1
English version
1.1
Introduction
The corpus callosum connects both the cerebral hemispheres and plays a vital role during their independent processing. It integrates information between both the hemispheres and is responsible for interhemispheric communication . Additionally, it coordinates the multiple areas of brain for successful motor performance The function of corpus callosum is significant during intensive bimanual coordination . One hemisphere inhibits the other through corpus callosum during unimanual motor performance. The same callosum facilitates disinhibition between the hemispheres during bimanual activity .
Developmental absence or agenesis of the corpus callosum (ACC) is a neurodevelopmental congenital disorder commonly reported in females . The absence may occur in isolation or with other conditions . The development of corpus callosum fibers gets completed by the age of 6–8 years of life . Hence, its role is also supported for handedness and laterality functions .
ACC exhibits delayed motor development, difficulty with balance, awkwardness during bimanual movement, large head size, low muscle tone, poor depth perception, reduced pain perception, sleeping difficulties, and either left or mixed handedness . It is also evident that ACC may be associated with mental retardation, diverse neurological and psychiatric symptoms with or without hyperactive disorders . Clients with ACC exhibited impairment in intelligence, cognitive-sensory-motor processing, attention, decision-making and executive functions .
The relation between stroke and ACC is unclear. Although impairment related to ACC is widely mentioned in the literature, the deficit in a poststroke patient with ACC is sparsely available . The aim of the present case report was to focus atypical motor behavior in a poststroke subject having congenital ACC. The other objective was to examine the effect of interlimb coordination based occupational therapy in poststroke subject with ACC.
1.2
Case description
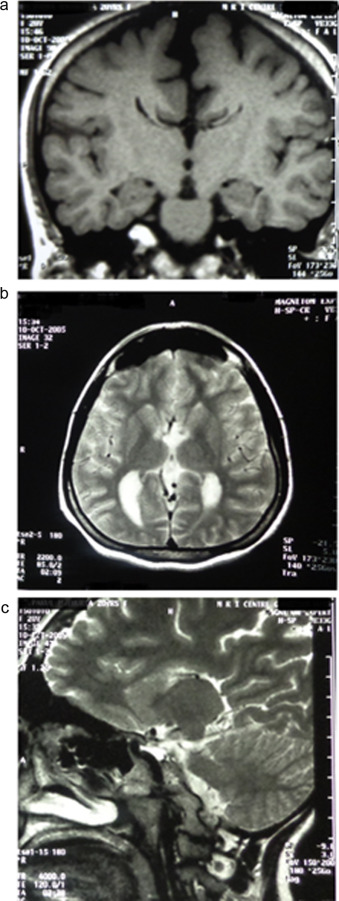
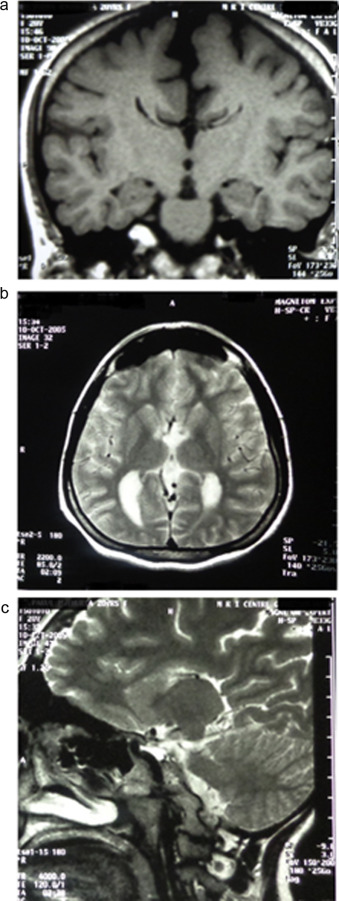
A 28-year-old female, postgraduate student had an episode of stroke. She could not stand and walk and presented with severe weakness on the right side of body. Stroke was diagnosed by a neurologist, as an acute event of cerebrovascular origin causing focal or global neurological dysfunction lasting for more than 24 hours, and confirmed by computed tomography . Computed tomography (CT) scan showed hypodensity in the left ganglionic capsular region and subcortical parietal region suggestive of ischemia along with absence of the corpus callosum ( Fig. 1 ). The subject had undergone inpatient care and standard medical management.

