Biceps Tenodesis—Indications, Techniques, and Results
Jonathan J. Streit
Reuben Gobezie
INTRODUCTION
The role of the long head of the biceps (LHB) tendon in producing anterior shoulder pain, first described by Hitchcock and Bechtol49 in 1948, is now widely accepted.103,110 Uncertainty about its role as a shoulder stabilizer, however, has led to the development of different schools of thought regarding the benefits of biceps tenodesis.41,43,50,58,89,92,101,125 The procedure’s popularity has waxed and waned, but its ability to dramatically reduce pain has led to a determined search for the ideal surgical technique. Since first being described by Gilcreest in 1926,38 biceps tenodesis has been attempted using fixation sites both proximal16,36,55,56,64,98,102 and distal,10,14,71 and using fixation methods which have included bone tunnels,68 interference scr ews,15,36,54,55 and 56,64,68,71,88,98,99 suture anchors,52,54,68,88,99 bony keyholes,88 and suturing to adjacent structures such as the conjoint tendon or short head of the biceps,102 or directly into bone within or adjacent to the bicipital groove.102
The biceps tendon may be the primary source of a patient’s shoulder pain when it is dislocated or becomes inflamed within the bicipital groove, or it may contribute to pain in conjunction with other pathologic entities, including rotator cuff tears, impingement, superior labral tears,110 and osteoarthritis,31 making tenodesis useful as an adjunct treatment when addressing pathology in these areas. By virtue of its position in the anterior shoulder, the biceps tendon is often injured when other structures become incompetent, or by the same mechanism of injury affecting the other structures. Since the synovial lining of the glenohumeral joint is contiguous with the LHB tendon sheath, the conditions arising within the joint may also cause pain with the movement of the LHB tendon.80,108
Both tenodesis and tenotomy of the LHB tendon function to relieve anterior shoulder pain by unloading a damaged or inflamed tendon and tendon sheath. Biceps tenodesis is considered superior to tenotomy for three primary reasons68,70: (1) Reattachment of the proximal biceps tendon maintains a normal length—tension relationship and prevents muscle atrophy, (2) elbow flexion and supination strength are maintained at near-normal levels, and (3) reattachment of the proximal biceps tendon affords a better cosmetic result by avoiding the “Popeye” deformity often seen following biceps tenotomy or rupture. The incidence of pain attributable to unchecked biceps contraction following tenotomy has been considered nonsignificant in comparison to that following tenodesis,14,87 but this consideration in combination with loss of strength and cosmetic deformity has made tenodesis the more desirable procedure in most cases. The loss of the proximal attachment of the LHB has been shown to lead to a 20% loss of forearm supination strength, and an 8% to 20% loss in elbow flexion strength.66,73 Currently, biceps tenodesis is preferred over tenotomy in all patients except for older patients in whom cosmetic concerns and diminished strength are less important than are early pain relief and minimal healing time.
Biceps tenodesis has often been approached cautiously due to the fact that the procedure removes a potential stabilizer from an inherently unstable joint. Neer cautioned that impingement could result from tenodesis due to a loss of the head depressor effect of the tendon,78 and indeed Warner and
McMahon demonstrated in 1995 that the LHB resists superior translation of the humeral head with scapular plane abduction, and suggested that impingement could result, especially in individuals with type II or III acromions.125 The biomechanical studies by Yamaguchi et al.129 and Levy et al.62 have shown that the biceps tendon is a head depressor, while others have found evidence to the contrary.50,58,101,125 The LHB has also been described as an anterior stabilizer,65,86,104 a posterior stabilizer,72 a contributor to elbow flexion with minimal activity at the shoulder,108,119,128 and even as a vestigial structure.63 Whatever its true importance in the normal shoulder may be, the role of LHB as a stabilizer is thought to be increased in cases of rotator cuff deficiency,12 although thickening of the tendon, as observed by Leffert and Rowe,61 is now thought to be due to chronic inflammation from repeated impingement rather than hypertrophy due to increased demands.129
McMahon demonstrated in 1995 that the LHB resists superior translation of the humeral head with scapular plane abduction, and suggested that impingement could result, especially in individuals with type II or III acromions.125 The biomechanical studies by Yamaguchi et al.129 and Levy et al.62 have shown that the biceps tendon is a head depressor, while others have found evidence to the contrary.50,58,101,125 The LHB has also been described as an anterior stabilizer,65,86,104 a posterior stabilizer,72 a contributor to elbow flexion with minimal activity at the shoulder,108,119,128 and even as a vestigial structure.63 Whatever its true importance in the normal shoulder may be, the role of LHB as a stabilizer is thought to be increased in cases of rotator cuff deficiency,12 although thickening of the tendon, as observed by Leffert and Rowe,61 is now thought to be due to chronic inflammation from repeated impingement rather than hypertrophy due to increased demands.129
