Bankart Repair and Inferior Capsular Shift
Theodore A. Blaine
Andrew Green
Jennie Garver
Louis U. Bigliani
DEFINITION
Glenohumeral instability is caused by a disruption of the normal stabilizing anatomic structures of the shoulder, leading to recurrent dislocation or subluxation of the glenohumeral joint.
ANATOMY
Glenohumeral stability depends on the integrity of static and dynamic components.4
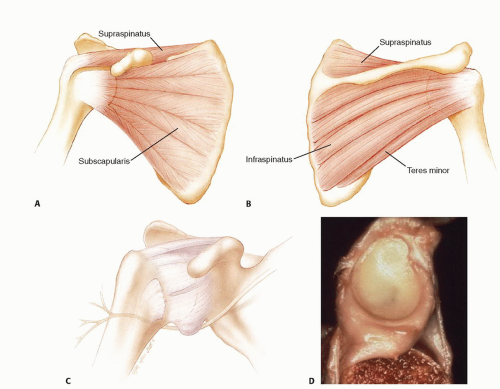
Dynamic stabilizers include the rotator cuff muscles, which provide a concavity compression effect, the scapular stabilizers, and the long head of the biceps tendon, which may contribute to anterior stability when the arm is in an abducted and externally rotated position (FIG 1A,B).
Static stabilizers consist of the bony and articular anatomy of the glenoid and humeral head, the negative intra-articular pressure supplied by the intact glenohumeral capsule, and the capsule-labral complex, which includes the glenoid labrum and the superior, middle, and inferior glenohumeral ligaments (IGHLs) (FIG 1C).
The glenoid labrum plays an important role in deepening the glenoid socket and as an attachment site for the glenohumeral ligaments (FIG 1D).
The superior glenohumeral ligament (SGHL) is located within the rotator interval and prevents inferior and posterior subluxation of the humeral head with the arm in an adducted and neutral or internally rotated position.
The middle glenohumeral ligament (MGHL) has a variable attachment site into the glenoid labrum, glenoid neck, and biceps tendon origin on the glenoid side. The MGHL is important in resisting anterior subluxation of the humeral head in the middle range of shoulder abduction (45 degrees).
The primary restraint to anterior inferior translation of the humeral head in 90 degrees of abduction and external rotation is the anterior band of the IGHL.
PATHOGENESIS
Glenohumeral instability (subluxation or dislocation) occurs when the static or dynamic stabilizers of the glenohumeral joint are disrupted.
Recurrent major trauma and/or repetitive microtrauma result in substantial deformation to the IGHL, producing subsequent episodes of symptomatic subluxation.
Biomechanical studies of this ligament have demonstrated that failure typically occurs at the glenoid insertion (40%), followed by the ligament substance (35%) and the humeral attachment (25%). Significant capsular stretching can occur (23% to 34%) before failure.
A wide range of capsulolabral pathology has been identified during arthroscopic examination after acute anterior dislocation, including anterior labral tears, superior labral tears, anterior capsule insufficiency, and humeral avulsion of the glenohumeral ligaments (HAGL lesion).11
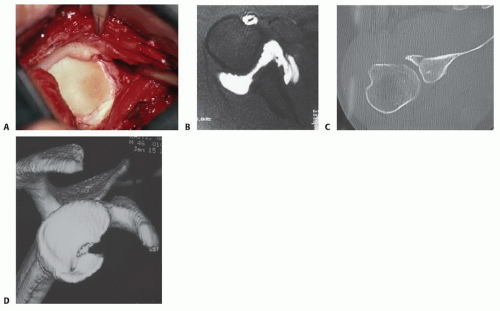
The “essential anatomic defect,” or Bankart lesion, first described by British pathologist A. Blundell Bankart in 1923, describes an avulsion of the anterior labrum and anterior band of the IGHL from the anteroinferior glenoid, typically as a result of a traumatic anterior shoulder dislocation (FIG 2A).
The Bankart lesion is present in up to 87% of shoulders undergoing arthroscopic examination after an acute anterior dislocation.15
The “essential” nature of the Bankart lesion has been challenged because a simulated Bankart lesion without capsular stretching does not lead to significant increases in glenohumeral translation.