Prestroke, she had been facing the acute and severe episodes of migraine headache (especially during academic examinations and any other stressful situations) for few years. Her prestroke MRI revealed agenesis of corpus callosum ( Fig. 2 a–c ). She had been prescribed non-steroidal anti-inflammatory drugs for the headache. Her childhood history revealed obesity, large head size and delayed milestones. She started walking at the age of 2 years with an atypical gait pattern in form of mild scissoring and extra body weight on her toes of the feet. Her mother also informed about insignificant behavioral issues as forgetfulness, aggressiveness and irritability. The subject informed that her handwriting (dominant, right hand) quality and speed was poorer than the other classmates during the student life prior to the stroke. She had difficulty in bimanual tasks. Such tasks were either time consuming or being avoided due to poor quality of performance. However, the quality of bimanual asymmetrical tasks was better than the symmetrical tasks.
Poststroke, she had not taken any specific rehabilitation management and discontinued her studies. After many months she reported to the occupational therapy unit at study site. Her motor impairment was stabilized during the last few months. Her chief complaints were in ability to hold a pen with the affected side and impairment in performing bimanual daily tasks such as folding cloths, kneading dough, plating hair and using keyboard. The subject scrambled few words when she was made to hold the pen by the affected hand. She was preparing for a professional entrance examination to become a school teacher. She was practicing with her less-affected hand (non-dominant, left side); however, with compromised speed and quality. The difficulty in performing bimanual and writing activities was the rationale for her reporting.
Clinically, it was observed that whenever the subject moved her affected arm in any direction, her left side (less-affected) also moved reflexively in an unusual pattern. Every time she made an effort by the affected hand similar hand movements appeared on her less-affected side. For instance, while pouring water from bottle to glass by the affected upper extremity, the less-affected upper extremity passed behind the body (shoulder adduction, extension and internal rotation; elbow flexion; wrist dorsiflexion and clawing of fingers with thumb in palm). Similarly, while picking up small objects such as beads by the paretic hand the less-affected arm passed behind the body; however, there was associated wrist flexion, and hyperextension and fanning of the fingers. During taking out pegs by the affected arm the less-affected hand moved very abruptly behind the body with associated clawing (less-affected fingers) and grasping, and spreading of the fingers (less-affected) and releasing ( Video ). The amount and severity of movement and contraction on the less-affected side was dependent on the efforts made on the affected side. Further, when the subject was instructed not to move the less-affected side, her movement quality deteriorated on the affected side. On resisting the movement on less-affected side passively by the therapist or against the subject’s body, there was strong contraction of the entire limb and observable wriggling movement of the fingers on the same side. She also exhibited half open and twisted jaw towards the affected side during her motor efforts. All the atypical motor presentations on the left side (less-affected) were not present prior to the stroke. The presentations were obvious as the voluntary motor control improved on the affected side. Further, associated movements were also exhibited on the affected side (right) when the resistive movements were provided on the less-affected side (left). For instance, involuntary mass flexion response of the affected hand was observed during both resistive grasping and releasing of the less-affected hand.
1.3
Assessment and intervention
The motor recovery on the paretic side was assessed using Brunnstrom Recovery Stages (BRS) for arm and hand, and Fugl-Meyer Assessment (FMA): upper extremity and lower extremity. Minnesota Manual Dexterity Test (MMDT) and Purdue PegBoard Test (PPBT) were applied to assess dexterity and hand coordination. Only placing and one-hand prehension subtests were used for MMDT (both the sides) and PPBT (left side) as the other subtests were not possible by the subject. All the measures were reliable and valid within the acceptable range and commonly used in stroke rehabilitation studies .
Initially, her motor examination exhibited BRS stage for upper arm (BRS-A), 4 to 5; hand (BRS-H), 3 and lower limb (BRS-LL), 4. Her detailed motor examination as measured by FMA is given in Table 1 . The total FMA upper extremity score was 26 including hand score of 9. Her muscle tone ranged from 0 to 1 as assessed by Modified Ashworth scale. Clinically, her voluntary motor control for the grosser movements was fair to good while the control was poor for the fine movements. Her all hand functions were found to be poor.
