Abstract
Introduction
Brain-machine interfaces (BMIs) use brain activity to control external devices, facilitating paralyzed patients to interact with the environment. In this review, we focus on the current advances of non-invasive BMIs for communication in patients with amyotrophic lateral sclerosis (ALS) and for restoration of motor impairment after severe stroke.
BMI for ALS patients
BMI represents a promising strategy to establish communication with paralyzed ALS patients as it does not need muscle engagement for its use. Distinct techniques have been explored to assess brain neurophysiology to control BMI for patients’ communication, especially electroencephalography (EEG) and more recently near-infrared spectroscopy (NIRS). Previous studies demonstrated successful communication with ALS patients using EEG-BMI when patients still showed residual eye control, but patients with complete paralysis were unable to communicate with this system. We recently introduced functional NIRS (fNIRS)-BMI for communication in ALS patients in the complete locked-in syndrome (i.e., when ALS patients are unable to engage any muscle), opening new doors for communication in ALS patients after complete paralysis.
BMI for stroke motor recovery
In addition to assisted communication, BMI is also being extensively studied for motor recovery after stroke. BMI for stroke motor recovery includes intensive BMI training linking brain activity related to patient’s intention to move the paretic limb with the contingent sensory feedback of the paretic limb movement guided by assistive devices. BMI studies in this area are mainly focused on EEG- or magnetoencephalography (MEG)-BMI systems due to their high temporal resolution, which facilitates online contingency between intention to move and sensory feedback of the intended movement. EEG-BMI training was recently demonstrated in a controlled study to significantly improve motor performance in stroke patients with severe paresis. Neural basis for BMI-induced restoration of motor function and perspectives for future BMI research for stroke motor recovery are discussed.
1
Introduction
A brain-machine interface (BMI) uses brain activity directly without any motor involvement for activation of a computer or other external devices. A considerable amount of scientific literature was created on BMIs during the past 15 years but most of this literature is experimental in nature, controlled studies on clinical applications are rare. Here we present an overview of the available studies, which fulfill at least some methodological criteria of a controlled clinical trial. We focus on two applications where most of the work was done: BMI in paralysis from amyotrophic lateral sclerosis (ALS) and BMI in the motor rehabilitation of chronic stroke.
2
ALS and need for BMI
Amyotrophic lateral sclerosis is a progressive motor disease of unknown etiology resulting eventually in a complete destruction of the peripheral and central motor system but only affecting sensory or cognitive functions to a minor degree . There is no treatment available; patients have to decide to accept artificial respiration and feeding after the disease destroys respiratory and bulbar functions for the rest of their life or to die of respiratory or related problems. If they opt for life and accept artificial respiration, the disease progresses until the patient loses control of the last muscular response, which is usually the eye muscle or the external sphincter. The resulting condition is called completely locked-in state (CLIS) . If rudimentary control of at least one muscle is present, we speak of a locked-in state (LIS) . Almost all people with ALS experience a motor speech disorder as the disease progresses. Initial symptoms typically do not interfere with speech intelligibility and may be limited to a reduction in speaking rate, a change in phonatory (voice) quality, or imprecise articulation. At some point in the disease progression, 80 to 95% of patients with ALS are unable to meet their daily communication needs using natural speech. Later, most become unable to speak at all . For them, communication support involves a range of augmentative and alternative communication (AAC) strategies involving low- and high technology (speech generating devices) options . Clinical decision-making related to communication is quite complex as screening, referral, assessment, acquisition of technology, and training must occur in a timely manner, so when residual speech is no longer effective, AAC strategies are in place to support communication related to personal care, medical care, social interaction, community involvement, and perhaps employment. Hence there is a need for an assistive technology to help patients in CLIS to communicate needs and feelings to their family member/caregiver.
2
ALS and need for BMI
Amyotrophic lateral sclerosis is a progressive motor disease of unknown etiology resulting eventually in a complete destruction of the peripheral and central motor system but only affecting sensory or cognitive functions to a minor degree . There is no treatment available; patients have to decide to accept artificial respiration and feeding after the disease destroys respiratory and bulbar functions for the rest of their life or to die of respiratory or related problems. If they opt for life and accept artificial respiration, the disease progresses until the patient loses control of the last muscular response, which is usually the eye muscle or the external sphincter. The resulting condition is called completely locked-in state (CLIS) . If rudimentary control of at least one muscle is present, we speak of a locked-in state (LIS) . Almost all people with ALS experience a motor speech disorder as the disease progresses. Initial symptoms typically do not interfere with speech intelligibility and may be limited to a reduction in speaking rate, a change in phonatory (voice) quality, or imprecise articulation. At some point in the disease progression, 80 to 95% of patients with ALS are unable to meet their daily communication needs using natural speech. Later, most become unable to speak at all . For them, communication support involves a range of augmentative and alternative communication (AAC) strategies involving low- and high technology (speech generating devices) options . Clinical decision-making related to communication is quite complex as screening, referral, assessment, acquisition of technology, and training must occur in a timely manner, so when residual speech is no longer effective, AAC strategies are in place to support communication related to personal care, medical care, social interaction, community involvement, and perhaps employment. Hence there is a need for an assistive technology to help patients in CLIS to communicate needs and feelings to their family member/caregiver.
3
Types of BMIs
Brain-machine interface technology has generated considerable research interest for the “locked-in” patients such as those in the late stages of ALS. BMI research includes invasive (implantable electrodes on or in the neocortex) and non-invasive means (including electroencephalography (EEG), magnetoencephalography (MEG), functional magnetic resonance imaging (fMRI), and near-infrared spectroscopy (NIRS)) to record brain activity for conveying the user’s intent to devices such as simple word-processing programs. Non-invasive methods have been utilized more extensively than invasive methods for people with disabilities (such as those with ALS) . While those with ALS and other conditions who are in a “locked-in” state have motivated research in this area, very few systems have been successful with this population.
3.1
EEG-based BMI for ALS patients
Three different types of EEG-based BMI are currently in use namely slow cortical potential (SCP)-BMI, sensorimotor rhythm (SMR)-BMI and P300-BMI. Based on the detailed comparison of three different signatures of EEG-based BMIs as reported by Birbaumer , it was concluded that in ALS patients with functioning vision and eye control, SMR-BMI and P300-BMI shows the most promising results. SCP-BMIs need more extensive training than other BMIs but may have the best stability and are more independent of sensory, motor, and cognitive functioning necessary for its application in the LIS and the CLIS patients. The patients described earlier had high success rates with SCP-BMI training but only after many sessions. It has been postulated that some cognitive impairment and changes in EEG signatures in late stage ALS may contribute to the lack of success using EEG-BMI technology as the technology was introduced after the participants had become “locked-in” . Kuebler and Birbaumer have shown that patients in CLIS do not reach sufficient BMI control for communication with EEG parameters. Kuebler and Birbaumer speculated that extinction of goal directed thinking may prohibit operant learning of brain communication. The most successful application for communication has occurred in people at the beginning stages of the disease . Hence there is a need to find an alternative neuroimaging technique to design a more effective BMI to help ALS patient in CLIS with communication.
3.2
fMRI-based BMI for ALS patients
fMRI measures increases and decreases of paramagnetic load of blood flow to activated pools of neurons, particularly to apical dendrites . Paramagnetic charge is determined by blood oxygenation level dependent (BOLD) flow, which reflects local metabolic deficiencies of the vascular bed supplying the neurons. Logothetis et al. have shown that the correlation of local blood flow change and the BOLD signal is particularly high for the neuronal inflow to the apical dendrites reflecting primarily intracortical activity. The fMRI-based BMI is difficult to apply on ALS patient because it is expensive, bulky and impossible to move to patients’ home. Moreover, the patient enclosed in the scanner does not experience a satisfying environment for communication. Still instrumental learning of BOLD control turned out to be successful in neuropsychiatric disorders .
3.3
fNIRS-based BMI for ALS patients
NIRS is an emerging neuroimaging modality which employs near-infrared light to non-invasively or invasively investigate cerebral oxygenation changes in healthy and neurologically challenged adults and children . It has reasonable spatial (about 1 cm) and good temporal (about 1 ms) resolution and is relatively robust to motion artifact, thereby enabling it to be suitable for investigating everyday tasks . Thus in contrast to functional magnetic resonance imaging, a NIRS-based BMI can easily be applied at the bedside of these highly impaired and difficult to move patients in desperate need for communication.
