situation of therapeutic failure – Expert opinion.
3.2
Pharmacological interventions
The review of the literature yielded 666 experimental articles (see Plantier et al., in this issue ). More specifically, regarding the care management of agitation and/or aggressiveness, 28 articles concerning 376 patients were analyzed.
For each therapeutic class, the justification of using the molecule is briefly covered (most of these drugs do not have a market authorization in France in this indication), then the results of the most relevant studies are described. Lastly, the general guidelines established by the SOFMER expert group are presented.
3.2.1
Beta-blockers
For agitation management, the mechanism of action of beta-blockers is not clear. One of the reasons brought up in the rationale for using beta-blockers is the reduced adrenergic activity at central or peripheral level . The appeasing effect of beta-blockers in stress-inducing situations is also very well-known .
The efficacy of beta-blockers in agitation and aggressiveness after TBI is based mostly on four controlled studies vs. placebo that used either propranolol or pindolol . These are older studies with small samples: 21 patients , 10 patients , 11 patients and 13 patients respectively. Except for the study by Brooke et al. (1992), the population studied is heterogeneous, including other causes of brain injuries . The study with the highest level of evidence (level 1 or 2) is the one by Brook et al. published in 1992. Twenty-one patients in the subacute phase after severe TBI were included in this study with 11 patients in the propranolol group and 10 patients in the placebo group. The treatment started at 60 mg per day, progressively increased up to a maximum of 420 mg per day in 60 mg increments every 3 days with an 8-week follow-up. Authors showed a significant reduction of the agitation intensity (assessed by the Overt Aggression Scale) in the group treated by Propranolol vs. controls. The maximum effect was obtained 5 weeks after treatment, the use of contentions had also significantly decreased in the treated group. However, the number of agitation episodes did not significantly differ in the two groups. No major adverse events were reported in this study. Beyond this study, the main risk with beta-blockers use is a drop in arterial blood pressure and heart rate. Thus, the risk appears relatively limited for young patients, especially when the dose used is relatively low (below 80 mg per day).
Overall, the prescription of beta-blockers and especially propranolol can be recommended for the management of agitation with a B grade. It is the Gold Standard when a TBI patient suffers from both high-blood pressure and agitation. It is recommended to perform an electrocardiogram before beginning the treatment, try with a test at 20 mg per day then progressively upgrade the doses up to 80 mg a day (some studies have shown an effect with higher dosage up to 320 mg/day) – Expert opinion. In the absence of efficacy after 8 weeks, it is recommended to progressively stop the treatment. There is no marketing authorization (MA) in this indication, and for this reason, beta-blockers should be prescribed according to the criteria of prescription outside MA while respecting contraindications – Expert opinion.
3.2.2
Mood regulating antiepileptics
The use of mood-regulating antiepileptics is driven by two principles: mood-regulating antiepileptics act on neurotransmitters (especially glutamatergic and GABAergic agents) involved in agitation and aggressiveness . The other more practical principle is based on the similarity of manic state symptoms for which several antiepileptics have a recognized indication. Finally, mood-regulating antiepileptics could act on the phenomenon of kindling in the limbic system involved in the classic reactions of agitation or aggressiveness sometimes observed in certain patients .
The analysis of the literature focused on 5 articles concerning four products: carbamazepine , oxcarbazepine , valproate and lamotrigine . The level of evidence remains quite modest: only one single randomized, double-blind study (level 1-2) comparing oxcarbazepine and placebo . In this study concerning 48 aggressive patients with various medical causes, 24 patients benefited from an oxcarbazepine treatment with an initial dosage of 1200 mg/day, increased to a maximum of 2400 mg over a 10-week period. A significant decrease of aggressiveness (assessed by the Global Overt Aggression Rating) was unveiled in the oxcarbazepine group vs. controls. Nine patients had to stop the study because of adverse side effects. The number of patients with TBI was not reported, nor was the delay before the onset of symptoms. In a level-3 open study, the effect of carbamazepine was studied on 10 patients with agitation and aggressiveness following TBI at different stages (between 11 and 188 weeks post-TBI) . Authors reported a significant agitation decrease for carbamazepine doses ranging from 400 to 800 mg/day for an 8-week treatment period. An improvement in irritability and disinhibition was also noted. The individual study showed that the positive effect was important in 5 patients, moderate in 3 patients and marginal in 2 patients. No cognitive adverse events were found in this study. An improvement for several symptoms of the Kluver-Bucy syndrome was noted in a level-3 open study conducted in 4 patients with TBI and bilateral brain lesions . In another level-3 open study, a reduction of aggressive and destructive behavior was described after the start of valproate treatment in 5 patients with severe TBI (several months after the initial trauma). The effect was noted in the first 2 weeks after the beginning of the treatment . The latter was well tolerated, with few side effects, mostly sedative and cognitive ones. More recently, a case study showed a decrease in agitation assessed via the Agitated Behavior Scale under lamotrigine in a patient with severe TBI, 11 months after the initial trauma and after having tried other agents (carbamazepine, trazodone, risperidone and paroxetine) . The lamotrigine treatment prescribed to a maximum dose of 50 mg twice a day was well tolerated. An improved autonomy was observed in the follow-up period.