| Outcome measure/items (maximum score) | Item description | Pre-score | Post-score |
|---|---|---|---|
| BRS-A | – | 4 | 5 |
| BRS-H | – | 3 | 4 |
| FMA–SSUA (36) | Sub-score upper arm (sum of FMA-I to FMA-VI) | 27 | 31 |
| FMA–SSWH (30) | Sub-score wrist and hand (sum of FMA-VII to FMA-IX) | 9 | 12 |
| FMA–TUES (66) | Total upper extremity score | 36 | 43 |
| PPBT | |||
| Left side | – | 12 | 13 |
| MMDT | |||
| Right side | – | Test could not be completed | 630 s |
| Left side | – | 75.33 s | 70.66 s |
Standard manual muscle testing (MMT) procedure was not possible for the affected side. MMT for the less-affected upper extremity demonstrated grades of 3+ in most of the shoulder and wrist muscles. All other muscles showed strength of grade 4. Her visual, auditory, perceptual, and somatosensory functions were found to be intact.
An occupational therapy program was formulated to manage the poststroke impairment and to enhance interlimb coordination between the upper limbs of the subject. The intervention protocol comprised unilateral and bilateral tasks. The activities such as lifting and reaching of pegs in different directions, palm up-down and wrist flexion extension using block, clay modelling, and picking up objects of various size and shape were given in form of unilateral movements. Bimanual activities consisted of folding cloth/newspaper, pouring water, opening and closing jar, chopping vegetables, kneading dough, washing clothes, and arranging wardrobe/refrigerator. The unilateral activities were based on Brunnstrom movement therapy while the bimanual therapy was based on motor relearning program Twenty-four therapy sessions, 1 hour each were provided for 2 months. Each activity was performed for 10 to 20 repetitions. Initially, emphasis was given on the unilateral activities. Once the subject achieved functional release of the hand, the bimanual tasks were gradually incorporated along with the unilateral activities.
Post-intervention, the changes were observed in FMA scores. The total FMA score reached to 43 from 36, upper arm FMA to 31 from 27 and wrist-hand FMA to 12 from 9. The detail scores are shown in Table 1 . Both supination and pronation components of flexor and extensor synergy respectively improved from score 1 to 2. Both the shoulder flexion and abduction control recovered from score 1 to 2. Similarly, the wrist flexion-extension improved at various ranges of the shoulder and elbow. Among hand function, only finger mass extension exhibited positive change of score 1.
However, no change was observed for the atypical motor behavior on the less-affected side. Further, no improvement was also observed for muscle tone on the affected side and muscle strength on the less-affected side.
1.4
Discussion
Corpus callosum is the only structure responsible for interhemispheric connectivity and bimanual coordination. It carries the information related to functional difference between the bilateral cortical areas. Role of corpus callosum becomes significant during asynchronous bimanual movements. Further, it inhibits the opposite hemisphere during unilateral activities . The interhemispheric inhibition transforms to disinhibition with repetitive performance of a bimanual task using the callosum. Hence, disinhibition of movements would be difficult for subject with ACC . Contrary, facilitatory motor responses are found to be same both in ACC and intact callosal subjects indicating spinal contribution . Interhemispheric inhibition facilitates complex unilateral movements and may augment recovery in a neurological insult . Although the interhemispheric synchronization is same for unimanual and bimanual tasks, it varies with the complexity of movements . The impairment related to ACC is well evident; however, the association between stroke and ACC is uncertain . The mechanism of the ischemic cerebral lesion was not clearly demonstrated; nevertheless, migraine is a risk factor for ischemia .
It is evident that subjects with ACC have great difficulty in performing complex and fast unilateral and bilateral movements. They have impairment in learning new bimanual skills . This could be the reason for the difficulty in performing various bimanual activities prestroke by the subjects of present study and the same became further challenging after the stroke. She was not able to perform significant number of daily tasks in spite of fair to good arm and hand control. The presentation validates the integrity of corpus callosum for bimanual skills and interhemispheric connectivity for hand functions . In the present study, unlike typical stroke, the subject showed 2 unusual motor behaviors in form of associated movements. Firstly, the movements were observed on the less-affected side during performance of the affected upper limb. Secondly, the associated movements appeared on the affected side even at the higher level of motor recovery. Clinically, it was noticed that these atypical movements led to exertion, bimanual/unimanual incoordination and asymmetry during task performance. Despite favorable motor recovery on the paretic side, the subject faced difficulties in all complex motor tasks. She was not independent in various self-care and household chores. For instance, performance of paper-folding, kneading and keyboard were poor. The present subject had intact visuo-perceptual and somatosensory functions; however, mild perceptual deficit in form of left hand apraxia has been reported in a recent case study . Post-intervention, it was observed that patient showed improvement in unimanual performance especially finer movements. However, bimanual performances were not satisfactory in spite of adequate motor recovery on the affected side. It was also examined that symmetrical bimanual activities were poorly performed than the asymmetrical tasks. For instance, the flour kneading was poorer than opening a bottle cap. She was not able to manage the keyboard with either of the side. Use of the mouse with the affected hand showed similar atypical motor behavior on the less-affected side as described earlier. The stroke related impairment in a subject with ACC is unclear. In a case study, ipsilateral paresis with spontaneous nystagmus after a cerebaral lesion has been reported . Hence, neurological impairments such as stroke in an individual with ACC further complicate the interhemispheric inhibition and exhibits variable motor deficits . Additionally, the corpus callosum has been found to influence cortical reorganization and associated motor outcome after stroke . Hence, the rehabilitation management for stroke subject with ACC is a challenge.
Poststroke hemiparesis subject presents with the motor behavior in form of associated or reflex reactions. Voluntary and forceful movements on the less-affected side produce uncontrolled or associated movements on the affected side. Such motor responses diminish as the voluntary motor control appears . Contrary, the associated motor response has been observed on the less-affected side during voluntary movement of the affected side in the present case study. The subject did not show any other involuntary movements, which could be attributed to the alternate neural pathways . Further, the neural fibres responsible for upper limb movements might not have developed inhibitory functional linkage with the controlateral motor cortex. It is assumed that the alternate pathways for the inhibition may develop after intense bimanual practice. Ipsilateral brain via lateral and ventral tracts indirectly has a role in bimanual movements. The fibers synchronize neuronal firing and processing . This was rationale for formulating the intervention protocol comprised of unilateral and bimanual activities. In the present study, interlimb coordination based occupational therapy was provided to enhance bimanual performance of the subject. However, in spite of improved unimanual performance on both the sides, no change was observed for the atypical movements on the less-affected side as well as for the bimanual activity. Further, the speed and quality of her handwriting did not progress up to the need. Apart from the neuropathology, the poor recovery could be attributed to long delay in taking rehabilitation management by the subject.
In a most recent study, it was concluded that mirror therapy could enhance motor performance rather than using interhemispheric interaction via corpus callosum . It is recommended that the role of mirror therapy may also be explored for the poststroke subject with ACC.
1.5
Conclusion
Atypical motor behavior was found to be present in a poststroke subject with ACC. The involuntary movements appeared on the less-affected side during performance of the affected upper limb. Such presentation is unusual in clinical practice. The management of poststroke subject with ACC is an additional challenge. Intervention for the atypical movements needs to be explored. Interlimb coordination based occupational therapy may improve motor recovery on the affected side.
Disclosure of interest
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgement
We would like to acknowledge Dr. Rakesh Lalla, Senior Resident, Department of Neurology, King George Medical University, Lucknow, India, for interpretation of the neuroimages.
2
Version française
2.1
Introduction
Le corps calleux relie les deux hémisphères cérébraux et joue un rôle vital dans le fonctionnement de leurs systèmes de traitement indépendants. Il intègre des informations entre les deux hémisphères et assure la communication interhémisphérique . En outre, il coordonne les différentes zones du cerveau, ce qui permet d’améliorer les performances motrices .
Le fonctionnement du corps calleux contribue tout particulièrement à la coordination bimanuelle intensive . Pendant une performance unimanuelle, c’est à travers le corps calleux que l’un des hémisphères inhibe l’autre ; pendant des activités bimanuelles, le même corps calleux facilite la désinhibition entre les deux hémisphères .
L’absence développementale ou l’agénésie du corps calleux (ACC) est un trouble de neurodéveloppement congénital fréquemment rapporté dans des personnes de sexe féminin . Cette absence peut avoir lieu isolément ou accompagnée d’autres pathologies . Le développement des fibres du corps calleux touche à sa fin pendant les 6 à 8 premières années de la vie . Son rôle dans la fixation de la manualité et de la latéralité est reconnu .