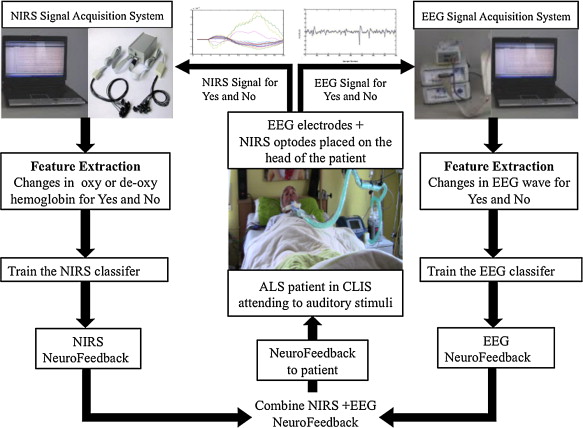
Sitaram et al. published the first controlled evaluation of a NIRS BMI. Using motor imagery with a 20 channels NIRS system over sensorimotor cortex they reported 89% correct classification of right and left hand imagery without any training and the use of a hidden Markov model as a classifier . Very recently NIRS was successfully used to investigate the functional activations in the cortex of a CLIS patient in response to auditorily presented stimuli containing correct or incorrect statements and open questions . The hemodynamic change in the motor cortex of the CLIS patient was recorded across many sessions spread over more than a year and was used to train a classifier to predict the “yes” and “no” answering pattern of the CLIS patient who was previously trained to use an EEG-BMI without success . The trained classifier was able to provide online feedback (“your answer was classified as (in) correct”) to the patient with performance rate of 71.76%. This is the first carefully documented case of communication in a CLIS patient with BMI, which holds promise and raises the hope for communication in CLIS. Hence, to further validate the preliminary findings of our lab and refine the technology of fNIRS-based BMI for communication in CLIS patients extensive studies are presently carried out on CLIS patients using combined fNIRS-EEG-based BMIs. The complete setup of the combined fNIRS-EEG-based BMIs developed for communication in CLIS patient is shown in Fig. 1 .
4
BMI for motor recovery in chronic stroke patients
Stroke is one of the leading causes of acquired disability in the adult population worldwide . While for patients with incomplete hand paralysis repetitive motor tasks may restore motor function , patients with severe hand paresis do not profit from current rehabilitation strategies as they are not able to perform the therapeutic movements. For those patients, BMI training represents a promising strategy to recover motor function.
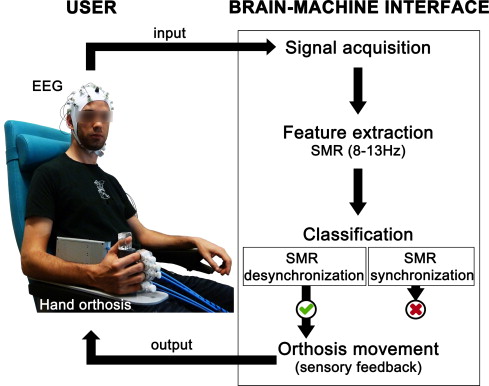
BMI training for stroke motor recovery involves repetitive motor tasks with the paretic limb through decoding of brain signals related to processing of motor information (e.g., actual movement or motor imagery) and contingent movement of the paretic limb guided by an external device providing sensory (visual and kinesthetic) feedback. The brain signal most commonly used to control BMI for motor recovery is the sensorimotor rhythm, or SMR, an oscillatory brain activity located over the sensorimotor cortex in the range of 8–13 Hz . The SMR decreases its amplitude (SMR desynchronization) during processing of motor information while a high SMR amplitude (SMR synchronization) is associated with processing of rest or an “idling cortical area” . Therefore, changes in SMR amplitude can be used to trigger an external device guiding paretic limb movements and providing sensory feedback contingent to user’s intention to move ( Fig. 2 ). The first demonstration of a SMR-based BMI for control of paralyzed limb movements driven by an external device was given in 2000 by Pfurtscheller’s group, in a study with a tetraplegic patient .