Overall, the number of study is quite limited and concerns older publications. Several methodological biases limit the impact of the results: e.g. heterogeneity of the population, treatment of agitation and aggressiveness at a chronic stage and not specifically during a crisis, associated medical treatments, assessments scales. Adverse effects on cognitive performances and time needed to perform psychomotor tasks are relatively common with carbamazepine and valproate. These side effects can even lead physicians to stop the treatment . Mood regulating anticonvulsants are the Gold Standard for agitation or aggressiveness after severe TBI if there is an associated epilepsy or bipolar disorders – Expert opinion. In other cases, the level of recommendation does not exceed a grade C for agitation or aggressiveness according to evidence-based medicine and these treatments can only be administered in the framework of a prescription outside MA.
3.2.3
Antidepressants
Why use antidepressants for the agitation and aggressiveness crisis? The first reason is a neurobiological one, since neurotransmitters involved in behavioral disorders could be modulated by the action of antidepressants; mainly serotonin, dopamine and adrenaline. In animal models, studies showed that the level of serotonin is negatively correlated to aggressiveness . Similarly, in patients with TBI, the level of serotonin could influence personality changes, agitation and aggressiveness . Regarding adrenaline and dopamine, these molecules are involved in cognitive functions such as attention and memory as well as executive functions . Alternatively, the depressive state, concomitant of a certain self-awareness of the situation, could promote the emergence of tantrum behaviors like agitation and aggressiveness. In this perspective, antidepressants could act on the cause of behavioral disorders.
The review of the literature identified only 4 articles where the objective was the study of antidepressants on the agitation and aggressiveness crisis. Only one study with a control group (level 1-2) was published ; the other three studies are open studies or case series (level 3-4) . Two molecules were experimented: sertraline and amitriptyline .
The only study with a control group focused on nine patients with severe TBI during the subacute phase (in the first 2 weeks after TBI) . Sertraline was started at the dose of 100 mg/day in six patients. The other three patients received placebo for 2 weeks. Agitation and orientation were monitored daily. The authors observed a decrease of the agitation score in both groups, without any significant difference between groups. The main limit of the study was its small sample. In an open trial conducted on 13 patients with TBI, sertraline was introduced at a dose of 50 mg/day, with a progressive increase up to 200 mg/day according to efficacy and tolerance . The severity of TBI and time since TBI were very variable according to patients (time since TBI range: 1 month to 9 years). Aggressiveness, irritability and depression were evaluated every 2 weeks over an 8-week period. Authors observed a decrease of aggressiveness in 8 patients out of 10, and reduction of irritability in 10 patients out of 10. One can note that the improvement was visible right from the first week and that not obvious relationship was evidenced between mood swings and behavioral changes. In a study on two cases of patients with Kluver-Bucy syndrome after TBI, sertraline (up to the dose of 150 mg/day) showed some efficacy on agitation, hyperorality, hypersexuality after the failure of other treatments (propranolol, carbamazepine) . In one of the cases, it seemed that the association of sertraline and haloperidol represented the best therapeutic strategy. In the study by Mysiw et al. , 58 patients hospitalized after TBI and in the confusion phase were included. Twenty of them presented with agitation (motor agitation, verbal or physical violence). The treatment was started at the dose of 25 mg/day, then increased by 25 mg increments every 3 days up to 150 mg/day. A positive response was observed in 13 patients (65%) in the week following the beginning of treatment (thus with a low dose). There was no change in the other 6 patients (30%) and authors noted increased agitation in one patient (5%).
Overall, antidepressants remain the treatment for depression. Regarding management of agitation and aggressiveness, the literature remains poor with a low level of evidence. Sertraline is the most studied medicine and should be preferred if an antidepressant treatment is prescribed in an agitated or aggressive patient – Grade C. It could be relevant to associate sertraline and a neuroleptic for Kluver-Bucy syndrome with temper tantrum symptoms (Grade C). Amitriptyline showed a certain effectiveness on agitation from 25 mg/day and could be recommended as second-line treatment (Grade C). The review of the literature showed that the time course of the drug effects could be quick, independently of the antidepressant effect. The indication should be weighted with the risks of adverse events: lowered epileptogenic threshold, increased confusion, even anxiety, anticholinergic effects of tricyclic antidepressants.
Antidepressants should be chosen when there is an associated depressive component during the agitation or aggressiveness crisis – Expert opinion. Outside of this specific context, antidepressants appear as second-line treatment and should be prescribed while abiding by criteria associated with a prescription outside of MA – Expert opinion.
3.2.4
Neuroleptics
Neuroleptics are used in the agitation crisis to obtain a quick sedation in order to protect the patient from himself/herself, closed ones or the healthcare team.
The review of the literature only found 4 articles corresponding to open studies or case-series (level 3-4). Drug agents studied were olanzapine , clozapine , quetiapine , and ziprasidone .
Clozapine was used to treat psychotic symptoms, anger fits or aggressiveness refractory to other treatments in 9 patients with TBI . A noticeable improvement of aggressiveness was observed in 2 patients. A moderate agitation decrease was reported in 3 patients. In 3 other patients, treatment response could not be refined probably due to a too-short treatment duration. Several adverse events occurred including seizures in two patients. On top of the clastic side effects of neuroleptics, clozapine presents a higher risk of agranulocytosis. Due to this risk, it is not recommended as first-line treatment. In a 6-week open pilot study, a quetiapine treatment was tried in 7 patients presenting with aggressiveness that appeared in the aftermath of TBI . Patients were included at least 3 months after TBI. The initial dose of quetiapine was 25 mg/day, then the treatment was increased progressively up to 300 mg/day. An improvement of the aggressiveness as assessed by the Overt Aggression Scale – Modified (OAS-M) was observed and the treatment was well tolerated. A study reported the effect of treatment with ziprasidone (medication available in France only in the context of a marketing authorization) on agitation during the post-traumatic amnesia period in 5 patients with TBI . According to the cases, the treatment was prescribed for a period ranging from 35 to 68 days at the dose of 20 to 80 mg/day. Authors described a quick improvement of the agitation assessed by the Agitated Behaviour Scale (ABS) without adverse events. In a case study, an improvement of delirious symptoms and anger fits were observed after the introduction of olanzapine .
Overall, few articles evaluated the effects of neuroleptics on the agitation or aggressiveness crisis in patients with TBI. However, these are studies with a low level of evidence. Nevertheless, some neuroleptics have a market authorization in this indication. This mainly concerns loxapine in its injectable form for the treatment of “agitation, aggressiveness and anxiety states associated with psychotic disorders or some personality disorders”. It is thus recommended to use this treatment in case of crisis but the duration of use should be as short as possible because of the risks of adverse events: epilepsy, neuroleptic malignant syndrome, excessive sedative effect that could promote the risk of swallowing disorders (choking or aspiration) or falls; cardiovascular risks; potentially deleterious effects on brain plasticity and thus on the recovery potential – Expert opinion. Neuroleptics can also be proposed in the treatment of agitation in case of associated delirious symptoms – Expert opinion. In other cases, neuroleptics are not recommended by the expert group. If the neuroleptic treatment is used, it is preferable to use second generation neuroleptics or atypical neuroleptics – Expert opinion.
3.2.5
Benzodiazepines
Benzodiazepines are used to manage the agitation crisis to obtain a quick sedation in order to protect patients from themselves, their closed ones or the healthcare team.
The review of the literature did not identify any article specifically evaluating the effect of benzodiazepine treatment in the management of agitation or aggressiveness crisis in patients with TBI.
Overall, some benzodiazepines have an indication in the agitation crisis like clorazepate dipotassium. Their use will be limited to situations where anxiety is the predominant symptom by privileging a short duration of use (symptomatic prescription) – Expert opinion. In patients with TBI, the use of benzodiazepines must take into account the risk of promoting or aggravating respiratory distress, triggering a paradoxical effect on agitation, inhibiting brain plasticity capacities. There is also a risk of dependence and addiction.
3.2.6
Amantadine
Amantadine is a pharmacological agent acting on several neurotransmitters: dopaminergic action by increasing the presynaptic release of dopamine and inhibiting the post-synaptic recapture . Amantadine also has an inhibiting action on glutamate by blocking the N-methyl-D-aspartate (NMDA) receptors channels . Amantadine could also have a serotonergic action and an effect on mood regulation . Finally, amantadine might stimulate some neurotrophic factors in rats and act on brain plasticity mechanisms . The justification to use amantadine in patients with agitation or aggressiveness after TBI is mostly based on the cognitive effects of this molecule . Relationships between cognitive functions and behavioral disorders have already been discussed in this article.
The literature review found two randomized studies that compared the effects of amantadine vs. placebo on aggressiveness and irritability in patients with TBI after the subacute phase . These recent publications could not be analyzed by the expert group as they were published after the reviewing protocol. They yield contradictory information. In the first monocenter study, there is a significant decrease of irritability and agitation in the group of 38 patients who received amantadine at the dose of 100 mg morning and noon vs. the control group ( n = 38). These results are not found in the multicenter study published in 2015 on 82 patients (86 patients in the control group). Two older open studies, on 12 patients (including 10 with TBI) and two TBI patients TC showed a positive effect of amantadine to reduce agitation and aggressiveness during the post-traumatic amnesia period.
Overall, the benefit of amantadine on agitation and aggressiveness remains to be validated and in the current state of knowledge and clinical practice, this treatment does not have specific guidelines in this indication for patients with TBI.
3.2.7
Buspirone
Buspirone presents an anxiolytic activity devoted from sedative effect, myorelaxant effect and anticonvulsant activity. The mechanism of action of buspirone is not completely resolved yet. In the current state of knowledge, it seems that its activity essentially unveils its effects on serotonin receptors. This treatment acts mainly as a presynaptic 5 HT1A receptors agonist and post-synaptic 5 HT1A receptors partial agonist. Buspirone also has an antagonist activity of D2 receptors essentially a presynaptic one, for the recommended doses in anxiety disorders. It does not interfere with benzodiazepine and GABAergic receptors.
The literature review identified 4 articles consisting of case series or case studies (level 3-4). Agitation and aggressiveness improvement is reported in these four articles that concerned respectively 13 patients with TBI , 10 patients , 2 patients (including 1 with TBI) and 1 TBI patient .
Overall, the level of evidence remains limited but these results converge to suggest an efficacy of buspirone in agitated or aggressive behaviors after TBI. This treatment represents an interesting alternative to benzodiazepines in case of anxiety associated with agitation or aggressiveness. In the absence of anxiety, this treatment can be tried as second-line treatment and after the failure of other treatments and in the framework of the legal guidelines on treatments outside MA – Expert opinion.
3.2.8
Methylphenidate
Methylphenidate is a psychostimulating agent, assimilated to amphetamines, acting on the monoaminergic pathways by increasing the quantity of dopamine and noradrenaline in the synaptic cleft by blocking the presynaptic recapture of these neurotransmitters . This treatment could then act on agitation and aggressiveness via cognitive effects. In a randomized vs. placebo study, a significant improvement of spatial attention and working memory was highlighted in 18 patients with TBI who received a unique dose of 20 mg of methylphenidate vs. subjects in the control group who received placebo .
The literature review showed an improvement of aggressiveness under methylphenidate in the two studies and an improvement of aggressiveness in one study in patients with TBI.
The first study is a randomized vs. placebo study conducted on 38 patients with moderate to severe TBI (level 1-2). The treatment was increased progressively up to 30 mg/day over a 4-week period and sustained for 2 weeks. Authors observed an improvement of the aggressiveness evaluated by the “Anger-KAS, State-Trait Anger Scale” and the “POMS anger/hostility factor”. Nevertheless, the improvement of aggressiveness was not the main objective of this study, which could constitute an observation bias.
The second one was also a randomized vs. placebo cross-over study assessing the effect of methylphenidate in 12 patients with cognitive disorders secondary to moderate to severe TBI at the chronic stage (between 14 and 108 months post-TBI) (level 1-2). Patients received methylphenidate at the dose of 0.3 mg/kg/day for a week followed by a placebo treatment for a week or vice-versa. A significant decrease of the aggressive behavior assessed by the “Katz Adjustment Scale” was validated even though it was not the main objective of this study, which focused more on cognitive disorders. In this case again, an observation bias could be brought forward.
The last study reported increased agitation in a TBI patient treated by methylphenidate (level 4).
Overall, methylphenidate effects are based on a small number of studies with results suggesting an effect on aggressiveness evaluated in a collateral manner in two randomized studies vs. placebo. A case study suggests an increase of the agitation induced by methylphenidate. At this stage, no guideline was elaborated by the expert group.
3.2.9
Hydroxyzine
Hydroxyzine is an anxiolytic derived from piperazine not belonging to phenothiazine agents and benzodiazepines. Hydroxyzine is an antihistaminic receptor antagonist of central and peripheral H1 receptors presenting anticholinergic properties.
The analysis of the literature did not yield any articles answering to this study’s criteria. Hydroxyzine can constitute an alternative to benzodiazepines when agitation is associated with anxiety symptoms for which this treatment has an indication – Expert opinion. This treatment has the advantage of causing less respiratory depression than most medicines in the benzodiazepine drug class but, according to the dose, it can increase vigilance disorders with risk of swallowing disorders and increased confusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






