Abstract
The reestablishment of communication is one of the main goals for patients with disorders of consciousness (DOC). It is now established that many DOC patients retain the ability to process stimuli of varying complexity even in the absence of behavioural response. Motor impairment, fatigue, attention disorders might contribute to the difficulty of communication in this population. Brain-computer interfaces (BCI) might be helpful in restoring some communication ability in these patients. After a definition of the different disorders of consciousness that might benefit from BCI, brain markers able to detect cognitive processes and awareness in the absence of behavioural manifestation are described. Can these markers be willfully modulated and used to restore communication in DOC patients? In order to answer this question, three paradigmatic articles using either functional imaging or electrophysiology are critically analysed with regard to clinical applications. It appears that the use of fMRI is limited from a clinical point of view, whereas the EEG seems more feasible with possible BCI applications at the patient’s bedside. However, at this stage, several limitations are pointed out: the lack of awareness in itself, the lack of sensitivity of the technique, atypical pattern of brain activity in brain damaged patients. The challenge is now to select the best candidates, to improve the efficiency, portability and cost of these techniques. Although this innovative technology may concern a minority of DOC patients, it might offer the possibility to restore or improve communication to heavily disabled patients and meanwhile detect a signature of awareness.
1
General background
Consider a patient left unresponsive after a dramatic accident and for whom clinicians have to decide about his cognitive status, the most appropriate health care, such as consent to interventions or withdrawal of life support, or more basically daily life situations (switch the music or television on or off…). Depending on the level of consciousness alteration, interactions with the patient may be simply not possible and these decisions will be the responsibility of third parties. This raises a number of major ethical issues: who holds responsibilities, role of previously expressed wishes… (see ).
It should also be considered that residual cognitive processes or even awareness of self and environment are preserved, or have reappeared but remain inaccessible because of motor impairment, vigilance fluctuation, or insufficient attention/work load. Beyond the assessment of consciousness, one important goal in clinical practice is the establishment of at least a yes/no code in order to restore basic communication with these patients.
This illustrates the need for methods of assessing cognitive or mental states, monitoring vigilance, attention, awareness, arousal, workload… Brain signals furnish direct measures that can contribute to the optimization of these assessments, complementing classical behavioral or peripheral physiological observations. Although this idea might seem obvious, online applications aimed at communicating with patients have only recently been possible, thanks to the latest development of brain-computer interfaces (BCI).
2
Assessing consciousness disorders
2.1
Defining consciousness
It is important to differentiate, on the one side, the level of consciousness that can vary e.g. from deep sleep to wakefulness and, on the other side, the content of consciousness with two main aspects: self-awareness and awareness of the environment . Many types of information can access consciousness, from low-level sensory stimulations to high-level abstract representations. Recent experiments suggest that to reach consciousness, the neural representation of the information should be previously amplified, propagated across a large distributed network of mutually connected cortical and subcortical structures . This is the basis of the global neuronal workspace theory .
2.2
Current nosology and clinical assessment in disorders of consciousness
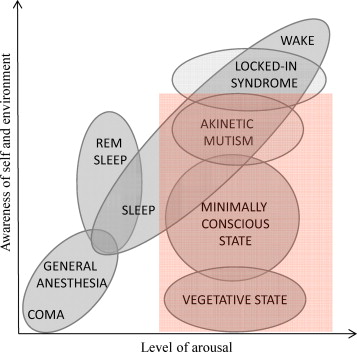
The current nosology of DOC after severe brain injury is based on the respective alteration of wakefulness and awareness (see Fig. 1 ). Comatose state is defined by the absence of both wakefulness and awareness ; vegetative state (VS), recently renamed “unresponsive wakefulness syndrome” (UWS), is a singular condition characterized by a dissociation between the presence of wakefulness and the absence of awareness ; minimally conscious state (MCS) has been defined to diagnose patients with severely altered consciousness in whom minimal but definite – i.e. inconstant but reproducible – evidence of self or environmental awareness can be demonstrated . Akinetic mutism is considered by some authors as a subcategory of MCS . Although some other authors recommend avoiding this term, in our view, akinetic mutism appears as a clinical entity that should be differentiated from other disorders of consciousness. This syndrome has been described after a lesion of the posterior mesencephalon , the diencephalon or the bilateral anterior cingulate and is characterized by a lack of initiation or motivation with at least partially preserved awakening and awareness. The core features of this syndrome are the limitation of spontaneous and voluntary movements and speech, enhanced motor and/or speech production under solicitation, preserved movement and eye fixation. This situation could result from a disruption of some executive functions, especially the motivational thalamo-cortical network . Finally, the Locked-in syndrome (LIS) is a state in which all four limbs and the last cranial nerves are paralyzed but awakening and awareness are not altered . Except for complete LIS, communication with the external world is usually possible using vertical or lateral eye movement and blinking . The LIS is the consequence of a disruption of the corticospinal and corticobulbar pathways generally after an isolated lesion of the ventral portion of the pons. Degenerative diseases, like amyotrophic lateral sclerosis can also generate LIS. Recently, the concept of functional LIS has been introduced to describe patients fully awake and aware, without any possibility of behavioral manifestation but who demonstrate consistent communication abilities using adjunctive tools .