The labrum may also be avulsed from the glenoid rim as part of a sleeve of tissue that includes glenoid periosteum (anterior labral periosteal sleeve avulsion [ALPSA]) (FIG 2B).23 In these cases, the tissue displaces medially and may heal to the medial glenoid neck, with subsequent instability if left uncorrected.
Osseous fracture of the anterior inferior glenoid rim (“bony Bankart” lesion) or more subtle attritional changes or glenoid wear may contribute to instability as well (FIG 2C).
NATURAL HISTORY
The incidence of glenohumeral instability has been estimated at 8.2 to 23.9 per 100,000 person-years.32
The incidence in at-risk populations is significantly (military population, 1.69 per 1000 person-years; NCAA athletes, 0.12 injuries/1000 athletic exposures).25
Overhead athletes are prone to atraumatic microtrauma, as their motion in the abducted, externally rotated position puts stress on the capsulolabral structures. Contact athletes (football players and wrestlers) have the highest incidence of shoulder dislocations as compared to other sports.
The rate of redislocation following nonoperative treatment of a traumatic first-time dislocation depends on the patient’s age, gender, and activity level but may be as high as 92% in the young, active male population.19,25,34 The rate decreases substantially with increasing age at the time of initial dislocation.16
PATIENT HISTORY AND PHYSICAL FINDINGS
Evaluation of the patient with suspected instability begins with a thorough history.
Arm dominance, nature of dislocation (direction, traumatic or atraumatic), and past history of injuries should be elicited.
Traumatic causes of instability should be determined as these are more likely to be associated with Bankart lesions. A history of atraumatic or voluntary dislocations should also be sought as this may be an indication of generalized ligamentous laxity or multidirectional instability.
The character of the problem should be elicited.
Does the patient complain of pain or instability?
Does the shoulder subluxate or dislocate?
What arm positions reproduce symptoms?
Any prior treatments (physical therapy, training modifications, medication, and surgery) should be noted.
Physical examination should include assessment of both shoulders.
Inspection should be performed to identify any skin incisions; evidence of wasting in the deltoid, rotator cuff, or periscapular musculature; and gross evidence of laxity, including sulcus signs or signs of generalized ligamentous laxity.
Palpation is performed to identify point tenderness: Anterior joint line tenderness may be present in acute anterior dislocations; subacromial tenderness may be present with impingement secondary to subtle instability.
Active and passive motion tests are an important part of the instability examination. Significant variations in motion are encountered in throwing athletes, with increased external rotation and decreased internal rotation common in the affected shoulder.
Provocative testing is perhaps the most important aspect in the clinical evaluation of shoulder instability.
Anterior translation and posterior translation are graded (Table 1) with the patient supine as well as with an anterior or posterior load and shift test, although this test is performed only in the anesthetized patient.
In the awake patient, signs of instability can be more subtle.
Glenohumeral translation with patient seated and arm at the side is assessed to determine underlying laxity in the affected shoulder and compared with the opposite side.
Table 1 Grading of Anterior or Posterior Translation with Load-and-Shift Maneuver
Anteroposterior Translation Grading Scheme
Grade 0
Normal glenohumeral translation
Grade 1+
Humeral head translation up to glenoid rim
Grade 2+
Humeral head translation over glenoid rim with spontaneous reduction once force withdrawn
Grade 3+
Humeral head translation over glenoid rim with locking
Table 2 Grading of Inferior Translation or Sulcus Sign
Sulcus Test Grading Scheme
Grade 1
Acromiohumeral interval <1 cm
Grade 2
Acromiohumeral interval 1-2 cm
Grade 3
Acromiohumeral interval >2 cm
The apprehension test is routinely performed on a supine patient with the arm abducted, extended, and externally rotated. A sensation of impending subluxation or dislocation in the patient is diagnostic of instability. Pain is less specific and may instead indicate internal impingement of the articular surface of the rotator cuff or functional impingement of the bursal side of the rotator cuff on a prominent coracoacromial ligament.
Relief of apprehension with application of a posteriorly directed force on the humeral head by the examiner (Jobe relocation test) suggests an unstable shoulder.
The sulcus sign, performed by applying inferior traction in a seated patient with the arm at the side, is often elicited in patients with inferior or multidirectional instability (Table 2).