L’ACC est caractérisée par des retards dans le développement moteur, des difficultés d’équilibre, de la maladresse dans les mouvements bimanuels, une tête de grande taille, l’hypotonie, une mauvaise perception de la profondeur, des perturbations du sommeil et le fait d’être soit gauchère, soit ambidextre . Il est également évident que l’ACC peut aller de pair avec un retard mental, ainsi que différents symptômes neurologiques ou psychologiques avec ou sans désordres hyperactifs . Certaines patientes ont présenté des déficiences en matière d’intelligence, de traitement cognitif et sensorimoteur, de facultés attentionnelles, de prise de décision et des fonctions exécutives .
L’association entre AVC et ACC manque de clarté. Bien que les déficiences associées à l’ACC fassent l’objet de multiples citations dans la littérature, il n’existe que peu d’études ayant trait aux déficits répertoriés dans des patients post-AVC avec ACC . Le premier objectif de l’étude de cas présente consiste à repérer un comportement moteur atypique dans une patiente post-AVC congénitalement atteinte de l’ACC. Le deuxième objectif est d’examiner les effets de l’ergothérapie centrée sur la coordination des membres dans le sujet post-AVC avec ACC.
2.2
Description du cas
Une femme de 28 ans poursuivant des études de troisième cycle a eu un premier accident vasculaire cérébral (AVC). Elle ne pouvait ni se tenir debout ni marcher et le côté droit de son corps était gravement affaibli. L’AVC était diagnostiqué par un neurologue comme un événement aigu d’origine cérébrovasculaire occasionnant un dysfonctionnement neurologique focal ou global d’une durée supérieure à 24 heures et dont la survenue fut confirmée par la tomographie . En effet, une tomodensitométrie fit apparaître une forme d’hypodensité à proximité de la capsule ganglionnaire gauche et de la région sous-corticale pariétale évoquant une ischémie, ainsi que l’absence du corps calleux ( Fig. 1 ). Le sujet avait déjà bénéficie de soins en régime hospitalier et de suivi médical normal.
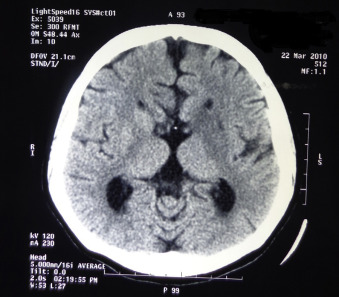
Avant l’attaque cérébrale, la patiente avait déjà eu à faire face, depuis plusieurs années et surtout pendant des examens scolaires et d’autres situations stressantes, à des épisodes aigus et sévères de migraine. Une IRM réalisé avant l’AVC avait révélé l’agénésie du corps calleux ( Fig. 2a–c ). Pour soulager ses maux de tête, on lui avait prescrit des anti-inflammatoires sans corticostéroïdes. Son enfance avait été marquée par l’obésité, la grande taille de la tête et un retard de certaines étapes de son développement. Par exemple, lorsqu’elle a commencé à marcher, à l’âge de 2 ans, le déroulement du mouvement était atypique, caractérisé par le cisaillement des jambes et le déplacement sur ses orteils du surplus de poids. Sa mère nous a également parlé de problèmes comportementaux mineurs dont des tendances à l’oubli, l’agressivité et l’irritabilité. La patiente nous a dit que dans sa vie estudiantine antérieure à l’AVC, la qualité et la vitesse de son écriture manuscrite (dominance de la main droite) étaient inférieures à celles de ses condisciples. Les tâches bimanuelles lui posaient des difficultés ; soit elles étaient chronophages, soit la patiente les évitait à cause de ses performances insatisfaisantes. Cela dit, elle réussissait mieux les tâches bimanuelles asymétriques que les tâches symétriques.
Subséquemment à l’attaque cérébrale, elle n’avait pas suivi de programme spécifique de réadaptation ; en même temps, elle a mis ses études entre parenthèses. Après plusieurs mois, elle s’est présentée à notre unité d’ergothérapie. Ses déficiences motrices se sont stabilisées assez rapidement. Elle se plaignait principalement des difficultés qu’elle éprouvait à tenir un stylo à partir du côté lésé et à exécuter des tâches bimanuelles quotidiennes dont plier du linge, pétrir la pâte, tresser ses cheveux et utiliser le clavier. Lorsqu’elle était obligée de tenir le stylo avec la main handicapée, il lui arrivait de mélanger ses mots. Elle était en train de préparer un examen d’entrée professionnel en vue de devenir maîtresse d’école. Dans cette optique, elle se servait de sa main relativement peu atteinte (non-dominance du côté gauche) mais aux dépens de la vitesse et de la qualité de son écriture manuscrite. Lorsqu’elle s’est présentée à l’unité, de telles difficultés (dans des activités bimanuelles et en écrivant) en étaient les raisons.
Cliniquement parlant, nous avons observé que dès que la patiente faisait bouger son bras handicapé, peu importe dans quel sens, la partie gauche de son corps (non lésée) bougeait également, de manière réflexive, dans une séquence inhabituelle. Chaque fois qu’elle faisait des efforts en se servant de la main lésée, des mouvements similaires de sa main gauche intervenaient. Par exemple, lorsqu’elle versait de l’eau d’une bouteille dans un verre à l’aide du membre supérieur diminué, l’autre membre supérieur est passé derrière son corps : adduction de l’épaule, extension et rotation interne ; flexion du coude ; dorsiflexion du poignet et contracture des doigts, le pouce immobilisé contre la paume. De manière similaire, lorsque la patiente a récupéré de petits objets dont des perles en se servant de sa main parétique, l’autre bras est passé de nouveau derrière son corps, geste accompagné de la flexion du poignet ainsi que l’hyperextension et la « ventilation » des doigts. Ou encore, lorsque des petites chevilles (pegs) ont été enlevées avec la main droite, la main gauche s’est abruptement déplacée derrière son corps ; les doigts non lésés se sont contractés de nouveau : il y a également eu des mouvements d’empoignade, d’écartement des doigts et de relâchement ( Vidéo ). La quantité et la sévérité des gestes et surtout des contractions émanant du côté non lésé dépendaient des efforts prodigués du côté lésé. En outre, dès qu’on demandait au sujet d’éviter de faire bouger le côté non parétique, la qualité des mouvements issus du côté parétique en était amoindrie. Plus précisément, lorsque le mouvement du côté non parétique était contrecarré soit passivement par le thérapeute, soit activement par le corps du sujet, il y avait une forte contraction du membre dans son entièreté et, toujours du même côté, une sorte de tortillement, de gigotement observable des doigts. En plus, lors de ses efforts moteurs sa mâchoire à moitié ouverte et tordue était penchée vers le côté parétique.
Les différents mouvements atypiques du côté non parétique n’avaient pas été présents avant l’AVC ; ils se mettaient en évidence alors que du côté parétique, on constatait une amélioration du contrôle volontaire de la motricité. Qui plus est, des mouvements associés émanaient du côté droit (lésé) pendant que des mouvements résistifs émanaient du côté gauche (non lésé). Par exemple, la réponse involontaire consistant en un mouvement de repliement de la main droite (parétique) était observée lors de l’empoignement résistif et du relâchement de la main gauche (non parétique).
2.3
Évaluation et intervention
La récupération de la motricité du côté parétique était évaluée en appliquant les Brunnstrom Recovery Stages (BRS) pour le bras et la main et utilisant le Fugl-Meyer Assessment (FMA) pour les extrémités supérieures et les extrémités inférieures. L’évaluation de la dextérité et de la coordination des mains s’effectuait en appliquant le Minnesota Manual Dexterity Test (MMDT) et le Purdue PegBoard Test (PPBT). En ce qui concerne le MMDT (les deux côtés) et le PPBT (côté gauche), seuls les sous-tests de placement et de préhension unimanuelle étaient réalisés, les autres sous-tests n’étant pas envisageables dans ce cas précis. Toutes les mesures étaient à la fois fiables et valides dans l’intervalle acceptable, et régulièrement utilisées dans les études de réadaptation post-AVC .
Dans un premier temps, l’évaluation de motricité BRS donnait les résultats suivants : l’avant-bras (BRS-A), stades de récupération 4 à 5 ; la main (BRS-H), 3 ; le membre inférieur (BRS-LL), 4. L’évaluation motrice détaillée en termes des mesures du FMA apparaît dans le Tableau 1 . Le score FMA global pour le membre supérieur s’élevait à 26, dont un score de 9 pour la main prise séparément. Selon l’échelle d’Ashworth modifiée, le tonus musculaire s’échelonnait de 0 à 1. En termes cliniques, la coordination motrice volontaire des mouvements grossiers était passable ou bien, alors que la coordination des mouvements fins était insuffisante. Toutes ses fonctions manuelles étaient également insuffisantes.