After a comatose state, cyclical eye opening or specific EEG patterns characterize the presence of wakefulness and thus, the end of coma. Patients evolve toward a vegetative state, which is most of the time transient but can be permanent especially after a widespread brain anoxia due to cardiac arrest. At this stage, one important issue is to recognize the presence of awareness in order to distinguish MCS from VS. Clinical assessment of awareness is indirect and often difficult, based on the observation of the patient’s spontaneous behaviour and his/her responses to stimuli. This is the usual way of inferring the content of consciousness – the so-called reportability – in clinical practice. In the absence of a reliable motor response to command, finalized movements, orientation to pain, intelligible verbalization, fixation and visual pursuit as well as accurate emotional reactions (cry, smile…) are the most usual signs that characterize the emergence of awareness. The differential diagnosis between VS and MCS is performed through repeated assessments by trained clinicians. Validated scales, like the Coma Recovery Scale Revised (CRS-R) , the Wessex Head injury Matrix (WHIM) and others (for a review see ) have been developed in order to standardize the evaluation of awareness and improve inter-rater reliability.
However, the detection of subtle but potentially meaningful manifestations of awareness remains difficult and hard to differentiate from purely automatic responses. Moreover, a part of subjectivity and interpretation of behavioral responses is often hard to avoid because of facing dramatic situations and family expectations. A contrario, a high frequency (up to 40%) of minimally conscious patients are erroneously diagnosed as vegetative by non-expert teams .
2.3
Neural signatures of awareness in DOC patients
In the past decades, the development of functional neuroimaging and electrophysiology raised the possibility of better exploring cognitive processes and awareness in healthy subjects and brain damaged patients with disorders of consciousness (DOC) (for a recent review see ). The principle of these approaches is to identify cognitive markers that do not require a behavioral response potentially difficult to obtain because of motor impairment or cognitive disabilities. In the following section, different paradigms based on various theoretical backgrounds are presented and discussed.
2.3.1
Resting state and the mesocircuit signature
Resting state cerebral perfusion or metabolism, as assessed by single photon emission computed tomography (SPECT) or positron emission tomography (PET), has been shown to gradually increase from brain death, VS, MCS to normal consciousness . Some regions appear of particular importance in awareness processes, such as the anterior forebrain mesocircuit . This network involves the central thalamus, the globus pallidus, the striatum, the pre-frontal cortex, the anterior cingulate, the posterior parietal cortex through long range cortico-cortical pathways and within cortico-striatopallidal-thalamo-cortical loop connections. Using PET imaging, some authors have investigated whether the recording of cerebral activity at rest within critical areas of this network could increase the sensitivity to detect awareness in patients with DOC as compared to a gold standard (usually clinical scales) . Using functional magnetic resonance imaging (fMRI), other authors have investigated the connectivity in the brain’s default-mode network, which is thought to be involved in self-awareness . These interesting approaches critically depend on the specificity of brain activations associated with conscious processes. Another difficulty is the reliability of the gold standard. For instance, if the mesocircuit is at work but the patient is considered as vegetative by the gold standard (and vice-versa), which test should be trust?
2.3.2
Task-related functional neuroimaging
Functional imaging studies have investigated the brain response to different tasks in patients with DOC, such as presentation of pictures of familiar faces ; noxious somatosensory stimuli ; simple and more complex auditory stimuli ; patient’s own name , hierarchical speech processing tasks . These studies have shown that VS patients activate the primary sensory cortices when exposed to the task, but fail to sufficiently activate higher order associative cortices. Functional connections between residual activated regions are also impaired, suggesting that isolated preserved brain areas, disconnected from the other parts of the brain, preclude awareness processes. When the same tasks were applied to MCS patients, a more widespread activation was generally observed as compared to vegetative patients . Moreover, in MCS patients, activation included associative areas and a more efficient cortico-cortical functional connectivity. It should be noted that in the series reported by Coleman et al., 2009 , two vegetative patients showed a pattern of activation related to speech processing similar to the one observed in minimally conscious patients. This raised the question as to whether these two patients were truly vegetative. Is it the neuroimaging findings that were insufficiently specific to awareness or is it the classification based on behavioral assessment that had to be reconsidered?
In 2006, Owen et al. introduced a new fMRI paradigm with two imagery tasks: imaging playing tennis “tennis task” vs imaging walking in a familiar place “spatial navigation task”. This paradigm requires that the subject attend to stimuli, understands verbal instructions, retain the information in working memory and responds to them through a modulation of his/her brain activity. Critically, as demonstrated in a group of healthy subjects, the supplementary motor area (SMA) was specifically and consistently activated during the tennis task whereas parahippocampal cortex activation was specifically and consistently associated with the spatial navigation task. The complexity of the tasks, the higher order cognitive processes involved and the specific patterns of brain areas related to each task allowed the authors to consider that the activity in these brain regions (when observed in response to the appropriate command) could be used as a neural marker of awareness. Using this technique, a first emblematic patient who fulfilled the clinical criteria for the vegetative state showed reliable activations in the expected regions for each task, respectively. This study offered the most convincing evidence that awareness may remain undetected using clinical assessments even by experienced teams.
2.3.3
Electrophysiology and evoked potentials: from passive to active paradigms
Long-latency event-related potentials (ERPs), namely the Mismatch negativity (MMN) and the P300, have been recorded in DOC patients, following the idea that these cortical markers of cognitive brain functions could be useful in detecting patients prone to regain awareness (for a review see ). The MMN, an indicator of pre-attentive sensory memory is obtained in passive oddball paradigm; i.e. by any discriminable change (deviant) in some repetitive aspect of sensory stimulation (standard) . MMN proved to be a remarkable early marker for awakening prognosis , but it is not a marker of awareness per se. The P300 (or P3) wave is a positive component of the EPRs that is elicited when the patient is explicitly asked to count the deviants (active paradigms). It can also be observed without requesting the active participation of the patient in oddball paradigms incremented with unexpected salient stimuli (called novel stimuli, or Novels), like for instance the subject’s own name (SON). At least two subcomponents of the novelty P3 have been described:
- •
the early central P3a has been associated with alerting processes governing the direction of attentional move ;
- •
the parietal P3b has been associated with stimulus categorization, and for some authors this subcomponent is a marker of conscious perception .
Remarkably, when the oddball paradigm using the subject’s own name as a novel was applied to patients with DOC, a P3b has been recorded in 2 patients, one considered as VS and the other as MCS (see Fig. 2 ).
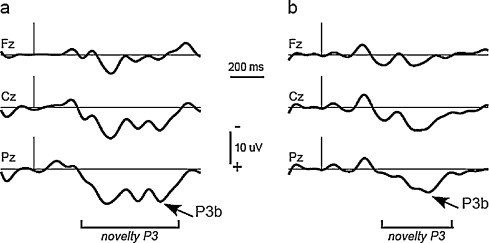
In another study using auditory evoked potentials to the patient’s own name and to 7 other equiprobable first names in severe brain damaged patients, a P3 component was observed in response to the patient’s name in all patients with Locked-in syndrome, in all MCS patients, and in 3 out of 5 patients in a VS . This first name paradigm has been used in active conditions, where the patients were instructed to count the occurrences of their own names, or of other names. Larger P3s were observed in response to target names in MCS patients, but not in VS patients . In these studies, it should be noted that the latency of the P3 wave was significantly delayed for MCS and VS patients compared with healthy volunteers. These results give other evidence of a discrepancy between clinical reportability of awareness and a direct brain signature –the P3 in these cases.
To further detect possible conscious processing in patients with DOC, Naccache et al. introduced an original active auditory paradigm . With this so-called “local–global” paradigm, an MMN is automatically elicited by changes in pitch that are local in time, whereas a change in sound sequence that appears across several seconds and is designed as a target elicits a parietal P300. The P3 is thought to only be present when subjects consciously perceive this global rule violation.
2.3.4
Global neuronal workspace theory and brain markers
According to the global neuronal workspace theory (see ) and Information Integration Theory , brain markers of consciousness should fulfill the following criteria: long distance synchrony between critical hubs of the network, signal complexity, re-entrant top-down processing, and global integration of brain signals. Using electroencephalography (EEG, ERP, MEG), conscious stimuli compared to non-conscious stimuli induce a late increase around 300 ms (including the P3 wave), gamma power and long range beta and gamma synchrony . Several recent studies have tested the validity of such markers in patients with DOC using the EEG to measure long distance cortical information sharing or the quantification of complexity .
All together, these studies demonstrate that electrophysiology and brain imaging can provide direct assessment of brain functioning in patients with DOC and may detect awareness in patients clinically considered in a vegetative state. The small but significant minority of DOC patients unable to produce any consistent behavior of awareness but who retain most of their higher cognitive functions are of course good candidates for BCI since this technological support can provide a unique mean to communicate. BCI may also improve the reliability and consistency of communication in other categories of DOC patients, and LIS.
2
Assessing consciousness disorders
2.1
Defining consciousness
It is important to differentiate, on the one side, the level of consciousness that can vary e.g. from deep sleep to wakefulness and, on the other side, the content of consciousness with two main aspects: self-awareness and awareness of the environment . Many types of information can access consciousness, from low-level sensory stimulations to high-level abstract representations. Recent experiments suggest that to reach consciousness, the neural representation of the information should be previously amplified, propagated across a large distributed network of mutually connected cortical and subcortical structures . This is the basis of the global neuronal workspace theory .
2.2
Current nosology and clinical assessment in disorders of consciousness
The current nosology of DOC after severe brain injury is based on the respective alteration of wakefulness and awareness (see Fig. 1 ). Comatose state is defined by the absence of both wakefulness and awareness ; vegetative state (VS), recently renamed “unresponsive wakefulness syndrome” (UWS), is a singular condition characterized by a dissociation between the presence of wakefulness and the absence of awareness ; minimally conscious state (MCS) has been defined to diagnose patients with severely altered consciousness in whom minimal but definite – i.e. inconstant but reproducible – evidence of self or environmental awareness can be demonstrated . Akinetic mutism is considered by some authors as a subcategory of MCS . Although some other authors recommend avoiding this term, in our view, akinetic mutism appears as a clinical entity that should be differentiated from other disorders of consciousness. This syndrome has been described after a lesion of the posterior mesencephalon , the diencephalon or the bilateral anterior cingulate and is characterized by a lack of initiation or motivation with at least partially preserved awakening and awareness. The core features of this syndrome are the limitation of spontaneous and voluntary movements and speech, enhanced motor and/or speech production under solicitation, preserved movement and eye fixation. This situation could result from a disruption of some executive functions, especially the motivational thalamo-cortical network . Finally, the Locked-in syndrome (LIS) is a state in which all four limbs and the last cranial nerves are paralyzed but awakening and awareness are not altered . Except for complete LIS, communication with the external world is usually possible using vertical or lateral eye movement and blinking . The LIS is the consequence of a disruption of the corticospinal and corticobulbar pathways generally after an isolated lesion of the ventral portion of the pons. Degenerative diseases, like amyotrophic lateral sclerosis can also generate LIS. Recently, the concept of functional LIS has been introduced to describe patients fully awake and aware, without any possibility of behavioral manifestation but who demonstrate consistent communication abilities using adjunctive tools .