Subscapularis integrity and strength should be evaluated in patients with glenohumeral instability, particularly in those who have had prior surgery for instability.
Inability to press the hand to the belly with the elbow positioned anterior to the body is a positive belly press test and indicates subscapularis muscle weakness or tear.
Inability to lift the hand from the back is a positive lift-off test and indicates subscapularis muscle weakness or tear.
IMAGING AND OTHER DIAGNOSTIC STUDIES
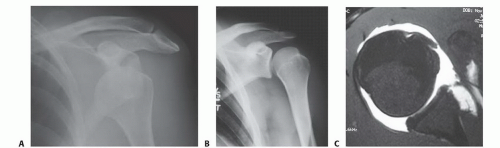
Radiographs include anteroposterior (AP), lateral, and axillary views (FIG 3A,B).
The axillary view is particularly important for assessing anterior glenoid rim defects.
The Hill-Sachs lesion of the posterosuperior humeral head is best seen on the AP internal rotation or Stryker notch views.
CT scan is not necessary in all cases but may be helpful in identifying patients with bony defects. Sagittal cuts and 3-D reconstructions are useful for quantifying the extent of glenoid bone loss (see FIG 2C,D).
Magnetic resonance imaging (MRI) scan is not necessary in all cases but can be useful in identifying labral lesions as well as concomitant rotator cuff tears (FIG 3C) or nondisplaced tuberosity fractures, which are more commonly seen in dislocations in patients older than 50 years of age.
MRI arthrogram is more sensitive in identifying labral pathology and may be necessary when superior or posterior labral pathology is suspected.
DIFFERENTIAL DIAGNOSIS
External impingement, subacromial bursitis, rotator cuff tendinitis
Internal impingement
SLAP (superior labral anterior to posterior tear)
Voluntary instability
Collagen disorder (Ehlers-Danlos syndrome, Marfan syndrome)
Subscapularis insufficiency or tear
NONOPERATIVE MANAGEMENT
After reduction of an acute dislocation, a sling is used for immobilization. The duration of immobilization has been controversial, but 3 to 6 weeks is recommended.28
Some providers recommend immobilization in a position of external rotation to better reduce the labral lesion during healing. The reported results of this approach to management vary, and many patients will not tolerate this position; a position of adduction and internal rotation therefore is more commonly used.
For treatment of acute injuries, rotational and scapular strengthening exercises of the affected shoulder are started after the initial immobilization period. The program is progressed toward normalization of strength and motion through increased resistance training.
Return to sports is allowed when the patient has a full and pain-free range of motion, normal strength, and little or no apprehension.28
For chronic and recurrent instability, strengthening is focused on the rotator cuff and scapular stabilizers as well as core strengthening of the abdominal and trunk musculature. Resistive exercises of the rotator cuff are begun with the arm in neutral below 90 degrees and are progressed gradually. Strengthening of scapular stabilizers is particularly important.
The rate of redislocation after nonoperative treatment depends on the patient’s age and activity level. In young patients participating in high-risk activities (eg, military cadets), the rate of redislocation may be as high as 92%.34
A systematic review of four studies comparing operative intervention to either rehabilitation or arthroscopic lavage without repair found that the risk of recurrent instability after repair was approximately one-fifth the risk following the other forms of treatment.6 In a meta-analysis comparing operative to nonoperative treatment for first-time dislocators, 50% of the conservatively treated patients eventually opted for surgery.25
SURGICAL MANAGEMENT
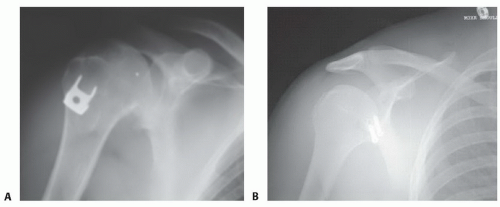
Surgical treatment options are generally categorized into anatomic and nonanatomic procedures.
Nonanatomic procedures (Putti-Platt, Magnuson-Stack) are aimed at tightening the anterior structures and preventing at-risk arm positions (ie, abduction and external rotation). These procedures have largely been abandoned after it was discovered that overtightening the anterior structures could lead to posterior subluxation and glenohumeral arthritis.14,24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree