Bowed Legs
B. David Horn
David A. Spiegel
CLINICAL PRESENTATION
Angular deformities of the lower extremity in children are a common source of concern and anxiety for families. The majority of the time, these represent normal variations, are self-limiting, and correct with normal growth and development. Rarely, however, these can be secondary to localized growth disturbances or may be a manifestation of a systemic disease or disorder and require surgical or brace treatment.
The evaluation of the child with bowing of the lower extremity starts with a thorough history and physical examination. The history can be very useful in narrowing the differential diagnosis: sudden onset of the bowing suggests a traumatic or postinfectious cause, while gradual onset and progression is more consistent with a developmental condition or systemic disorder. The general health of the child should be evaluated through the history, and a family history should also be obtained, as some patients with bowlegs will have a positive family history for physiologic bowing, skeletal dysplasia, or rickets.
CLINICAL POINTS
Children are most often affected.
This self-limiting condition generally resolves over time.
History may be significant.
PHYSICAL FINDINGS
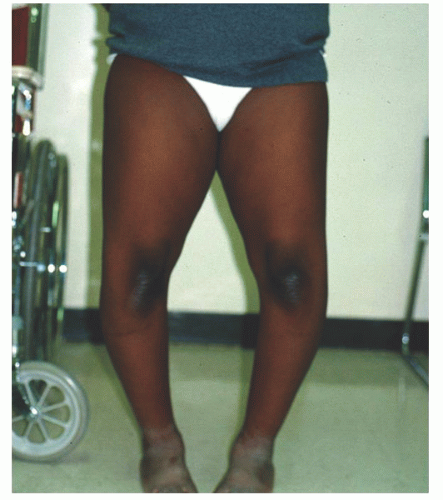
The physical examination should include evaluation of the child’s height and weight. Height <5th percentile and weight >95th percentile are potential indicators of skeletal dysplasia or Blount disease.1 The appearance of the limb in the frontal, sagittal, and axial planes should then be assessed (Fig. 55-1). This should be done with the patella pointing forward in order to standardize assessment of the limb and remove the effect of hip rotation from the exam.2 A child with medial tibial torsion, for example, frequently has the appearance of tibia vara because the hip (and lower limb) is externally rotated to compensate for the medial tibial torsion. This pseudobowing is easily differentiated from tibia vara by examining the lower limb in a neutral position (i.e., with the patella forward), since the tibia has a normal alignment in pseudobowing. The location of the deformity should also be evaluated: a localized deformity suggests a localized growth disturbance such as Blount disease or posttraumatic deformity, whereas a generalized deformity suggests a systemic disease such as rickets or a metabolic disease. The child’s gait should also be assessed. The presence of a lateral thrust (lateral deviation) of the affected knee in stance phase is a significant finding and is an indication for further evaluation.
STUDIES (LABS, X-RAYS)
Radiographs are not routinely indicated for bowing of bilateral lower extremities in children <2 years of age. Indications for radiographs include age >24 months, stature <5th percentile, a lateral thrust while walking, and unilateral deformity. A standing radiograph should be obtained of each lower extremity in the anteroposterior (AP) and lateral projections. Care should be taken to obtain the radiographs with the patella pointed straight forward, as rotated images are difficult to interpret and can lead to misdiagnosis. If a systemic disorder is suspected, a skeletal survey may be ordered to image other bones that may be affected.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree