Bites
Human Bites
General Information
Human bites commonly occur on the hand following fights (fight bite) (Fig. 1). These wounds are often complicated by bacteriologic infection because of the complex flora of the human mouth.
Diagnostic Criteria
Physical Examination
The bites are usually located over the extensor surface of the hand in the vicinity of the metacarpophalangeal joints. One should inspect the area of the bite for evidence of infection and palpate the adjacent joints to look for evidence of septic arthritis.
Other Assessment
Patients with evidence of infection should have a white blood count with a differential. Radiographs should be done if there is a concern for fracture, septic arthritis, or osteomyelitis.
Treatment
All wounds should be explored to determine the depth of the bite. The extensor tendon should be inspected. During the exploration, specific inspection of the joint capsule should be done to determine if the bite extends to the joint space. The finger should be examined in both flexion and extension.
Superficial wounds can be treated with irrigation and débridement. Tetanus immunization should be updated whenever appropriate. Usually these wounds are treated with twice daily dressing changes until the wounds heal by secondary
intention. Patients should be instructed in range of motion exercises for the hand to limit the occurrence of stiffness.
intention. Patients should be instructed in range of motion exercises for the hand to limit the occurrence of stiffness.
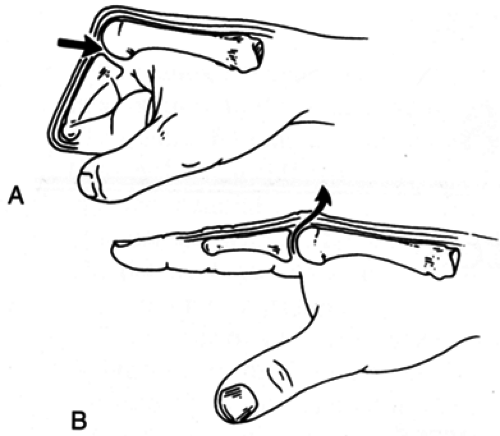 FIG. 1. A: A tooth penetrates the fully flexed metacarpophalangeal joint of a closed fist. B: As the digit is extended, the inoculum is trapped because the path of entrance is now closed. |
Deep wounds and wounds with joint space involvement should be treated by extending the wound and thoroughly irrigating the joint and tendon space. The wounds should be packed open and the patient should be instructed in local care.
Often these patients need intravenous antibiotics. Patients with established bone and joint infection need early referral to a hand specialist.
Key Points
Staphylococcus aureus is the most common organism causing hand infections after human bite. Eikenella corrodens can also cause infection following human bite.
One should carefully inspect the wound to evaluate for joint space penetration or early septic arthritis. Satisfactory débridement is crucial to obtaining a good outcome.
Initial antibiotic therapy usually requires both a first-generation cephalosporin and penicillin. Culture results give the physician the opportunity to use specific antibiotics.
Cat and Dog Bites
General Information
Cat and dog bites are the most common bites seen for emergency evaluation. Untreated, these bites are commonly complicated by infection, often by alpha Streptococcus, Staphylococcus aureus, and Pasteurella multocida.
Diagnostic Criteria
History
Most often patients are bitten or scratched on the hand when attempting to handle the animal. It is important to determine whether the bite was provoked in some way. If the bite was not provoked, then rabies prophylaxis should be considered. These bites are often painful and associated with the early onset of infection.
Physical Examination
The physical examination should include recording the patient’s temperature, observing the bites for location and number; careful assessment for local tenderness, erythema, subcutaneous abscess, and deep infection; palpation of the arm for evidence of abscess, ascending infection, and tender proximal adenopathy.
Other Assessment
Patients who have developed a significant infection or abscess require a complete blood count.
Treatment
Usually the wounds are small puncture sites that may need to be opened with an incision to allow thorough inspection of the bite and débridement of devitalized tissue. Obtain cultures of any suspicious fluid. Usually the wound should be left open to granulate. When indicated, update the tetanus status. The patient should be instructed to perform twice-daily dressing changes and issued a prescription for oral antibiotics (usually Augmentin).
Aftercare
Patients should be followed carefully to look for evidence of bite site infection. Patients should be instructed in range of motion exercises and twice-daily dressing changes. Some patients may benefit from more intensive local wound care methods (whirlpool treatments) and organized occupational therapy
Key Points
Rabies has been reported after domestic cat bite. If the animal cannot be observed, the local health department should be consulted for advice on rabies prophylaxis. One should always determine the rabies immunization status of the biting animal.
The deep spaces of the hand are often inoculated because of the configuration of the animal’s tooth.
These infections are usually caused by the normal flora of the animal’s mouth.
Patients who present with an established hand abscess usually need intravenous antibiotics, serial débridement, and intensive occupational therapy.
Selected Reference
Goldstein EJ. Bite wounds and infection. Clin Infect Dis 1992;14:633–638.
Other “Wild Animal” Bites
Unusual wild animal bites (raccoons, skunks, foxes, bats, and some rodents) are seen in the emergency setting and require treatment similar to the treatment of dog and cat bites. One should obtain a careful history about the event that caused the bite and the location and type of the animal because these bites carry a higher risk for rabies. Usually, if the animal is not observable or if the bite was unprovoked, rabies prophylaxis is indicated. If the animal exhibited signs of rabies at the time of exposure, rabies treatment should begin as soon as possible. One should consult with the local health department or an infectious disease specialist if there is a question about the need for rabies treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