What evidence is there for the belief that biceps tenodesis will cause problems due to loss of the tendon’s head depressor action? Isolated tenodesis procedures have historically demonstrated a high failure rate,10,28,49,66,92 which was presumed to be due to impingement.125 However, the loss of acromiohumeral distance resulting from the procedure appears to be minimal: Boileau et al.14 evaluated the outcomes of 68 patients following arthroscopic biceps tenodesis or tenotomy performed in conjunction with other procedures at an average of 35 months, and found that the average reduction in acromiohumeral distance was 1.1 mm; only one patient had developed glenohumeral arthritis by the time of followup. Walch et al. similarly found that biceps tenotomy led to an average decrease in acromiohumeral distance of 1.3 mm at 57 months postoperatively.122 This loss of acromiohumeral distance is similar to that seen after simple debridement and is less than that found after acromioplasty.35,53,116 Despite the small loss in acromiohumeral distance demonstrated in these studies, which may strengthen the view that tenodesis removes a head depressor, biceps tenodesis is currently employed successfully by many surgeons as an adjunct therapy or palliative treatment for a variety of painful shoulder conditions.
Anatomy
The anatomic location of the LHB tendon leaves it vulnerable to damage, especially in association with subacromial impingement and superior labral tear from anterior to posterior (SLAP) tears of the glenoid labrum. Its origin on or near the supraglenoid tubercle in association with the labrum has been shown to be variable, arising 40% to 60% of the time from the supraglenoid tubercle and glenoid labrum, and the rest of the time from the labrum alone.120 Its position relative to the bony glenoid is also variable, as it arises 22% of the time from an area completely posterior to the tubercle, 33% of the time mostly posterior to the tubercle, 37% of the time with equal contributions from the anterior and posterior labrum, and 8% of the time from an entirely anterior position.120 The wider, intra-articular portion of the tendon44,46 is extra-synovial, with the synovial membrane wrapping around the tendon sheath such that the tendon is not exposed to synovial fluid. The tendon courses anterolaterally to exit the joint beneath the transverse humeral ligament, becoming narrower44,46 as it progresses toward the bicipital groove.
The bicipital groove and the surrounding structures have been implicated as the possible causes of LHB pathology. The groove is wide and shallow at its entrance proximally (9.6 mm × 2.2 mm), becomes somewhat narrower and deeper in the middle portion (8.2 mm × 5.0 mm), and then flattens out at its exit distally (7.3 mm × 2.4 mm).44,46 An anatomic variation in the entrance to the groove, termed as supracondylar ridge, may make medial dislocation more likely by diminishing the relative height of the lesser tuberosity, thereby lessening the trochlear effect of the tuberosities in retaining the LHB tendon.39,73 The medial opening angle of the bicipital groove is also important and variable, averaging 44 degrees, with a range of 9 to 74 degrees based on radiographic studies performed by Pfahler et al.,91 and this may also contribute to biceps instability. Degenerative changes within the groove were noted in 44% of patients with ultrasound-proven LHB pathology, and a shallower groove and smaller medial opening angle were associated with biceps pathology.91 The transverse humeral ligament does not play an important role in stabilizing the LHB within the groove because it is weak and poorly positioned for this function,1,46,73,74,90 but the coracohumeral ligament, superior glenohumeral ligament (SGHL), and pectoralis major tendon have been shown to provide the necessary support,1,22,23,32,46 with the SGHL forming the medial biceps sling in the lateral part of the rotator interval.126
An anatomic evaluation of the distal aspect of the proximal biceps musculotendinous junction has found that this lies at the inferior border of the pectoralis major tendon.94 Re-establishment of an appropriate length—tension relationship of the biceps after tenodesis makes use of this anatomic constant. The importance of this constant was emphasized by Mazzocca et al.,69 who attempted to quantify their results by quantifying post-tenodesis isometric biceps contraction on the involved and uninvolved extremities using what they termed the biceps apex distance.
The blood supply to the LHB has been studied, and some poorly supplied areas have been identified,2,5,95 although their importance remains speculative. Branches of the anterior humeral circumflex artery supply the tendon in the bicipital groove,5 but more adequately supply the superficial portion of this tendon, leaving the gliding undersurface less-well supplied. The intra-articular portion of the LHB tendon receives labral branches from the suprascapular artery, but Abrassart et al.2 showed that the area of the superior glenoid is relatively avascular. Rathbun and Macnab95 also observed a critical zone of avascularity within the intracapsular portion of the tendon, similar to that seen in the supraspinatus tendon, by performing a microvascular injection study of the shoulder. These studies may help to explain why LHB pathology is often noted near the tendon’s origin and within the bicipital groove.
Recently, the LHB tendon has been given more attention as a considerable pain generator at the shoulder. Alpantaki et al.6 noted its sensory and sympathetic innervation with unmyelinated and thinly myelinated fibers, and suggested the presence of a higher concentration of sensory and autonomic neuropeptides in the proximal LHB tendon. These authors proposed that previously documented evidence of the vasoactive and immune regulatory functions of these neuropeptides may play a role in the perception as well as generation of pain in the biceps tendon. Interestingly, the type of innervation found in the tendon was not associated with vascularity in different regions of the tendon. Research into the true mechanisms of pain generation in the tendon and its sheath is ongoing, as
Singaraju et al.110 did not find any correlation between the presence of LHB symptoms or macroscopic pathology with the presence of higher concentrations of nociceptive neuropeptides or microscopic inflammation in the tendon or tendon sheath. These authors did, however, find a weak correlation of pain with tendon sheath vascularity, and concluded that the etiology of anterior shoulder pain related to the biceps tendon in the setting of rotator cuff tears is likely related to a complex interaction of the tendon and the surrounding soft tissues.
Singaraju et al.110 did not find any correlation between the presence of LHB symptoms or macroscopic pathology with the presence of higher concentrations of nociceptive neuropeptides or microscopic inflammation in the tendon or tendon sheath. These authors did, however, find a weak correlation of pain with tendon sheath vascularity, and concluded that the etiology of anterior shoulder pain related to the biceps tendon in the setting of rotator cuff tears is likely related to a complex interaction of the tendon and the surrounding soft tissues.
Pathophysiology
The biceps tendon contributes to anterior shoulder pain when its location and structure cause either inflammatory or traumatic conditions to arise within the tendon or tendon sheath.20,78,79 and 80,83,97 The ability of inflammation in the shoulder due to rotator cuff tearing or arthritic conditions to cause a synovitis which affects the LHB tendon and tendon sheath is well known.19,46,77,79,80,81,82 and 83 Mechanical impingement can lead to degenerative changes within the tendon, and occurs by the same mechanism as rotator cuff impingement due to the anterior location of the biceps tendon under the coracoacromial arch.20,78,83 Medial instability also causes pain, especially with internal rotation, and can be exacerbated by anatomic factors such as a shallow groove, presence of a supracondylar ridge, or small medial opening angle, as well as by pathologic conditions such as subscapularis tears and pulley lesions which allow the LHB tendon to escape from the groove.
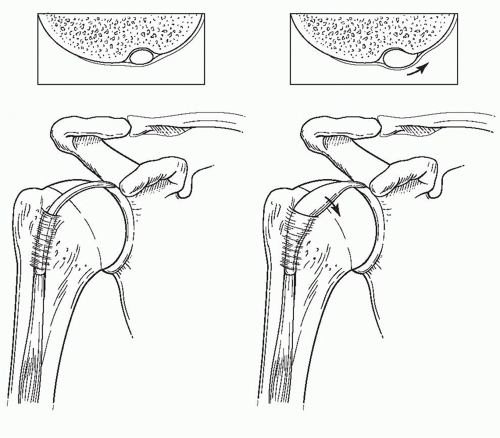
Although uncommon, primary disease of the biceps tendon without associated shoulder pathology has been described, occurring usually within the bicipital groove and with idiopathic disease accounting for 43% of primary biceps tendinitis.26 In many cases, the term “tendinitis” is a misnomer, as inflammatory changes are likely to be absent. Biceps tendon pathology within the bicipital groove at the level of the transverse humeral ligament has been likened to de Quervain’s stenosing tenosynovitis,26,27,63,75,80,92 with hemorrhagic changes of the sheath apparent at surgery and inflammatory exudates present between the layers of the sheath.63 Microscopically, a round-cell infiltration into the tendon substance with edema and fiber degeneration has been described.63,77 The tendon may appear dusky and swollen in the acute, painful stage, with the intra-articular portion taking on an “hourglass” appearance as it is mechanically blocked from entering the bicipital groove with shoulder flexion (Fig. 5-1).13 Later, the tendon may appear thin and frayed, and can form adhesions within the groove, leading to pain and stiffness with motion, or it may spontaneously rupture, leading to a sudden resolution of symptoms, which is diagnostic of biceps pathology as a cause of the patient’s shoulder pain.
Lesions of the biceps tendon are well known to co-occur with massive rotator cuff tears,10,11,13,28,49,77,79,100,108,122 and include tendinitis, joint entrapment, subluxation, and frank dislocation. Degenerative changes in the biceps tendon were found by Petersson90 to occur in older individuals, with no degenerative changes noted in any individuals under the age of 60 years in his dissection of 151 shoulders in 76 cadavers. Chen et al.21 demonstrated macroscopic biceps tendon abnormalities in association with rotator cuff tears, including all cases of chronic tears, and similar conclusions have been drawn based on cadaveric studies.117 Rotator cuff disease, primarily a disease of older individuals, was shown by Murthi et al.77 to show a strong association with biceps tendon pathology based on a prospective arthroscopic evaluation of the LHB tendon in 200 patients undergoing rotator cuff surgery.
Instability of the biceps tendon can also lead to pain, as the tendon transiently subluxes, or, more commonly, becomes
permanently displaced medially out of the groove. The tendon may dislocate superiorly due to loss of the coracohumeral ligament (CHL) and sling (type I), become unstable at the entrance to the bicipital groove due to a lesion of the superior subscapularis tendon (type II), or (Fig. 5-2) demonstrate subluxation due to a lesser tuberosity malunion or nonunion (type III).46 Loss of soft-tissue restraints due to rotator cuff tears has been shown to result in LHB instability,19,46,90,123,124 especially at the rotator interval,19,22,23,46,48,123,124 with up to 20% of all rotator cuff tears being associated with a dislocated LHB tendon.111 Depending on the depth of tearing of subscapularis or the pattern of tearing of supraspinatus and the biceps sling structures, the tendon may be found to lie over or under subscapularis90 (Fig. 5-3). Walch et al.124 found that 19 of 116 cases of rotator cuff tears were associated with “hidden” lesions of the rotator interval affecting the anterior supraspinatus tendon, coracohumeral ligament, and SGHL; 14 of these hidden rotator interval lesions contained a subluxated LHB tendon.
permanently displaced medially out of the groove. The tendon may dislocate superiorly due to loss of the coracohumeral ligament (CHL) and sling (type I), become unstable at the entrance to the bicipital groove due to a lesion of the superior subscapularis tendon (type II), or (Fig. 5-2) demonstrate subluxation due to a lesser tuberosity malunion or nonunion (type III).46 Loss of soft-tissue restraints due to rotator cuff tears has been shown to result in LHB instability,19,46,90,123,124 especially at the rotator interval,19,22,23,46,48,123,124 with up to 20% of all rotator cuff tears being associated with a dislocated LHB tendon.111 Depending on the depth of tearing of subscapularis or the pattern of tearing of supraspinatus and the biceps sling structures, the tendon may be found to lie over or under subscapularis90 (Fig. 5-3). Walch et al.124 found that 19 of 116 cases of rotator cuff tears were associated with “hidden” lesions of the rotator interval affecting the anterior supraspinatus tendon, coracohumeral ligament, and SGHL; 14 of these hidden rotator interval lesions contained a subluxated LHB tendon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree